What Causes Parkinsons Disease
Parkinsons disease is a chronic, progressive neurological disease that currently affects about 1 million Americans. Parkinsons disease involves a small, dark-tinged portion of the brain called the substantia nigra. This is where you produce most of the dopamine your brain uses. Dopamine is the chemical messenger that transmits messages between nerves that control muscle movements as well as those involved in the brains pleasure and reward centers. As we age, its normal for cells in the substantia nigra to die. This process happens in most people at a very slow rate.
But for some people, the loss happens rapidly, which is the start of Parkinsons disease. When 50 to 60 percent of the cells are gone, you begin to see the symptoms of Parkinsons.
How Lifestyle Behaviors Influence Risk Of Parkinson Disease
People with prior incidence of traumatic brain injury and exposure to lead were shown to be at elevated risk of Parkinson disease development, with family history also found to influence risk.
History of head trauma or concussion and exposure to lead may more than double the risk of Parkinson disease , according to study findings published in Parkinsons Disease.
In determining risk of PD, the study authors said that conflicting research has been published on whether genetic factors play a role in the pathogenesis of the condition. As a result, they noted that PD is likely caused by a complex interaction between genetic and environmental risk factors, which include exposure to pesticides, toxic metals, solvents, and history of traumatic brain injury.
Identifying environmental factors that increase PD risk would allow exposure mitigation and disease prevention efforts while facilitating the experimental investigation of mechanisms and intervention opportunities, noted the study authors.
Along with prior studies that have found a positive link between rural living and the development of PD, a spatial analysis of US Medicare beneficiaries showed a concentration of PD in the Midwest and Northeast.
In addition to exposure and physical activity, participants reported on the family medical history of diagnosis of neurological disorder within each of their family members, they added.
Reference
Assessment Of Type 2 Diabetes At Baseline
Assessment of the history of type 2 diabetes was based on self-reporting and on the data of two nationwide registers. The National Hospital Discharge Register data included hospital discharge diagnoses since 1968. Data on diabetes medication were ascertained from the national Social Insurance Institution’s register on special reimbursement for antidiabetic drugs from 1964. Antidiabetic drugs prescribed by a physician are free of charge in Finland and are subject to approval of a physician of the Institution who reviews each case history. The physician confirms the diagnosis of diabetes, applying the World Health Organization criteria: one or more classic symptoms plus a fasting plasma glucose level 7.8 mmol/l or the oral glucose tolerance test 11.1 mmol/l; at least one raised plasma glucose concentration on a fasting plasma glucose level 7.8 mmol/l or the oral glucose tolerance test 11.1 mmol/l in the absence of symptoms; or treatment with a hypoglycemic drug . All patients receiving free medication were entered into a register maintained by the Social Insurance Institution. Subjects who reported having diabetes on the questionnaire, or who had a hospital discharge with a diagnosis of diabetes, or the approval for free-of-charge medication for diabetes before the baseline survey, were classified as having the history of diabetes at baseline.
What Makes Them Different
MS and Parkinsons have different causes. They usually start to affect you at different ages, too.
MS often affects people between ages 20 and 50, but children get it, too. Parkinsons usually starts at age 60 or older, but some younger adults get it.
MS is an autoimmune disease. That means your bodys immune system goes haywire for some reason. It attacks and destroys myelin. As myelin breaks down, your nerves and nerve fibers get frayed.
In Parkinsons, certain cells start to die off. Your makes less and less of a chemical called dopamine that helps control your movement. As your levels dip, you lose more of this control.
Some genes may put you at risk for Parkinsons, especially as you age. Theres a small chance that people who are exposed to toxic chemicals like pesticides or weed killers can get it, too.
These symptoms are more common if you have MS. They not usually found in Parkinsons:
- or , where you feel like the room spins around and you lose your balance
How Do People Cope With Huntingtons Disease
There are several measures that people can take to deal with the disease on a daily basis. It is important to remember that Huntingtons disease affects not only the person who has the symptoms. This disease affects the whole family in various ways, and all of them should find ways to cope.
Therapy is a big help for people who personally suffer from the disease, their caregivers, and their descendant. It is a grim outlook to feel your life decline and for your loved ones to see. Support groups and organizations also provide orientation and help to people who need it.
Another big problem, besides the psychological ones, is the mobility issues the patient faces. They may have to also go to a physiotherapist, a dietician, and even a speech therapist to deal with the progressive motor difficulties.
When the disease progresses, it may become harder for family members to take care of the patient on their own. They might have to consider additional help at home from a nurse or take them to a care facility. Specialized social agencies exist to orientate the families in those difficult processes and decisions they have to make.
Patients With Inflammatory Bowel Disease Are More Likely To Get Parkinson’s Disease Reports The Journal Of Parkinson’s Disease However The Risk Is Very Small
Amsterdam, NL Relatively new research findings indicating that the earliest stages of Parkinson’s disease may occur in the gut have been gaining traction in recent years. In a published in the Journal of Parkinson’s Disease, Tomasz Brudek, PhD, evaluates evidence for the association between inflammatory bowel disease and PD and proposes directions for future research.
“Parkinsonism is probably not just a brain disorder, but a group of diseases that may have their onset in the periphery, particularly in the gastrointestinal tract,” explained Dr. Brudek, of the Research Laboratory for Stereology and Neuroscience, and Copenhagen Center for Translational Research, Copenhagen University Hospital, Bispebjerg, and Frederiksberg Hospital, Copenhagen, Denmark. “Taken together, all data, including human, animal, and microbiome studies, suggest quite strongly that individuals with an increased tendency for peripheral inflammation have a higher risk to acquire PD. Given the potentially critical role of gut pathology in the pathogenesis of PD, there is reason to suspect that IBD may impact PD risk.”
Many epidemiological and genetic studies have found that there seems to be an increased risk of developing PD among people with IBD. The association between IBD and PD may simply be that IBD is just one type of intestinal inflammation, so it is not IBD specifically that increases the PD risk but perhaps intestinal or peripheral inflammation in a broader sense.
###
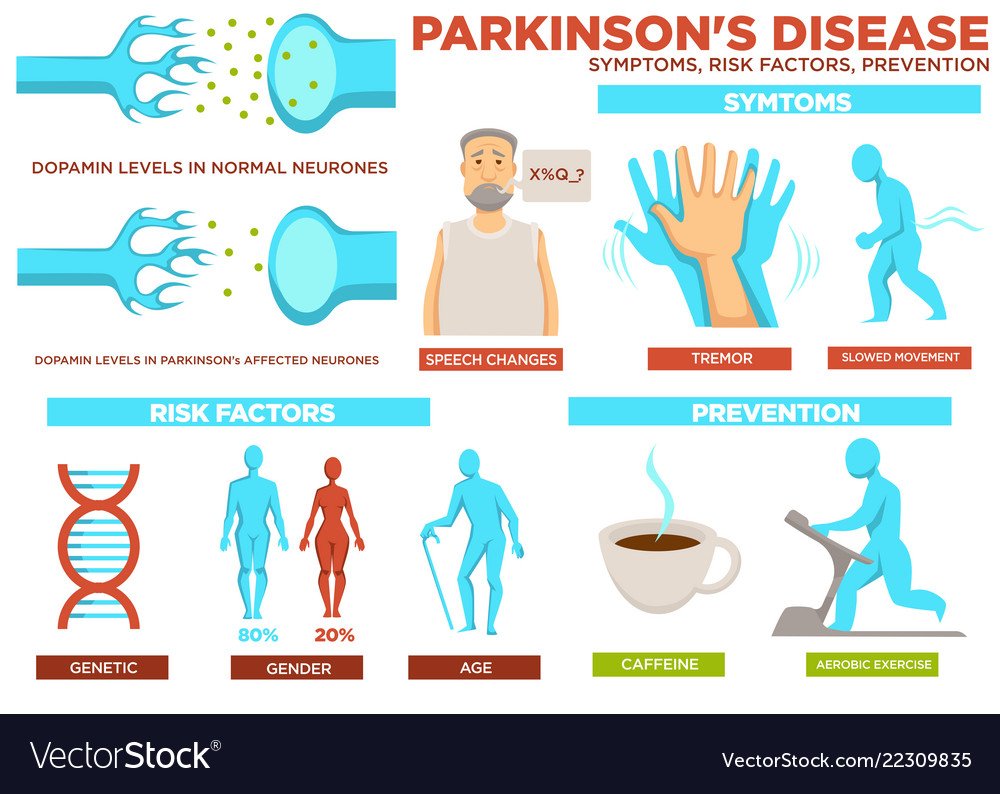
Parkinson’s Disease Risk Factors
Although a primary cause for Parkinson’s disease is yet to be identified, a number of risk factors are clearly evident.
Advancing age– Although there is the occasional case of the disease being developed as a young adult, it generally manifests itself in the middle to late years of life. The risk continues to increase the older one gets. Some researchers assume that people with Parkinson’s have neural damage from genetic or environmental factors that get worse as they age.
Sex- Males are more likely to get Parkinson’s than females. Possible reasons for this may be that males have greater exposure to other risk factors such as toxin exposure or head trauma. It has been theorised that oestrogen may have neuro-protective effects. Or, in the case of genetic predisposition, a gene predisposing someone to Parkinson’s may be linked to the X chromosome.
Family history– Having one or more close relatives with the disease increases the likelihood that you will get it, but to a minimal degree. This lends support to the idea that there is a genetic link in developing Parkinson’s.
Declining oestrogen levels– Post menopausal who do not use hormone replacement therapy are at greater risk, as are those who have had hysterectomies.
Low levels of B vitamin folate– Researchers discovered that mice with a deficiency of this vitamin developed severe Parkinson’s symptoms, while those with normal levels did not.
2002-2012©Parkinson’s Disease Information.
Risk Factors For Parkinson’s Disease
While the exact causes arent fully understood, researchers have identified characteristics that increase a persons risk of developing Parkinsons, including gender, age, race, and genetic factors. However, it is worth noting that the vast majority of cases of PD are considered idiopathic Parkinsons disease. Idiopathic means a condition that arises spontaneously or for which the cause is currently unknown. Major advances in and science are continuing to reveal more underlying causes for PD.1,2
Differences Between Alzheimers And Parkinsons
Were going to group the differences between both illnesses into different blocks and explain what each of them consists of. All of them have been extracted from two reference psychopathology manuals: Belloch, Sandn, and Ramos and the DSM-5 .
The first block of differences between Alzheimers and Parkinsons refers to their type of symptoms. Lets see what they are.
In Summary Reduce Your Stress
The most important thing we can do for our long-term health, both physical and cognitive, is to reduce the stress in our bodies. All stress physical, emotional and chemical causes inflammation and long-term damage throughout the body.
Whether youre seeking Parkinsons prevention techniques or ways to alleviate symptoms, any of the above dietary and lifestyle practices can have long-term health benefits. Drinking green tea, eating organic, local vegetables, and regular aerobic exercise all significantly reduce the long-term cumulative damage done by stress.
Learn more about health services offered at Judson by !
How Is Huntingtons Disease Diagnosed
Scientists were able to identify the affected gene as a marker for Huntingtons Disease in 1993. A diagnostic test is now available that can identify the presence of the protein huntingtin before symptoms appear. In most cases, genetic counseling is recommended after a positive diagnosis for Huntingtons Disease, as the defective chromosome is indiscriminately passed on to future generations.
Causes And Risk Factors
The cause of Parkinson’s disease is not yet known, according to the Mayo Clinic. But researchers suspect that PD is caused by a combination of genetic and environmental factors.
Parkinson’s is a disease of aging, and getting older is the most common risk factor for it, Bega told Live Science. PD is more likely to develop in people around age 60, and the risk increases with every decade after 60, he noted.
The disorder can also be diagnosed in younger people, but it’s rare. Only 5 to 10 percent of people have “early-onset” disease, meaning people are diagnosed before age 50.
Besides age, other risk factors for Parkinson’s disease include:
- Being male: Men are 1.2 to 1.5 times more likely than women to develop Parkinson’s, for reasons that are not yet known, Bega said.
- Heredity: Some genetic mutations may contribute to the development of Parkinson’s and can slightly increase a person’s risk. But most cases of the disease are not caused by inheriting genes linked to it. Only about 10 percent of people with Parkinson’s are genetically predisposed to the condition, according to the American Parkinson Disease Association.
- Exposure to toxins: Studies have shown that environmental factors such as exposure to pesticides, herbicides and drinking well water may be tied to an increased risk of Parkinson’s, but that risk is relatively small, Bega said.
- Repeated head injuries: When these injuriestrigger a loss of consciousness, they have been linked with an increased risk of P.
Visual Impairment Is More Common In Patients With Parkinson’s Disease

08/20/2021
Older people with Parkinson’s disease are significantly more likely to be visually impaired than those without the disease and poor vision may take a toll on their mental and physical health, according to an analysis of Medicare claims data.
The study of Medicare beneficiaries found that the prevalence of moderate to severe visual impairment was 1.7 percent among PD patients compared with 0.71 percent among those who don’t have the disease. Yet only 54 percent of PD patients had annual eye exams.
The study, published in the July 14 online edition of Movement Disorders, also found a higher incidence of depression, anxiety, dementia, and all-cause mortality among PD patients with visual impairment compared to those without a visual impairment.
Vision is understudied and underappreciated in PD, said lead study author Ali Hamedani, MD, a neuro-ophthalmologist and epidemiology researcher at the Perelman School of Medicine at the University of Pennsylvania.
Dr. Hamedani said that while visual problems attributable to Parkinson’s disease such as contrast sensitivity, double vision, and color discrimination are well documented, it is not clear why patients are more apt to have moderate to severe visual impairment as a result of ophthalmic disease. He said visual loss could be particularly problematic for PD patients dealing with loss of balance and mobility.
Study Examines Connection Between Diabetes Medication And Parkinsons Disease
It was first suggested in the 1960s that people with type-2 diabetes are at increased risk for developing Parkinson’s disease and when they do develop PD, its progression is faster and often more severe. This may be due, in part, to an apparent relationship in the brain between dopamine, insulin resistance, and glucose control. Insulin is not only made in the pancreas, its also present in the brain where it has been shown to impact dopamine levels.
Parkinsons is generally believed by scientists to be caused by the loss of dopamine-producing neurons. Parkinsons symptoms, such as slowness, rigidity, and tremor, typically develop after approximately 40-80% of these dopamine-producing neurons die.
Why does this matter? Currently, more than 30 million people in the United States have type-2 diabetes, and that number is growing. The lifetime is also on the rise. In light of these trends, it would be valuable to know whether any specific type-2 diabetes medications might be associated with an increased or decreased risk for developing PD.
1) Thiazolidinediones , like pioglitazone or rosiglitazone , which specifically target insulin resistance
2) Drugs, like albiglutide or dulaglutide , that mimick glucagon-like peptide-1 a hormone that promotes insulin secretion, and
3) Dipeptidyl peptidase 4 inhibitors, which increase GLP-1 levels, and lead to insulin secretion and lowering of blood sugar levels
Results
What Does This Mean?
Learn More
Q: What Happens If I Get A Cough From Covid
A: You are correct that it is important to pay attention to possible medication interactions. Cough and cold medications containing dextromethorphan, pseudoephedrine, phenylephrine, and ephedrine need to be avoided only if you are on a monoamine oxidase inhibitor such as rasagiline, selegiline or safinamide. Be sure to check the product ingredients before purchasing, and if you are unsure ask your doctor or pharmacist to clarify which brands/medications should be avoided. If you are on an MAOI, any other cold medication without these ingredients is safe for you to take. If you are not taking an MAOI, any cold medication is suitable for you.
is the list of medications to avoid in PD.
Q: I Received The Covid
A: The vaccine is certainly able to cause short term side effects of fatigue, aches and even fever. There isnt extensive data yet on how it affects PD symptoms, just anecdotal data. For some people, PD symptoms are worse in the short term. This does not mean that your PD has progressed, and I would expect that you will return to your previous baseline in the next few days. I would talk with your neurologist about your worsened tremor as well.
How Are They Alike
and Parkinsons both affect your central nervous system, which includes your and spinal cord. Thats why they both can affect how you move, , feel, and talk.
These diseases both affect your nerves. MS can break down the coating, called myelin, that surrounds and protects your nerves. In Parkinsons, nerve cells in a part of your slowly die off.
Both can start out with mild symptoms, but they get worse over time.
Common symptoms of both diseases include:
- Shaky fingers, hands, lips, or limbs
- Slurred speech thats hard for others to understand
- Numb or weak limbs that make your walk unsteady
- Loss of muscle control that often affects one side of your body at first, then later both
- Spastic limb movements that are hard to control
- Loss of or bowel control
- Poor balance
is another symptom common to both conditions.
Molecular Mechanisms And Basic Science Evidence For The Role Of Infection In Pd
Much of the evidence associating PD with infections, whether viral or bacterial, is based on obser-vational studies demonstrating increased risk to develop the disease, rather than direct evidence of infection as a singular cause. In fact, due to the complexity and multifactorial etiology of PD, identifying a single point of initiation in human PD is often impossible. For this reason, and the impossibility of interventional studies in humans involving infectious agents, the use of preclinical animal models of PD may provide the clearest evidence for or against a role of infectious agents in the etiology of PD.
Mechanistically, what might be the link between the cells of the peripheral immune system and the innate immune system in the brain? One critical component functions through recognition of MHCII; a key antigen presenting protein . MHCII is critical for the presentation of antigen to both T-cells as well as microglial cells situated in the CNS . In regard to microglia, it is interesting to note that the SNpc contains the highest microglia:neuron ratio in the brain ; perhaps leading to its particular sensitivity to inflammation .
These observations provide plausible mechanisms to explain infection as either a susceptibility or cau-sative factor for PD. The hypothesized process by which infectious agents increase susceptibility to PD is summarized in Fig. 1.
Fig. 1
Symptoms Of Parkinsons Disease
Parkinson’s disease has four main symptoms:
- Tremor in hands, arms, legs, jaw, or head
- Stiffness of the limbs and trunk
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include and other emotional changes; difficulty swallowing, chewing, and speaking; urinary problems or ; skin problems; and sleep disruptions.
Symptoms of Parkinsons and the rate of progression differ among individuals. Sometimes people dismiss early symptoms of Parkinson’s as the effects of normal aging. In most cases, there are no medical tests to definitively detect the disease, so it can be difficult to diagnose accurately.
Early symptoms of Parkinson’s disease are subtle and occur gradually. For example, affected people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly, or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinson’s. They may see that the person’s face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinson’s often develop a parkinsonian gait that includes a tendency to lean forward, small quick steps as if hurrying forward, and reduced swinging of the arms. They also may have trouble initiating or continuing movement.
Q: I Have Parkinsons Disease Should I Receive A Covid
A: For information about the COVID-19 vaccines how they work, safety, and more please visit our updated COVID-19 information section. In general, your age alone increases your risk of complications from COVID-19 infection. Depending on what PD symptoms you have, PD can also increase the risk of complications from the virus. For these reasons, it would be wise to protect yourself as much as possible from COVID-19, which would include getting vaccinated. As always, speak to your doctor about your individual clinical situation and to find out when and where you will be able to get the vaccine.
Causes And Risk Factors Of Parkinsons Disease
![[CNS] 2](https://www.parkinsonsinfoclub.com/wp-content/uploads/cns-2-what-is-parkinsons-disease-symptoms-causes.jpeg)
Genetics aside, environmental risk factors include head injury, area of residence, occupation, solvents and polychlorinated biphenyls, as well as exposure to pesticides, herbicides, and metals. Head injury refers to a traumatic brain injury that alters the level of consciousness, which seems to increase the risk of developing Parkinsons disease some years later. As for area of residence and occupation, there are differences in both the geographic distribution of Parkinsons disease and the incidence of Parkinsons disease in certain occupational categories. Pesticide and herbicide exposure are linked to Parkinsons disease, while metal exposure seems to be related to its development, but the exact connection is not entirely understood. Lastly, high concentrations of PCBs have been found in the brains of people with Parkinsons disease.
Apart from potential genetic causes and environmental risk factors, other risk factors include age and gender. More specifically, the number of people diagnosed with Parkinsons disease increases with age, regardless of sex, and approximately 1 percent of people over the age of 60 have the disease. As for gender, men are more likely to have Parkinsons disease than women. In rare cases, Parkinsonian symptoms can be caused by MPTP. This is a toxic impurity that can be found in the recreational drug MPPP, or desmethylprodine, which is a synthetic opioid.
Resources:
Q: Are There Any Studies Of The Long
A: A recent study examined post-COVID symptoms in a small number of PD patients. Among the symptoms that persisted after COVID infection included worsening of motor function, increased levodopa daily dose requirements, fatigue, cognitive disturbances, and sleep disturbances. More research will need to be done to corroborate and expand on these findings.
Even Modest Consumption Of Low
While the findings may point towards overindulging in low-fat dairy as a potential precursor to increased Parkinson’s risk, a deeper dive into the data proved otherwise. Even people who consumed just one serving of low-fat dairy a day were still 39 percent more likely to develop the neurological disorder compared to those who had less than one serving a week.
“Our study is the largest analysis of dairy and Parkinson’s to date,” study author Katherine C. Hughes, ScD, said in a statement. “The results provide evidence of a modest increased risk of Parkinson’s with greater consumption of low-fat dairy products. Such dairy products, which are widely consumed, could potentially be a modifiable risk factor for the disease.”
Hughes also noted that a 2002 study published in the journal Annals of Neurology linked consumption of dairy products with a modest increased risk of Parkinson’s in men but did not find the same correlation among women.
What Role Do Genes Play
Your genes are like your body’s instruction book. So if you get a change in one of them, it can make your body work in a slightly different way. Sometimes, that means you’re more likely to get a certain disease.
There are several genetic mutations that can raise your risk for Parkinson’s, each by a little bit. They have a part in about 1 in 10 cases.
If you have one or more of these changes, it doesn’t mean you’ll get Parkinson’s. Some people will, but many won’t, and doctors don’t know why. It may have to do with other genes or something in your environment.
Who Is At The Highest Risk Of Developing Parkinsons Disease As A Result Of Paraquat Exposure
Everyone who worked with or was frequently around paraquat is at risk of developing Parkinsons disease, as this herbicide is very toxic. The majority of people who use paraquat are agricultural workers. However, there are some categories of people who have the highest risk of developing Parkinsons disease as a consequence of prolonged exposure to paraquat, which refers to the following:
Consequently, agricultural workers are not the only category of people who are at risk of developing Parkinsons disease following paraquat exposure. If you notice the symptoms of this condition in a family member with a history of paraquat exposure, we strongly advise you to encourage them to seek medical attention. Because Parkinsons disease is often misdiagnosed, your family member may need to look for a second and even a third opinion from medical specialists if they do not receive a diagnosis of Parkinsons disease after their initial appointment. It is important to keep in mind that only individuals who struggle with Parkinsons disease are eligible for compensation if they were exposed to paraquat.
