What Is Tardive Dyskinesia Symptoms Causes Diagnosis Treatment And Prevention
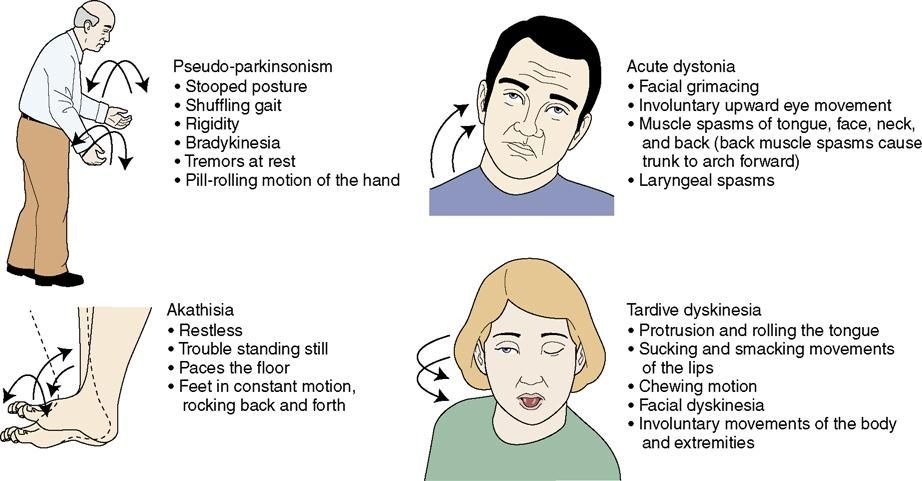
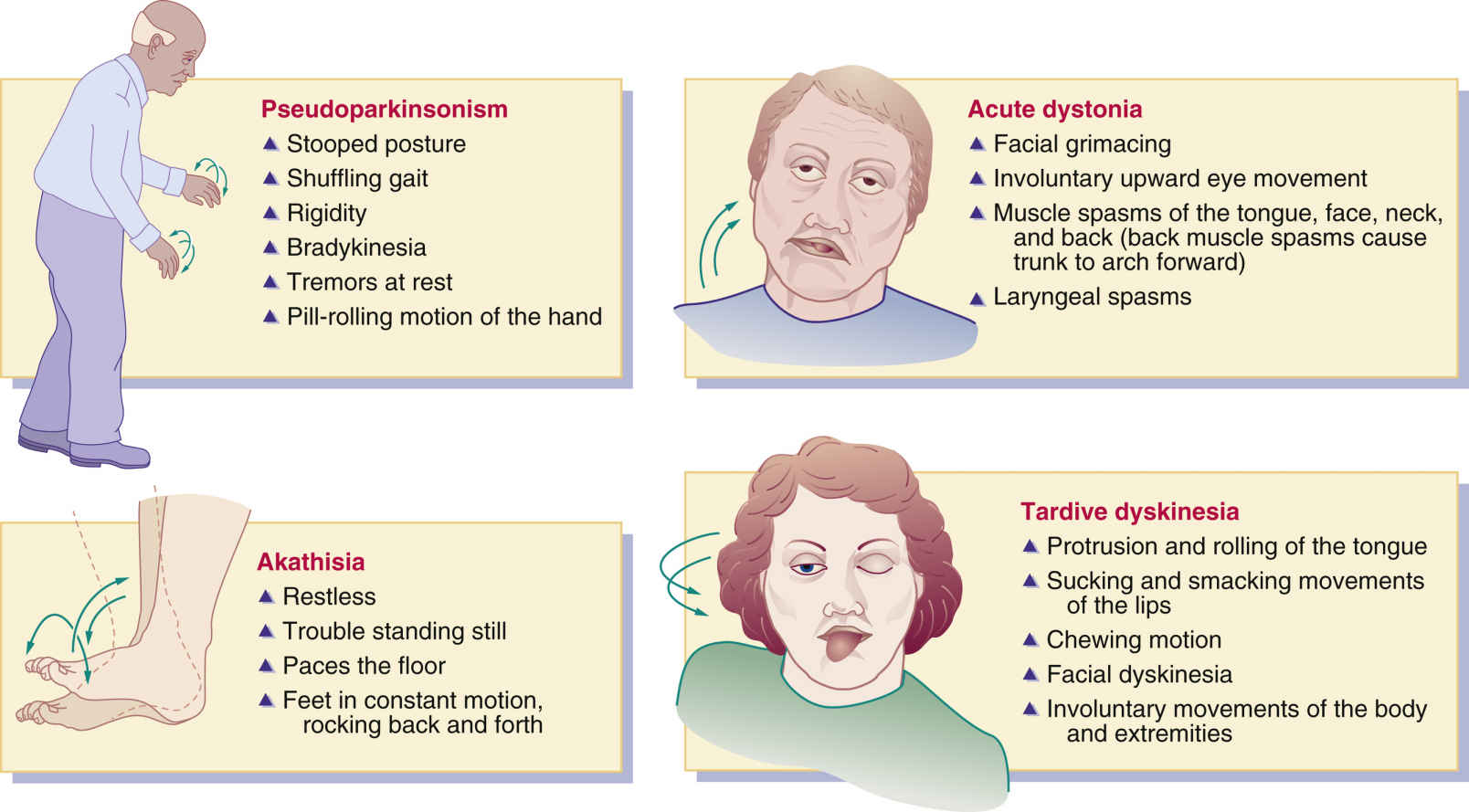
Sometimes medications used to treat serious conditions can bring on serious conditions of their own. That’s the case with tardive dyskinesia , a neurological syndrome marked by random and involuntary muscle movements that usually occur in the face, tongue, lips, or jaw.
It’s typically caused by long-term use of antipsychotic medications that block dopamine receptors. Antipsychotic medications are used to treat a number of mental illnesses and mood disorders, including schizophrenia, bipolar disorder, and depression.
Drugs Associated With Parkinsonism And Other Abnormal Involuntary Movements
There are numerous drugs and drug classes that are associated with the development of parkinsonism and other abnormal involuntary movements. Drug-induced parkinsonism is often not recognised, especially in the non-psychiatric patient , The side effect often develops within 1 month of the start of treatment, with 60% of patients developing it by this time point and 90% within 3 months .The potency of antipsychotics is defined by their ability to block the D2 receptors. Therefore, high-potency neuroleptics tend to have a greater propensity to cause extra-pyramidal side effects. However, some high-potency neuroleptics that also have anticholinergic properties are associated with fewer motor side effects. Atypical antipsychotics tend to have broader pharmacodynamic effects, and it is thought that their activity at 5HT2a receptors mediate efficacy with less need for blocking of the D2 receptors in the mesolimbic pathways and therefore in the substantia nigra.
The evidence surrounding iatrogenic dystonias is less well developed. Conventional neuroleptics are clearly implicated as are calcium channel blockers. Additionally, there are several case reports noting an association with olanzapine, carbamzaepine, lithium, imipramine, gabapentin and ziprasidone. Other dystonias are less clearly associated with iatrogenic causes.
How Do I Know If Its Parkinsons Disease Dyskinesia Or A Parkinsons Tremor
At times, it can be difficult to distinguish between Parkinson’s Disease Dyskinesia and parkinsonian tremor, particularly when the information is based primarily on history. Making the correct diagnosis is critically important, as it can profoundly alter treatment decisions. If a person with Parkinson’s is having dyskinesias that are bothersome and/or present most of the time, one option would be to reduce the levodopa dose. On the other hand, if a person with Parkinson’s is experiencing a parkinsonian tremor, one would do the exact opposite .
In short, making the wrong decision such as increasing levodopa when the person with Parkinson’s actually has bothersome dyskinesias or decreasing the dose when the person with Parkinson’s actually has tremor, can significantly compromise normal movement and quality of life.
First and foremost, your doctor must take the time to educate him/herself on your condition before making this distinction. As noted above, dyskinesias are highly irregular and cause a variety of types of movements. Parkinsonian tremor is quite different. It can affect one or more parts of the body and is characterized by regular back and forth oscillations of movement with a frequency of 5-7 cycles per second. If recorded, one would see rhythmic sinusoidal waves of to and fro movements.
Key Differences Between Tardive Dyskinesia And Parkinson’s Disease
Tardive dyskinesia and Parkinson’s disease are both movement disorders, and both have causes related to the neurotransmitter chemical called dopamine. Dopamine takes signals from the brain to certain parts of the body, regulating their function. Both diseases can be the result of medication side effects. Though Parkinson’s disease may be congenital , only in extremely rare cases is tardive dyskinesia congenital. Tardive dyskinesia is usually caused by certain drugs.
In the human brain, dopamine works on five types of dopamine receptors. It is produced in several parts of the brain. Though dopamine is available as an intravenous medication, it only acts on the sympathetic nervous system when given as a drug, producing a higher heart rate and increased blood pressure. Dopamine given as a drug, however, cannot cross the blood-brain barrier, and so cannot affect the central nervous system.
Inside the brain, dopamine is associated with the brain’s “reward” system, causing a feeling of enjoyment and increasing motivation. It is released by rewarding experiences like sexual activity, food, drugs, and even normally neutral stimuli that become associated with activation of the brain’s reward system. Drugs like cocaine, amphetamines, and nicotine directly or indirectly cause an increase of dopamine levels in one of the brain’s reward pathways, and this may help explain the addictive nature of these drugs.
Measuring Tardive Dyskinesia Against Drug Induced Parkinsonism

The symptoms of tardive dyskinesia and drug-induced parkinsonism can be remarkably similar, but an accurate diagnosis is critical when treatment for one condition may worsen the other.
Kristen M. Ward, PharmD
An accurate diagnosis for patients with either drug-induced parkinsonism or tardive dyskinesia is imperative and can minimize the impact of the symptoms on the patients’ quality of life, according to a new review of movement related disorders.
Researcher duo Kristen M. Ward, PharmD, and Leslie Citrome, MD, MPH, conducted a literature review of articles published as of the spring of 2018 that related to the presentation, pathophysiology, epidemiology, and management of DIP and TD. The pair found that there was “sparse” primary literature that supported the use of most medications for treatment of DIP and TD, except for valbenazine and deutetrabenazine.
The study authors wrote that while both DIP and TD “are stigmatizing movement disorders associated with exposure to dopamine receptor blocking agents such as antipsychotics… they differ in their pathophysiology and clinical management.”
The differences in treatment are immensely important, they said, because treatment for one may worsen the other. The treatments are different for DIP and TD and rely on accurate diagnoses.
Leslie Citrome, MD, MPH
The study authors noted that it is possible for patients to have both DIP and TD; DIP usually precedes TD. This is not currently understood clearly.
Medications And Supplements Used To Treat Tardive Dyskinesia
A number of medications and supplements have been identified that ameliorate TD symptoms.
Cholingergic Agents.
Cholinergic agents are used as muscle stimulants to diagnose myasthenia gravis and to treat glaucoma. These agents can also improve the Parkinsonian features of TD. Donepezil, a reversible acetylcholinesterase inhibitor, is currently the only cholinergic medication that has shown benefit against TD.109 Overall, however, cholinergic agents are not a widely accepted treatment for TD as sufficient evidence is lacking to suggest they are more helpful than other treatments.110
Clozapine, Quetiapine, Olanzapine, and Apomorphine.
Clozapine, a serotonin and dopamine receptor antagonist, is an atypical APD used to treat schizophrenia. Clozapine is the best current medication recommended for patients who require antipsychotics and simultaneously have TD,111 as clozapine has been reported to reverse TD symptoms.112,113 Clozapine has been linked to TD; however, the incidence is much lower compared to other atypical APDs.114 Drugs with similar mechanisms of action such as quetiapine, a weak striatal dopamine antagonist, and olanzapine, a dopamine and serotonin receptor antagonist, have also been shown to be effective in ameliorating TD symptoms.115 Apomorphine, a dopamine receptor antagonist, can be given in conjunction with L-DOPA to decrease dyskinesias.116
Tetrabenazine Analogs.
Clonazepam.
Propranolol.
Amantadine.
Branched-Chain Amino Acids.
Ginkgo Biloba.
How Are Tremors And Dyskinesia Experienced By Caregivers
People with Parkinson’s disease can experience their condition much differently than do their caregivers or spouses. “Sometimes being in the ‘off’ state looks more comfortable to the caregiver because the person is still, and can even seem kind of calm,” says Herrington. “But for the person with Parkinson’s, they experience that ‘off’ state as very uncomfortable. They may describe it as feeling trapped because they want to move but and they can’t.
“In this case,” he continues, “the person might say, ‘Look, I know I have dyskinesia, but I prefer being free to move than feeling stuck and trapped.” The caregiver, however, may feel bothered by the increased movement, he says, and think that the person is taking too much medication.
“There can be a real disconnect there between what the patient would want and what the caregiver might think is best,” says Herrington. “It’s not always the best thing to try to get rid of every last bit of dyskinesia, because the person might be less comfortable in that state.”
If Levodopa Causes Dyskinesia Then Why Should I Take It
At present, treatment with levodopa is the most effective way to relieve tremor, stiffness, and slow movement associated with Parkinson’s. In the early stage of Parkinson’s, levodopa may not be necessary and there are other medications available to treat this stage of the disease. However, as the disease progresses and symptoms begin to interfere with daily living, your doctor will prescribe levodopa.
- It typically doesn’t develop immediately – It’s important to note that there is usually a time lag of roughly 4 to 10 years from the start of treatment with levodopa to when dyskinesia emerges, and its severity will vary among different individuals.
- Younger people are at a greater risk –People who get Parkinson’s in their later years may not show signs of dyskinesia or may have only mild symptoms within their lifetime. Being diagnosed with Parkinson’s at a younger age is associated with a greater chance of developing dyskinesia.
- As with every aspect of Parkinson’s, there is variability in dyskinesias – Some do not develop dyskinesias at all. For those who do get them, not all experience them the same. Dyskinesia in its milder form may not be bothersome, and the mobility afforded by taking levodopa may be preferable to the immobility associated with not taking levodopa. People with Parkinson’s must weigh the benefits from using levodopa versus the impact of dyskinesia on their quality of life.
Is Tardive Dyskinesia A Symptom Of Parkinson’s Disease
Tardive dyskinesia is not a symptom of Parkinson’s disease. It’s a separate movement disorder caused by long-term use of anti-psychotic medications.
In addition to being a side effect of different medications, tardive dyskinesia also has its own set of symptoms. The movements associated with tardive dyskinesia tend to be more fluid in appearance compared with Parkinson’s dyskinesia.
Drugs that most often cause tardive dyskinesia include:
- Chlorpromazine
- Fluphenazine
- Haloperidol
- Perphenazine
- Prochlorperazine
- Thioridazine
Biological Basis Of Iatrogenic Movement Disorders
The biological basis of the movement disorders is complex. However, those listed above as secondary to medication are characterised by the action of drugs on central nuclei and in particular pathways and nuclei associated with the basal ganglia, a functional unit located at the base of the forebrain.
The basal ganglia have principal connections to the cortices and thalamus. Although involved in multiple functions including cognition and emotional function, it is their role in the control of involuntary movements that is relevant to this chapter. The other functions, though, are clinically important and discussed elsewhere in this book. At rest, the structures of the basal ganglia can be considered to provide a tonic inhibition of motor activity. This inhibition is released through conscious activity via an increased release of dopamine from the substantia nigra, thereby allowing voluntary control of motor activity in the necessary area.
However, cholinergic pathways elsewhere are involved in cognition, vigilance and emotional modulation and degenerate in Parkinson’s disease – while anticholinergic medication may therefore be associated with an improvement in movements, it is at the expense of deterioration in cognition in this disease, as well as in patients with psychosis, where anticholinergic medication may additionally mediate confusion and psychotic symptoms.
Whats The Cause Of Parkinsons Disease Dyskinesia
Parkinson’s Disease Dyskinesia is generally believed to be caused by disease progression and the use of levodopa medications. As Parkinson’s progresses, deteriorating dopamine brain cells have increasing difficulty in managing normal movement. Levodopa medications replace normal dopamine allowing good movement control which is less “OFF” time and more “ON” time .
Over time it may be necessary to take more frequent doses of levodopa to manage movement problems. When levodopa is administered in frequent doses , the levels in the blood vary between doses, creating “peak” and “troughs” rather than continuously replacing dopamine. This has the potential to damage dopamine receptors over the years, eventually causing Parkinson’s Disease Dyskinesia.
How Can Parkinsons Disease Dyskinesia Be Managed
Because Parkinson’s Disease Dyskinesia can become such a problem in the management of Parkinson’s and is still so poorly understood, much of the effort to deal with its complication has centered on delaying, if not actually preventing the dyskinesia altogether.
One approach has been to delay the start of levodopa for as long as possible in an attempt to delay the onset of dyskinesias. However not taking, or limiting the dose of levodopa may not allow for greater movement control in early disease and throughout treatment. Another approach to forestall starting levodopa has been to use a dopamine agonist as a first line of treatment, particularly as these agents rarely cause dyskinesia on their own.
A number of large studies have shown that early agonist therapy can delay the need for levodopa by a number of years. However, this approach has gradually become less attractive for two reasons. First, dopamine agonists carry a significant burden of side-effects on their own, including excessive daytime sleepiness, impulse control disorder and pedal edema to name a few. These side-effects can be carefully monitored, and are dose dependent, so they can be dealt with when both the person with Parkinson’s and physician are on the lookout for them.
This blog article was sponsored by Adamas Pharmaceuticals, Inc.
How Is Parkinsons Disease Dyskinesia Diagnosed
Contrary to many disorders in modern medicine, where sophisticated medical tests are required, in most instances, diagnosis of this is almost purely based on the clinical history and most importantly a physical examination. It can best be made by the well-trained eye of a movement disorder specialist.
The movements can include chorea , athetosis or dystonia . They are typically random in occurrence rather than rhythmically repetitive and can range from very mild to severe. In milder cases, they can be mistaken for normal restlessness, and it’s not unusual for a person with Parkinson’s to be totally unaware of them.
At the other end of the spectrum, Parkinson’s Disease Dyskinesia can be quite severe and can significantly interfere with activities of daily living, even affecting gait and balance. The critical point is that these dyskinesias can occur when a person with Parkinson’s needs more, not less, levodopa.
Causes And Risk Factors For Tardive Dyskinesia
Tardive dyskinesia is mainly caused by an older class of drugs used to treat psychiatric disorders. These antipsychotic medications, also called neuroleptic drugs, are generally prescribed to treat psychiatric disorders. They work by blocking dopamine receptors in the brain. Dopamine is a neurotransmitter that helps control the brain’s reward and pleasure centers. It also plays a major role in motor functioning.
It’s not clear why or how tardive dyskinesia symptoms begin, but they’re thought to be related to the chronic blocking of these receptors.
Newer antipsychotic drugs are less likely to cause the syndrome, but still may trigger symptoms.
Other drugs that can cause the problem include:
- Metoclopramide , which treats gastroparesis
- Levodopa for Parkinson’s disease
- Phenobarbitals, which treat seizures
- Phenytoin , which also treats seizures
Journal of Neurological Sciencespeople with schizophreniaantipsychotics
Tardive Dyskinesia Treatment: Surgical Options
Deep brain stimulation is a procedure where electrodes are placed in specific areas of the brain. The electrodes block the abnormal brain circuitry seen in patients with neurological conditions such as Parkinson’s disease, essential tremors, dystonia and dyskinesia.
DBS does not destroy the overactive cells, like other movement disorders treatments such as pallidotomy and thalamotomy surgeries. Rather, it temporarily blocks the abnormal signals and is a reversible process. In DBS, a lead is permanently implanted into your brain and connected to a generator, which is attached under the skin of your chest.
An alternative to making a lesion with an electrode is to use highly focused radiation. Two types of devices can be used to deliver stereotactic radiosurgery, namely the Gamma Knife® and the LINAC-Scalpel.
Wake Forest Baptist Multidisciplinary Approach
The treatment of movement disorders at Wake Forest Baptist is a collaborative effort between neurologists and neurosurgeons.
Quality of life is further enhanced by the participation of physical, occupational and speech therapists, and otolaryngologists who have special expertise in speech and swallowing difficulties.
How Does Levodopa Work In Parkinson’s Disease
Levodopa is the gold standard treatment for Parkinson’s and works by temporarily replacing dopamine in the brain. In the nervous system, dopamine is a chemical messenger released by neurons to send signals to other neurons about movement. In Parkinson’s, the dopamine-producing brain cells are lost and dopamine levels decrease, leading to Parkinson’s disease symptoms. Levodopa effectively treats motor symptoms such as tremor, bradykinesia , and muscle stiffness by crossing into the brain through what is referred to as the blood/brain barrier. It is combined in medications with carbidopa, which slows the breakdown of levodopa in the bloodstream so more medication can reach the brain. While effective at managing some symptoms, it does not slow or stop disease progression or treat non-motor symptoms like sleep issues and depression.
As Parkinson’s disease progresses, more levodopa tends to be needed in order to continue managing symptoms. Patients may experience what is referred to as “off” time, when medication wears off before it’s time for another levodopa dose. “Off” time can lead to motor fluctuations as well as the return of other symptoms.
What Causes Dyskinesia In Parkinson’s Disease
Unlike “off” time, patients typically experience dyskinesia in Parkinson’s when medications are working and other symptoms are under control. Researchers aren’t exactly sure what causes dyskinesia, but it is believed to be a side effect of long-term levodopa use and involves several different brain chemicals, including serotonin, glutamate, and dopamine.
Because levodopa is taken throughout the day, dopamine levels in the brain rise and fall. These fluctuating levels of dopamine combined with the continued loss of dopamine in the brain make it difficult to maintain regular dopamine levels, and lead to dyskinesia.
Levodopa-induced dyskinesia can sometimes be confused with Parkinson’s tremor, which is a back and forth shaking caused by the disease. In contrast, dyskinesia can look like a jerking or twisting motion. These involuntary movements can also appear as head bobbing or body swaying, depending on which part of the body is affected.
Those diagnosed with Parkinson’s at a younger age are more likely to experience dyskinesia. It’s also more common in later stages of Parkinson’s or in those who have taken levodopa for several years.
Dystonia Vs Dyskinesia In Parkinson’s Disease
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology. She is an associate professor of neurology at Tufts Medical School and medical director of the Lahey Clinic Multiple Sclerosis Center in Lexington, Massachusetts.
Dystonia and dyskinesia are movement problems that commonly occur in Parkinson’s disease . You may experience one or both of them, particularly in late-stage PD. Dystonia is muscle stiffening caused by PD, while dyskinesia is a type of muscle twisting caused by some PD medications.
Dystonia and dyskinesia can both cause distress, and they are distinguished from each other based on their visible features. They can be managed with medication or surgery, typically with a moderate improvement of symptoms.
PD is characterized by four primary symptoms:
- Resting tremor
- Postural instability
- Rigidity
While they can fluctuate in severity, the primary symptoms of PD tend to be present most of the time.
Dystonia and dyskinesia are recurrent, abrupt, and short-lived muscle movements. Not everyone who has PD experiences dystonia and dyskinesia. If they do, the symptoms they experience can be telling.
-
Affects large muscle groups
-
Smooth, repetitive movement often described as a rolling or writing motion
-
Can begin suddenly and stop after several minutes
-
Not typically painful
-
More likely to occur when PD medication effects are at their peak
Approach To Psychogenic Movement Disorders
Patients with psychogenic movement disorders, somatoform disorder, somatization disorder, hypochondriasis, hysteria, conversion disorder, malingering, Munchausen syndrome, and factitious disorders usually have manifestations that rule out TD. Nevertheless, clinicians may be tempted to consider treatment for possible TD in people who have psychiatric and psychological problems. The desire of the clinician to offer a therapeutic intervention may be intensified by the requests and demands of patients for surgery and other help.
Prudent clinicians must exercise extreme caution to avoid providing pharmacologic and surgical treatments to patients with psychogenic movement disorders. These patients are likely to experience extreme adverse effects and no beneficial effects from such treatments. In particular, surgery, including psychosurgery, is contraindicated for psychogenic movement disorders.
A tactful suggestion that stress may be contributing to the symptoms is appropriate. Typically, people who manifest psychogenic movement disorders have recently had life experiences that are stressful. The life stresses can be both positive, such as a promotion, and negative, such as the death of a loved one. Psychotherapy may then provide a more effective means of expressing the psychological distress often associated with psychogenic movement disorders. Referral to mental health professionals should always be considered.
Mechanism Of Adverse Medication Reactions
The exact mechanisms of adverse medication reactions that cause TD are not well defined. However, the blockade of dopamine receptors by dopamine antagonists is the most widely accepted theory.1 Chronic dopamine blockade caused by dopamine D2 receptor antagonists or APDs could result in an upregulation of dopamine receptor responsiveness, resulting in a compensatory supersensitivity of the receptors, especially in the basal ganglia. However, some studies suggest that D3, D4, and D5 receptors are also involved in the pathogenesis of TD.32,33 D3 and D5 receptors have a consistent positive correlation with TD, but evaluations of D4 yield inconsistent results.32,33
Anticholinergic agents are also linked to TD, and taken together with the dopamine receptor supersensitivity hypothesis, an imbalance of dopamine and acetylcholine is likely involved in TD pathogenesis.34 Evidence also suggests an imbalance of serotonin. Selective serotonin reuptake inhibitors such as fluoxetine inhibit dopamine neurons in the nigrostriatal pathway by increasing serotonin in the raphe nucleus. SSRIs act by potentiating the inhibitory effects of serotonin on dopamine production in the basal ganglia.35 This decrease in dopamine production by serotonin could contribute to the pathogenesis of TD.
Medications That Cause Tardive Dyskinesia
Home » Medications that cause Tardive Dyskinesia
While tardive dyskinesia has been associated primarily with neuroleptic drugs, other medications can cause this condition, including some medications given for digestive troubles and nasal allergies. The longer a person is on a tardive dyskinesia inducing-drug the more likely he or she is to develop tardive dyskinesia. People over age sixty-five are more likely to develop drug-induced tardive dyskinesia than younger people are. As we age, our body’s metabolism and ability to process medication changes and slows; by age sixty these changes may already be apparent.
In February 2009, the connection between tardive dyskinesia and certain medications made the news, when the FDA announced that metoclopramide would be required to carry a “black box” label warning of the risk of tardive dyskinesia with long term use. Metoclopramide is an antiemetic prescribed for gastroparesis, severe acid reflux, and other problems; it is sold under the brand names: Reglan, Octamide, and Maxolon. Patients under sixty who use this drug for three months or more run the risk of developing tardive dyskinesia; people age sixty and older are especially vulnerable and may develop tardive dyskinesia after only a month on metoclopramide.
The following overview of drugs which can cause tardive dyskinesia is by no means exhaustive. Other medications not included here can also cause tardive dyskinesia.
Dyskinesia Cause #6: Too Much Medication
Each person with Parkinson’s experiences symptoms a little differently than the next. The challenge for the physician is finding the dose and formulation of levodopa that provides the right balance of symptom relief while avoiding dyskinesia, says Todd Herrington, MD, PhD, a neurologist at Massachusetts General Hospital in Boston and an instructor in neurology at Harvard Medical School in Cambridge, Massachusetts. Too much levodopa can trigger dyskinesia and possibly make other Parkinson’s symptoms worse, he says. But if people don’t take enough medication, it can leave them feeling slow, stiff, and even trapped in their own body. So be sure to work with your doctor on the right treatment regimen for you.
What Is Dyskinesia In Parkinsons Disease
Dyskinesia is predominately a side effect of a medication called levodopa that’s used to treat Parkinson’s disease.
“To the trained eye, dyskinesias look quite different ,” says Herrington. “Dyskinesias are not rhythmic — they have a more writhing quality.”
Herrington points out that you can see an example of dyskinesia if you look at videos of Michael J. Fox. “Usually,” he says, “when is on camera, he has some dyskinesia, or extra movements that are involuntary.”
Signs And Symptoms Of Tardive Dyskinesia
As someone who lives with tardive dyskinesia , I really wish I had known its signs and symptoms when I was first diagnosed. I didn’t even know it existed! A neurological condition that develops from long-term anti-psychotic medication use, TD is a disorder that can be either temporary or chronic, which depends on a number of factors that can vary for each individual.
TD is in a class of disorders known as dyskinesias, which are broadly defined as involuntary movements. Dyskinesias are characteristic of conditions like Huntington’s and Parkinson’s diseases. However TD is unique in that it is caused by medication; put another way, you cannot develop TD unless you’ve taken one of the medications that can cause it.
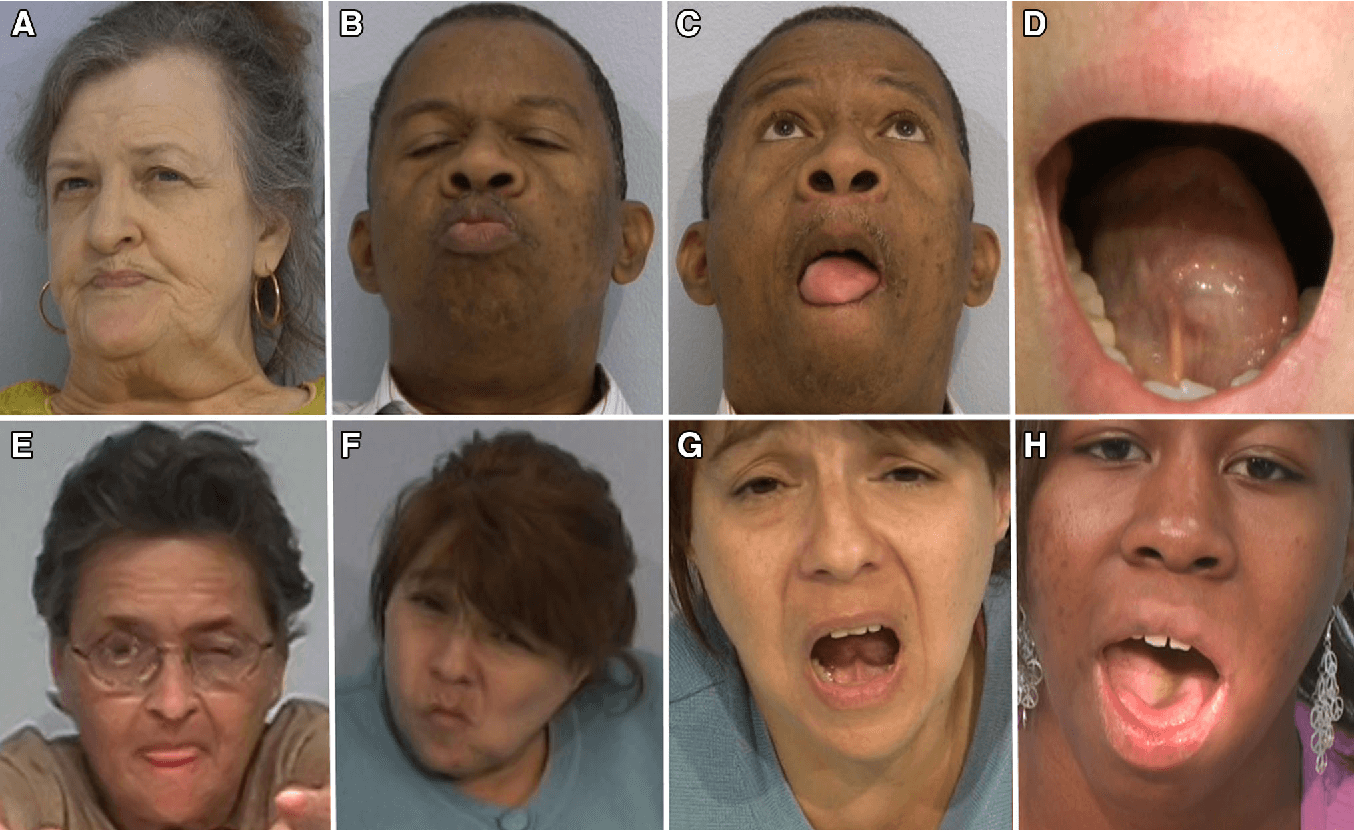
Involuntary movements, or sometimes called “tics,” is an intentionally broad and vague definition of dyskinesias. Simply put, any part of the body that moves can be affected by TD. Facial muscle tics are the most common in TD patients, specifically the tongue, lips, eyes, cheeks and jaw. My psychiatrist once described the “rule of thumb:” TD is more likely to affect muscle groups in the higher parts of the body, and likelihood of symptoms decreases as you move down toward the feet.
Gallery: 5 Signs You’re Getting Multiple Sclerosis, By an Expert
TD tics in other parts of the body vary as well. These can include :
When To See A Doctor/go To The Hospital
You should tell your doctor if you start to experience any of the effects of tardive dyskinesia. You and your doctor will need to monitor the side effects and decide whether the benefits of the medication you are taking outweigh the side effects.
While the neuroleptics that cause tardive dyskinesia are usually used to treat psychiatric disease, other medications used to treat depression, epilepsy, some GI disorders, and a variety of conditions off-label can cause it too. Sometimes the medication can be substituted for another effective treatment that doesn’t cause tardive dyskinesia.
A medication dosing adjustment or switching to another medication can be helpful. There are also treatments, including Austedo , that can reduce the symptoms of tardive dyskinesia.
Continuing Education / Review Questions
- The inter-relationships of tardive dyskinesia, parkinsonism, akathisia and tardive dystonia: the Curaçao Extrapyramidal Syndromes Study II.van Harten PN, Hoek HW, Matroos GE, Koeter M, Kahn RS. Schizophr Res. 1997 Aug 29; 26:235-42.
- Clozapine treatment for neuroleptic-induced tardive dyskinesia, parkinsonism, and chronic akathisia in schizophrenic patients.Clozapine treatment for neuroleptic-induced tardive dyskinesia, parkinsonism, and chronic akathisia in schizophrenic patients.Spivak B, Mester R, Abesgaus J, Wittenberg N, Adlersberg S, Gonen N, Weizman A. J Clin Psychiatry. 1997 Jul; 58:318-22.
- The nosology of tardive syndromes.The nosology of tardive syndromes.Frei K, Truong DD, Fahn S, Jankovic J, Hauser RA. J Neurol Sci. 2018 Jun 15; 389:10-16. Epub 2018 Feb 6.
- Review Novel antipsychotics, extrapyramidal side effects and tardive dyskinesia.Barnes TR, McPhillips MA. Int Clin Psychopharmacol. 1998 Mar; 13 Suppl 3:S49-57.
- Review Clinical relationship of extrapyramidal symptoms and tardive dyskinesia.Andrew HG. Can J Psychiatry. 1994 Nov; 39:S76-80.
What Does Tardive Dyskinesia Look Like
TD looks like different, uncontrollable movements and patterns of the limbs and face. Sometimes referred to as stereotypy, the activity can be patterned, repetitive, and rhythmic movements that can involve one or more body parts. More than 3/4 of those with TD experience oral-facial-lingual stereotypic movements .1 The Baylor College of Medicine Movement Disorders Clinic conducted a videotape review of 100 people with tardive dyskinesia. The evaluation showed that the majority experienced irregular and chaotic movements in the OFL region, including lip smacking, chewing and other tongue and mouth movements. Other areas of the body can also show signs of TD like nodding and rocking, repeated body movements like crossing and uncrossing arms and legs, and random vocalizations.
Those who experience these involuntary movements may not even realize it. Like other conditions, these stereotypies can get worse under stress. They can manifest as muscle contractions or spasms, inability to be still, facial tics, or other jerking and abnormal movements.
Understanding The Levodopa Side Effect

If you have Parkinson’s disease, there is a good chance that you’ve been, or will be taking medication containing levodopa. Levodopa is administered in combination with the drug carbidopa . This drug combination is considered standard treatment for Parkinson’s disease symptoms such as tremor, muscle stiffness, and slowness of movement. A side effect of long-term use of levodopa is dyskinesia. Below, you will learn about dyskinesia, what causes it, how it can be managed, and some basic coping strategies.
Want More Practical Articles Like This
Much more can be found in a powerful new edition of Davis Phinney Foundation’s free Every Victory Counts® manual. It’s jam-packed with up-to-date information about everything Parkinson’s, plus an expanded worksheets and resources section to help you put what you’ve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
