Coming To Terms With A Parkinson’s Diagnosis
Being diagnosed with Parkinsons can an emotional experience. Some people feel shocked or confused others feel angry or anxious. Some people even feel relieved to have an explanation for their symptoms.
Here we share how people have coped with their own diagnosis.
- I do think about how I might be in a year, five years, 10 years, but there is no point worrying about it, it won’t change anything. I try to focus on what I can do NOW.
- There are times when I’m terrified and I mourn the loss of what I can do. And some times, I want to scream and shout. But mostly, I get on and work
- Hang in there and keep smiling. Its difficult and I admit I always have Parkinsons words floating around in my mind. But I choose to just investigate the research and how we can be helped in the future.
- My local Parkinsons UK group is amazing. Its been an absolute lifeline and I couldnt imagine managing without it.
- Tell all of your friends and family – they will become a pillar of support.
- Get in touch with a Parkinsons nurse. They are a great source of information.
Our helpline is here to answer any questions you have about your recent diagnosis and life with Parkinson’s. You can call us on 0808 800 0303 or email
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
How Is Parkinson’s Diagnosed
Current evidence suggests that Parkinsons tends to develop gradually. It may be many months, even years, before the symptoms become obvious enough for someone to go to the doctor.
This information looks at what parkinsonism is, how Parkinsons and other similar conditions may be diagnosed, and explains some of the tests that may be involved in the process.
Parkinsonism is a term used to describe symptoms or signs that are found in Parkinsons, but which can also be found in other conditions that cause slowness of movement, stiffness and tremor.
Most people with a form of parkinsonism have idiopathic Parkinsons disease, also known as Parkinsons. Idiopathic means the cause is unknown.
Other less common forms of parkinsonism include multiple system atrophy , progressive supranuclear palsy , drug-induced parkinsonism and vascular Parkinsons.
If youre concerned about symptoms youve been experiencing, you should visit your GP. If your GP suspects you have Parkinsons, clinical guidelines recommend they should refer you quickly to a specialist with experience in diagnosing the condition .
Its not always easy to diagnose the condition. So its important that you see a Parkinsons specialist to get an accurate diagnosis and to consider the best treatment options.
Diagnosing Parkinsons can take some time as there are other conditions, such as essential tremor , with similar symptoms. There is also currently no definitive test for diagnosing Parkinsons.
Also Check: Signs Of Parkinson’s In Young Adults
Pd Diagnosis Disease Severity And Disease Progression
The diagnosis of PD is essentially clinical , and we believe that the clinical evaluation of patients will not be replaced by modern imaging techniques. Nevertheless, as pointed out earlier, misdiagnosis can approach 20% of cases . Recently, in line with the European Union, the U.S. FDA approved DAT scan as a diagnostic tool to help differentiate between PD and Essential Tremor. This is the only current FDA-approved subsidiary examination to aid in PD diagnosis.
The role of magnetic resonance imaging in the diagnosis of PD is still not fully established. Traditionally, it has been seen as a means to potentially exclude alternate diagnoses such as vascular parkinsonism, or more importantly , atypical forms of degenerative parkinsonism such as MSA or progressive supranuclear palsy . Traditional structural MRI findings of these latter diagnoses such as increased pallidal iron, rim of putaminal hyperintensity, hot cross bun sign and/or cerebellar atrophy in MSA or the hummingbird or penguin sign in PSP may not be reliable, particularly in early disease.
Figure 5. Multimodal MRI in PD. Differences are noted between patients with PD and controls through voxel-based analysis of R2, mean diffusivity, and fractional anisotropy maps.
Brent A. Vogt, in, 2019
Network Analysis And Cognition
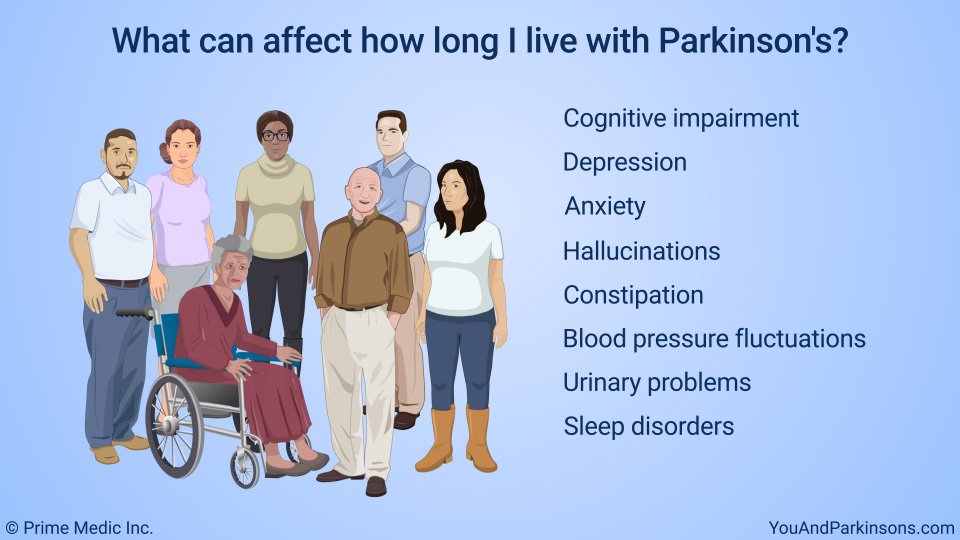
While the clinical diagnosis of PD rests largely on the motor signs and symptoms , non-motor symptoms can be prominent and even precede the motor symptoms . For example, RBD, as discussed earlier, represents a strong risk factor for PD . Cognitive dysfunction can be substantial in PD, typically appearing later in the disease and progressing slower. Nevertheless, the point prevalence of PD is high , and with time the majority of patients will develop cognitive impairment or dementia .
Neurology87Cold Spring Harbor Perspectives in Medicine2Neurology87Neuroimage78
The partial relation between PDCP expression and dopaminergic dysfunction may help explain why non-demented PD patients can have different changes in cognition when receiving dopaminergic treatments. Specifically, improvement in verbal learning that some patients exhibit with levodopa treatment, depends on baseline PDCP expression . PD patients with caudate tracer uptake in the 3550% range exhibit modest PDCP elevations and show improved cognitive response with medications. In contrast, those with a relatively intact caudate dopaminergic system exhibit cognitive decline with levodopa, which is in accordance with a dopamine overdose hypothesis . Similarly, patients with advance dopaminergic dysfunction and high PDCP scores lose the cognitive benefit from levodopa, possibly due to advance pathology in key PDPC nodes .
Recommended Reading: Levodopa Price
Diagnosing Early Onset Parkinsons Disease
There is no single test to detect Parkinsons. A diagnosis may be difficult and take a while. The condition is usually diagnosed by a neurologist based on a review of your symptoms and a physical exam.
A DaTscan to visualize your brains dopamine system may help confirm diagnosis. Blood tests and other imaging tests, such as an MRI scan, dont diagnose Parkinsons. However, they may be used to rule out other conditions.
What Is Parkinsons Disease
Parkinsons disease is a progressive brain disorder that affects mobility and mental ability. If you or a loved one has been diagnosed with Parkinsons, you may be wondering about life expectancy.
According to some research, on average, people with Parkinsons can expect to live almost as long as those who dont have the condition.
Also Check: Lateral Superior Pontine Syndrome
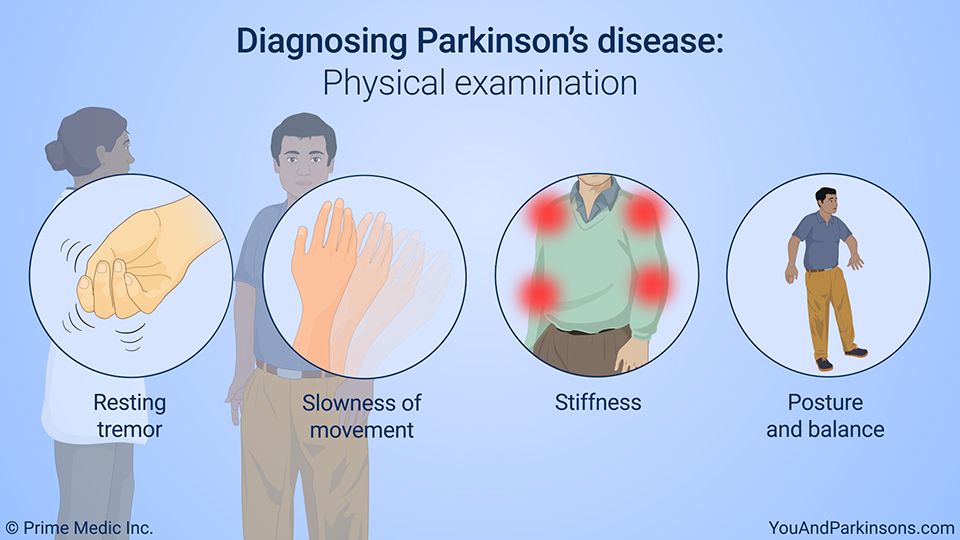
Physical And Neurological Examination
Your doctor will conduct a physical and neurological examination. This can involve observing your behavior, movements, and mental state and conducting tests or asking you to perform certain exercises.
These are some of the symptoms of Parkinsons your doctor can determine visually:
- Fewer spontaneous movements or hand gestures
- Reduced frequency of blinking
- Tremors in your hands while they are at rest, often only in one hand
- Hunched posture or forward lean while walking
- Stiff movements
These are some of the exercises your doctor may ask you to do to evaluate your movements, balance, and coordination:
- Opening and closing your fist
- Tapping your fingers, toes, and heels
- Holding your arms out in front of you
- Moving your finger from one point to another
- Rotating your wrists or ankles
- Standing from a chair
The Plus Side Of An Early Diagnosis
The news is not nearly all bad for those with young-onset Parkinsons. For one thing, patients with YOPD are better candidates for surgical procedures and medical innovations being used or developed to treat Parkinsons disease. For another, younger patients are less likely to be coping with other health problems at the same time.
Targeting Parkinsons-Linked Protein Could Neutralize 2 of the Diseases Causes
Researchers report they have discovered how two problem proteins known to cause Parkinsons disease are chemically linked, suggesting that someday, both could be neutralized by a single drug designed to target the link.
Read Also: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Diagnosis Of Parkinson Disease: Motor Symptoms
The clinical diagnosis of Parkinson’s disease is based on the presence of characteristic motor symptoms: bradykinesia, rigidity, postural instability, and resting tremor but neuropathology is still considered the gold standard for definite diagnosis. Differentiating PD from other movement disorders can be challenging throughout the disease course, because signs and symptoms often overlap. Indeed, neuropathology studies reveal that clinical diagnosis of PD can be confirmed with an accuracy of about 75%. Good response to levodopa is often used to support the diagnosis of PD. However, cases of pathologically proven PD with poor response to levodopa have also been reported.
Misdiagnosis of PD can occur for several reasons. In a community-based study of patients taking antiparkinsonian medication, the most common misdiagnosis were essential tremor, Alzheimer’s disease, and vascular parkinsonism. In addition, many of the prominent features of PD may also occur as a result of normal aging or from comorbid and multifactorial medical conditions .
R. Savica, … G. Logroscino, in, 2016
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
Also Check: Lifespan Parkinson’s
Obtaining A Parkinson’s Disease Diagnosis
During the exam, the neurologist will look for cardinal symptoms of the disease. Facial expressions and features will be assessed. The doctor will look for signs of tremor while the patient is at rest. The doctor may watch how easily the patient stands up from sitting in a chair. The doctor may also stand behind the patient and gently pull back on the patients shoulders and look for how easily the patient can regain balance. Good responsiveness to levodopa also helps support the diagnosis of PD. However, taking levodopa may exclude patients from clinical studies that need to recruit recently diagnosed patients who have not yet had treatment . Participation in a clinical trial should be discussed with the doctor.
PD can be challenging to accurately diagnose, particularly in early stages of the disease, which is why a neurologist trained in movement disorders is critical. Approximately 5-10% of patients with PD are misdiagnosed, as many of the symptoms of PD are similar to other diseases. If the patient thinks that he or she has been misdiagnosed, a second opinion may help.1,2
What Are The Stages To Coping With My Condition
Parkinsons disease causes recurring bouts of grief. Your life will change and you will no longer be able to continue all your activities.
These are the stages most individuals go through before accepting their diagnosis and developing new life skills. A psychologist specializing in neurodegenerative diseases can help you go through these stages more easily.
Don’t Miss: Yopd Life Expectancy
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
How Many Canadians Live With Parkinsonism And How Many Are Newly Diagnosed Each Year
Based on the latest estimates available , in 20132014, approximately 84,000 Canadians aged 40 years and older were living with diagnosed parkinsonism and 10,000 Canadians were newly diagnosed with this condition . The age-standardized prevalence was 1.5Footnote i times higher among males than among females , and similarly the age-standardized incidence was 1.7Footnote i times higher among males than females . The epidemiological burden of parkinsonism increases with age. In 20132014, when comparing estimates among Canadians aged 85 years and older vs. those aged 40-44 years, the prevalence of the condition was 169Footnote i times higher in the older age group , while the incidence was 48Footnote i times higher in the older age group .
Figure 1: Prevalence of diagnosed parkinsonism, including Parkinsons disease, by sex and age group, Canada, 20132014
| Age group |
|---|
| 44.7 | 55.1 |
Note: The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20. Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, July 2017.
You May Like: How Long Does End Stage Parkinson’s Last
Is Early Diagnosis Possible
Experts are becoming more aware of symptoms of Parkinsons that precede physical manifestations. Clues to the disease that sometimes show up before motor symptoms and before a formal diagnosis are called prodromal symptoms. These include the loss of sense of smell, a sleep disturbance called REM behavior disorder, ongoing constipation thats not otherwise explained and mood disorders, such as anxiety and depression.
Research into these and other early symptoms holds promise for even more sensitive testing and diagnosis.
For example, biomarker research is trying to answer the question of who gets Parkinsons disease. Researchers hope that once doctors can predict that a person with very early symptoms will eventually get Parkinsons disease, those patients can be appropriately treated. At the very least, these advances could greatly delay progression.
Parkinson’s Disease and Movement Disorders Center
Our center provides compassionate and timely treatment to patients with movement disorders, such as dystonia, ataxia, essential tremor and similar conditions. But our mission goes beyond patient care excellence. By offering educational events and support groups, we empower patients and caregivers to become better partners in their health.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Don’t Miss: Non Motor Symptoms Of Parkinson’s
Who Gets Parkinsons Disease
Parkinsonâs disease, documented in 1817 by physician James Parkinson, is the second most common neurodegenerative disease after Alzheimerâs disease. Estimates regarding the number of people in the United States with Parkinsonâs range from 500,000 to 1,500,000, with 50,000 to 60,000 new cases reported annually. No objective test for Parkinsonâs disease exists, so the misdiagnosis rate can be high, especially when a professional who doesnât regularly work with the disease makes the diagnosis.
Molecular Imaging In Parkinson’s Disease
The diagnosis of PD relies on the clinical manifestation of cardinal motor symptoms, bradykinesia, and tremor at rest or rigidity . A positive response to dopaminergic drugs is supportive of the diagnosis. Single photon emission computed tomography or PET ligands that are specific for dopamine transporters indirectly enable the quantification of the deficit of dopaminergic nigrostriatal projections and can provide further support of diagnosis . Deficiencies of monoamine synthesis can be measured with dihydroxyphenylalanine which is a substrate for the enzyme aromatic amino acid decarboxylase in all monoaminergic neurons including noradrenergic neurons .
The role of deficits of noradrenaline in motor and non-motor symptoms is not clear and research on the noradrenergic system in PD patients has been hindered by lack of specific methods to visualize the noradrenergic neurons and projections in vivo. We have recently carried out PET studies to investigate the role of noradrenaline in non-motor symptoms in PD patients and these studies will form the basis of discussions in the paragraphs below.
Paul Johns BSc BM MSc FRCPath, in, 2014
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s
