What Is Wolff Parkinson White Syndrome
Wolff-Parkinson-White syndrome is a heart condition that causes the heart to beat abnormally fast for periods of time.
Its a relatively common condition, affecting between one and three in every 1,000 people.
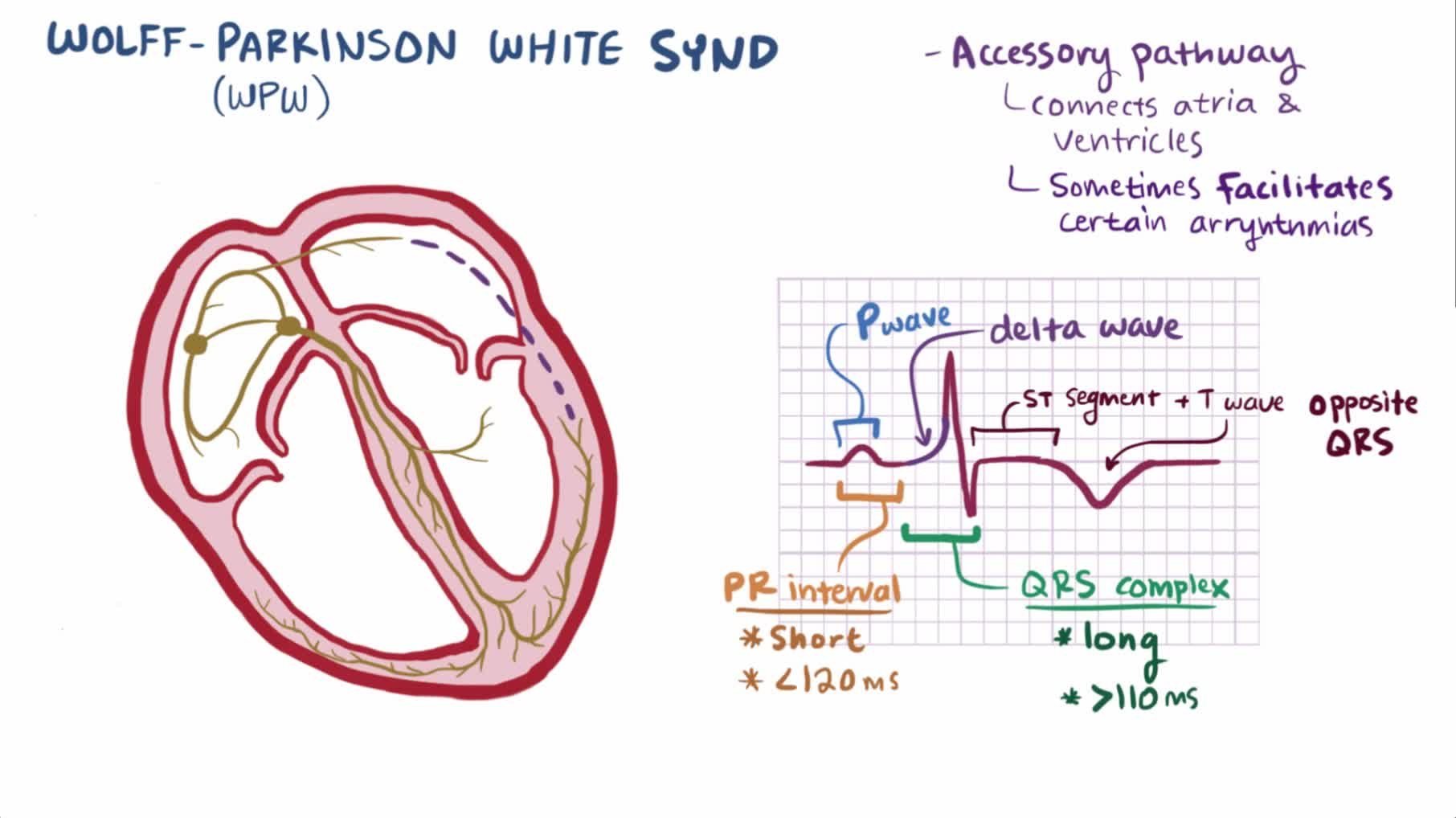
The cause is an abnormal;electrical pathways between the atria and ventricles causing the electrical signal to arrive at the ventricles too soon and to be transmitted back into the atria. These accessory pathways can cause electrical impulses to travel in both directions rather than one direction . In Wolff-Parkinson-White syndrome, an extra electrical pathway between your hearts upper chambers and lower chambers causes a rapid heartbeat. Some people with Wolff Parkinson White syndrome also have atrial fibrillation. Wolff Parkinson White syndrome causes the conduct of impulses to be faster than normal. Very fast heart rates may develop as the electrical signal ricochets between the atria and ventricles. Some people with WPW syndrome dont have symptoms but they still have an increased risk for sudden death.
This problem with the heart is present at birth , although symptoms may not develop until later in life. Many cases are diagnosed in otherwise healthy adults aged between 20 and 40.
Sometimes the extra electrical connection wont cause any symptoms and may only be picked up when an electrocardiogram test is carried out for another reason. In these cases, further tests will be done to determine if treatment is required.
Wolff Parkinson White Syndrome Treatment
In many cases, episodes of abnormal heart activity associated with Wolff Parkinson White syndrome are harmless, dont last long and settle down on their own without treatment.
You may therefore not need any treatment if your symptoms are mild or occur very occasionally, although you should still have regular check-ups so your heart can be monitored.
If your cardiologist recommends treatment, there are a number of options available. You can have treatment to either stop episodes when they occur, or prevent them occurring in the future.
Wolff Parkinson White Syndrome Symptoms
People of all ages, including infants, can experience the symptoms related to Wolff Parkinson White syndrome.
If you have Wolff Parkinson White syndrome, youll experience episodes where your heart suddenly starts racing, before stopping or slowing down abruptly. This rapid heart rate is called supraventricular tachycardia .
Symptoms of Wolff Parkinson White syndrome are the result of a fast heart rate. They most often appear for the first time in people in their teens or 20s.
Common symptoms of Wolff Parkinson White syndrome include:
- Sensation of rapid, fluttering or pounding heartbeats
- Dizziness or lightheadedness
Signs and symptoms in infants with WPW syndrome may include:
- Ashen color
- Rapid breathing
- Poor eating
An episode of a very fast heartbeat can begin suddenly and last for a few seconds,;minutes or several hours. Rarely, they can last for days. Episodes can occur during exercise or while at rest. Caffeine or other stimulants and alcohol may be a trigger for some people.
How often they occur varies from person to person. Some people may have episodes on a daily basis, while others may only experience them a few times a year.
They normally occur randomly, without any identifiable cause, but they can sometimes be triggered by strenuous exercise or drinking a lot of alcohol or caffeine.
If youve already been diagnosed with WPW syndrome and you experience an episode, first try the techniques youve been taught or take any medication youve been given .
Recommended Reading: Essential Oils For Parkinson’s
Normal Heart Electrical System
Your heart is made up of four chambers two upper chambers and two lower chambers . The rhythm of your heart is normally controlled by a mass of tissue in the right atrium . The sinus node produces electrical impulses that generate each heartbeat.
These electrical impulses travel across the atria, causing muscle contractions that pump blood into the ventricles. The electrical impulses then arrive at a cluster of cells called the atrioventricular node usually the only pathway for signals to travel from the atria to the ventricles. The AV node slows the electrical signal before sending it to the ventricles.
This slight delay allows the ventricles to fill with blood. When electrical impulses reach the ventricles, muscle contractions pump blood to the lungs and the rest of the body.
Figure 1. The hearts electrical system
Catheter Ablation Of Accessory Pathways
Lesh, MD, Van Hare, G, Scheinman, MM. Comparison of the retrograde and transseptal methods for ablation of left free-wall accessory pathways. J Am Coll Cardiol. vol. 22. 1993. pp. 542-9.
Jackman, WM, Wang, X, Friday, KJ. Catheter ablation of accessory atrioventricular pathways by radiofrequency current. N Engl J Med. vol. 324. 1991. pp. 1605-11.
Kuck, KH, Schluter, M, Geiger, M. Radiofrequency current catheter ablation of accessory atrioventricular pathways. Lancet. vol. 337. 1991. pp. 1557-61.
Calkins, H, Langberg, J, Sousa, J. Radiofrequency catheter ablation of accessory atrioventricular connections in 250 patients: abbreviated therapeutic approach to Wolff-Parkinson-White syndrome. Circulation. vol. 85. 1992. pp. 1337-46.
Kay, GN, Pressley, JC, Packer, DL. Value of 12-lead electrocardiogram in discriminating atrioventricular nodal reciprocating tachycardia from circus movement atrioventricular utilizing a retrograde accessory pathway. Am J Cardiol. vol. 59. 1987. pp. 296-300.
Tchou, PJ, Lehmann, MJ, Donga, J. Effect of sudden rate acceleration on the human His-Purkinje system: adaptation of refractoriness in a damped oscillatory pattern. Circulation. vol. 73. 1986. pp. 920-9.
Drago, F, DeSantis, A, Grutter, G, Silverti, MS. Transvenous cryothermal catheter ablation of re-entry circuit located near the atrioventricular junction in pediatric patients. J Am Coll Cardiol. vol. 45. 2005. pp. 1096-103.
Read Also: Parkinsons Disease Gene
Management Of Asymptomatic And Symptomatic Preexcitation
Blomström-Lundqvist, C, Scheinman, MM, Aliot, EM. ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular ArrhythmiasExecutive Summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines . Circulation. vol. 108. 2003. pp. 1871-1909.
Klein, GJ, Gulamhusien, SS. Intermittent preexcitation in the Wolff-Parkinson-White syndrome. Am J Cardiol. vol. 52. 1983. pp. 292-6.
Campbell, RWF, Smith, R, Gallagher, JJ. Atrial fibrillation in the preexcitation syndrome. Am J Cardiol. vol. 40. 1977. pp. 514-20.
Auricchio, A, Klein, H, Trappe, HJ. Lack of prognostic value of syncope in patients with Wolff-Parkinson-White syndrome. J Am Coll Cardiol. vol. 17. 1991. pp. 152-8.
Wellens, HJ, Bar, FW, Gorgels, AP. Use of ajmaline in patients with the Wolff-Parkinson-White syndrome to disclose short refractory period of the accessory pathway. Am J Cardiol. vol. 45. 1980. pp. 130-33.
Brembilla-Perrot, B, Ghawi, R. Electrophysiological characteristics of asymptomatic Wolff-Parkinson-White syndrome. Eur Heart J. vol. 14. 1993. pp. 511-15.
Leitch, JW, Klein, GJ, Yee, R, Murdock, C. Prognostic value of electrophysiology testing in asymptomatic patients with Wolff-Parkinson-White pattern. Circulation. vol. 82. 1990. pp. 1718-23.
Wolff Parkinson White Syndrome Complications
For many people, WPW syndrome doesnt cause significant problems. But complications can occur, and its not always possible to know your risk of serious heart-related events. If the disorder is untreated, and particularly if you have other heart conditions, you may experience:
- Fainting spells
- Rarely, sudden death
Also Check: Parkinson’s Cannabis Oil
How Is This Problem Diagnosed
Clinical features: See Supraventricular tachycardia.
Physical findings: Most of the time the physical examination is normal when the child is not having an episode. In about 15% of children, the problem is associated with a heart defect. In this case the child has physical findings associated with that defect.
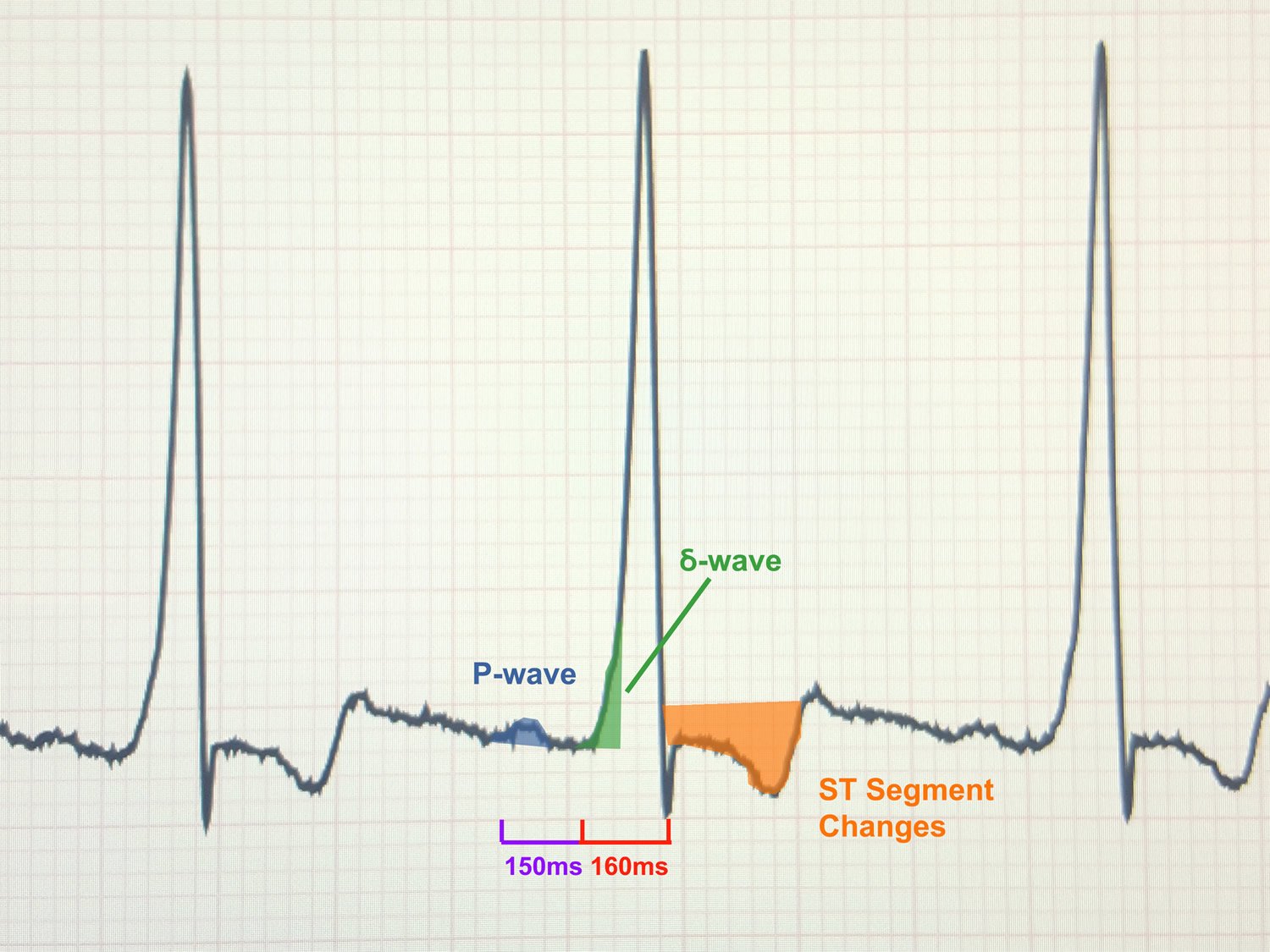
Medical tests: One of the first tests usually done is an electrocardiogram. This is a safe a painless test that involves putting some stickers across the chest. The stickers are connected to a machine that records the hearts electrical activity. In WPW, the resting ECG shows pre-excitation. This finding is quite specific for WPW and helps to confirm the diagnosis. Sometimes, pre-excitation is found on a routine ECG in a person who has no symptoms.
It may be important to record an ECG at the time of symptoms. This is done by device called a transtelephonic ECG recorder. There are different models of these devices available, but they are all able to record an ECG at the time of symptoms. The tracing can then be sent over the phone to a cardiology center where it can be reviewed. Other tests that may be done include a Holter monitor, echocardiogram, and/or exercise test.
How Is Wpw Treated
Treatment depends on the type and frequency of arrhythmias, associated symptoms such as syncope, and presence of structural heart disease. Typically a physician will recommend an ablation procedure to further define the characteristics of the accessory pathway, and ultimately, to eliminate the pathway entirely.
- Observation – If you have no symptoms, you may not require treatment. Your doctor may choose to have regular follow-up without treatment.
- Medications – A variety of drugs are available to treat arrhythmias. Because everyone is different, it may take trials of several medications and doses to find the one that works best for you. It is important to know:
- The names of your medications
- What they are for
- How often and at what times to take them
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Prevalence Symptoms And Prognosis Of Wpw Syndrome
An electrocardiographic pattern of preexcitation occurs in the general population at a frequency of around 1.5 per 1000. Of these, 50% to 60% of patients become symptomatic. Approximately one-third of all patients with paroxysmal supraventricular tachycardia are diagnosed as having an AP-mediated tachycardia. Patients with AP-mediated tachycardias most commonly present with the syndrome of PSVT.
Population-based studies have demonstrated a bimodal distribution of symptoms for patients with preexcitation, with a peak in early childhood followed by a second peak in young adulthood. Nearly 25% of infants who demonstrate preexcitation and/or have AP-mediated arrhythmias will lose evidence of preexcitation and/or become asymptomatic over time as the conduction property of the AP can degenerate with time.
Pappone et al reported that during a mean follow-up of 37.7 months, 18.2% and 30% of noninducible patients have lost the anterograde and retrograde conduction, respectively. The mean age of these patients was 33.6 ± 14.3. Compared to others who had persistent conductibility through the AP, these patients were asymptomatic, noninducible, and had longer minimal 1:1 conduction cycle length through the AP during the baseline EPS.
How Can We Tell The Location Of The Ap Based On The Superficial 12 Lead Ecg
Gallager, JJ, Pritchett, ELC, Sealy, WC. The preexcitation syndromes. Prog Cardiovasc Dis. vol. 20. 1978. pp. 285-327.
Ross, DL, Uther, JB. Diagnosis of concealed accessory pathways in supraventricular tachycardia. Pacing Clin Electrophysiol. vol. 7. 1984. pp. 1069-85.
Arruda, MS, McClelland, JH, Wang, X. Development and validation of an ECG algorithm for identifying accessory pathway ablation site in Wolff-Parkinson-White syndrome. J Cardiovasc Electrophysiol. vol. 9. 1998. pp. 2-12.
Fitzpatrick, AP, Gonzales, RP, Lesh, MD. New algorithm for the localization of accessory atrioventricular connections using a baseline electrocardiogram. J Am Coll Cardiol. vol. 23. 1994. pp. 107-16.
Lindsay, BD, Crossen, KJ, Cain, ME. Concordance of distinguishing electrocardiographic features during sinus rhythm with the location of accessory pathways in the Wolff-Parkinson-White syndrome. Am J Cardiol. vol. 59. 1987. pp. 1093-1102.
Cain, ME, Luke, RA, Lindsay, BD. Diagnosis and localization of accessory pathway. Pacing Clin Electrophysiol. vol. 15. 1992. pp. 801-24.
DAvila, A, Brugada, J, Skeberis, V. A fast and reliable algorithm to localize accessory pathways based on the polarity of the QRS complex on the surface ECG during sinus rhythm. Pacing Clin Electrophysiol. vol. 18. 1995. pp. 1615-27.
Xie, B, Heald, SC, Bashir, Y. Localization of accessory pathways from the 12-lead electrocardiogram using a new algorithm. Am J Cardiol. vol. 74. 1994. pp. 161-5.
Recommended Reading: How Long Does It Take For Parkinson’s Disease To Progress?
How Is Wpw Diagnosed
WPW can only be diagnosed by reviewing an ECG . A holter or ambulatory monitor and exercise testing are also helpful in evaluating patients known to have WPW.
In the past, patients with WPW but without symptoms had been observed by a cardiologist for many years. Recently, new guidelines have been published for this group of patients. Your cardiologist may order a holter monitor or stress test to look for a persistent patter of WPW. If the WPW pattern persists, invasive electrophysiology testing is now recommended.
Your doctor will also ask you several questions:
- Do you have symptoms?
- Do you have a history of atrial fibrillation?
- Do you have a history of fainting?
- Do you have a history of sudden cardiac death or does anyone in your family?
- Are you a competitive athlete?
The results of your diagnostic tests and the answers to these questions will help guide your therapy.
How Is The Problem Treated
See supraventricular tachycardia. Patients may be treated with heart medicines to prevent episodes of SVT. In general, infants are treated until their first birthday and then the medicines can be stopped. In older children, radiofrequency ablation has become first line treatment as it is safe with high success rates.
Recommended Reading: Average Life Expectancy With Parkinson’s
What Are The Symptoms Of Wpw
People may first experience symptoms at any age, from infancy through adult years.
Symptoms of WPW may include one or more of the following:
- Heart palpitations a sudden pounding, fluttering or
- Racing feeling in your chest
- Dizziness feeling lightheaded or faint
- Shortness of breath
- Rarely, cardiac arrest
Some people have WPW without any symptoms at all.
Are There Any Specific Tachycardias Associated With Accessory Pathways
Cain, ME, Luke, RA, Lindsay, BD. Diagnosis and localization of accessory pathways. Pacing Clin Electrophysiol. vol. 15. 1992. pp. 801-24.
Reyes, W, Milstein, S, Dunnigan, A. Indications for modification of coexisting dual atrioventricular node pathways in patients undergoing surgical ablation of accessory atrioventricular connections. J Am Coll Cardiol. vol. 17. 1991. pp. 1561-7.
Klein, GJ, Bashore, TM, Sellers, TD. Ventricular fibrillation in the Wolff-Parkinson-White syndrome. N Engl J Med.. vol. 301. 1979. pp. 1080-5.
Dreifus, LS, Haiat, R, Watanabe, Y. Ventricular fibrillation: a possible mechanism of sudden death in patients with Wolff-Parkinson-White syndrome. Circulation. vol. 43. 1971. pp. 520-7.
Wellens, HJJ, Durrer, D. Wolff-Parkinson-White syndrome and atrial fibrillation. Am J Cardiol. vol. 34. 1974. pp. 777-82.
Campbell, RWF, Smith, R, Gallagher, JJ. Atrial fibrillation in the preexcitation syndrome. Am J Cardiol. vol. 40. 1977. pp. 514-20.
Sharma, AD, Klein, GJ, Guiraudon, GM. Atrial fibrillation in patients with Wolff-Parkinson-White syndrome: incidence after surgical ablation of the accessory pathway. Circulation. vol. 72. 1985. pp. 161-9.
Dagres, N, Clague, JR, Lottkamp, H. Impact of radiofrequency catheter ablation of accessory pathways on the frequency of atrial fibrillation during long-term follow-up: high recurrence rate of atrial fibrillation in patients older than 50 years of age. Eur Heart J. vol. 22. 2001. pp. 423-7.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Treatments For Wpw Syndrome
In many cases, episodes of abnormal heart activity associated with WPW syndrome are harmless, don’t last long, and settle down on their own without treatment.
You may therefore not need any treatment if your symptoms are;mild or occur very occasionally, although you should still have regular check-ups so your heart can be monitored.
If your cardiologist recommends treatment, there are a number of options available.;You can have treatment;to either stop episodes when they occur, or prevent them occurring in the future.
Are There Different Types Of Accessory Pathways
Lown, B. The syndrome of short P-R interval, normal QRS complex and paroxysmal rapid heart action. Circulation. vol. 5. 1952 May. pp. 693-706.
James, TN. Morphology of the human atrioventricular node, with remarks pertinent to its electrophysiology. Am Heart J. vol. 62. 1961. pp. 756-71.
Lev, M, Leffler, WB, Langendorf, R. Anatomic findings in a case of ventricular preexcitation terminating in complete atrioventricular block. Circulation. vol. 34. 1966. pp. 718-33.
Murdock, CJ, Leitch, JW, Teo, WS. Characteristics of accessory pathways exhibiting decremental conduction. Am J Cardiol. vol. 67. 1991. pp. 506-10.
Ross, DL, Uther, JB. Diagnosis of concealed accessory pathways in supraventricular tachycardia. Pacing Clin Electrophysiol. vol. 7. 1984. pp. 1069-85.
Anderson, RH, Becker, AE, Brechenmacher, C. Ventricular pre-excitation: a proposed nomenclature for its substrates. Eur J Cardiol. vol. 3. 1975. pp. 27-36.
Mahaim, I, Benatt, A. Nouvelles recherches sur les connections superieures de la branche du faisceau de His-Tawara avec cloison interventriculaire. Cardiologia. vol. 1. 1937. pp. 61
Recommended Reading: Can Parkinson’s Change Your Personality
Wolff Parkinson White Syndrome Diagnosis
If your doctor thinks you might have Wolff Parkinson White syndrome after assessing your symptoms, theyll probably recommend having an electrocardiogram and will refer you to a cardiologist .
An ECG is a test that records your hearts rhythm and electrical activity. Small discs called electrodes are stuck onto your arms, legs and chest and connected by wires to an ECG machine. The machine records the tiny electrical signals produced by your heart each time it beats.
If you have Wolff Parkinson White syndrome, the ECG will record an unusual pattern that isnt usually present in people who dont have the condition.
To confirm the diagnosis, you may be asked to wear a small portable ECG recorder so your heart rhythm can be recorded during an episode. A Holter monitor records your heart activity for 24 hours. An event recorder monitors heart activity when you experience symptoms of a fast heart rate. The recorder will trace your heart rate continuously over a few days, or when you switch it on at the start of an episode.
Electrophysiological testing. Thin, flexible tubes tipped with electrodes are threaded through your blood vessels to various spots in your heart. The electrodes can precisely map the spread of electrical impulses during each heartbeat and identify an extra electrical pathway.
Wolff Parkinson White Syndrome Causes
When the heart beats, its muscular walls contract to force blood out and around the body. They then relax, allowing the heart to fill with blood again. This is controlled by electrical signals.
In Wolff Parkinson White syndrome, theres an extra electrical connection in the heart, which allows electrical signals to bypass the usual route and form a short circuit. This means the signals travel round and round in a loop, causing episodes where the heart beats very fast.
The extra electrical connection is caused by a strand of heart muscle that grows while the unborn baby is developing in the womb.
Its not clear exactly why this happens. It just seems to occur randomly in some babies, although rare cases have been found to run in families.
Wolff Parkinson White is more common in males than in females.
Also Check: Do People Die From Parkinsons

