Introducing Unlock Your Hip Flexors
Unlock Your Hip Flexors gives you a practical, easy-to-follow program you can use today for instantly releasing your hip flexors for more strength, better health and all day energy.
Working with Rick, weve created a great program that is quite simply Done-For-You.
Rick has pulled together a sequential flow designed just for you composed of 10 carefully selected exercises, including PNF Stretching, Static Stretching, Dynamic Stretching, 3-Dimensional Core Stability Exercises, Mobility Exercises, Fascia Stretching and Muscle Activation.
Unlock Your Hip Flexors DVD Video
Weve shot these 10 exercises with explanations from Rick on perfect form and exactly how to target that hard-to-reach psoas muscle. The video content is split in two:
The first is a Coaching Instructional Video where Rick takes you in detail through each exercise, so you fully understand why youre doing that exercise, the best form to take and how it should feel. The second video is a Follow Along format designed so you can perform the flow alongside the video without breaking for explanation.
Unlock Your Hip Flexors Manual
Youll receive a highly targeted manual with greater depth about the psoas muscle and the effects of its shortening on your health and well-being. It also includes detailed descriptions of the exact exercise movements with pictures.
You will experience immediate results the very first time you go through the program.
But first a warningthis isnt for everyone.
Changes In Sleeping Patterns
As Parkinsons progresses, you can also develop problems with sleep patterns. These may not happen in the early stages, but can be noticeable later. You might wake up often in the middle of the night or sleep more during the day than you do at night.
Another common sleep disturbance for people with Parkinsons is rapid eye movement sleep behavior disorder. This is when you start acting out your dreams in your sleep, such as verbally and physically, which can get uncomfortable if someone is sharing your bed. Dr. Rundle-Gonzalez says many times a bed partner will be the one to notice sleep problems.
REM sleep behavior disorder can also happen in people who dont have Parkinsons. However, if this isnt something youve dealt with before, its likely related to your disease. There are medications your doctor can prescribe to help you sleep comfortably through the night.
Sure Signs You’re Getting Parkinson’s According To Science
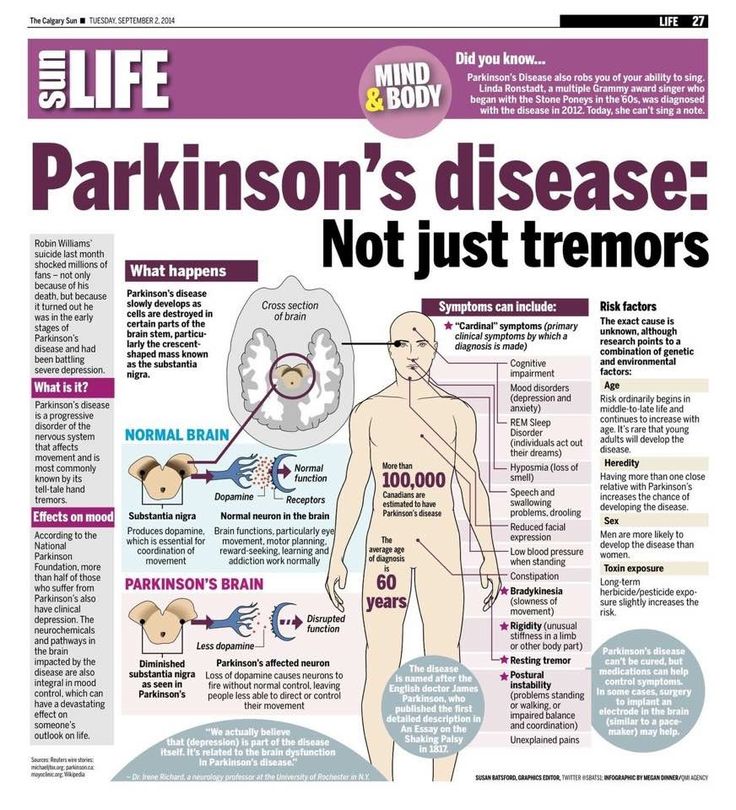
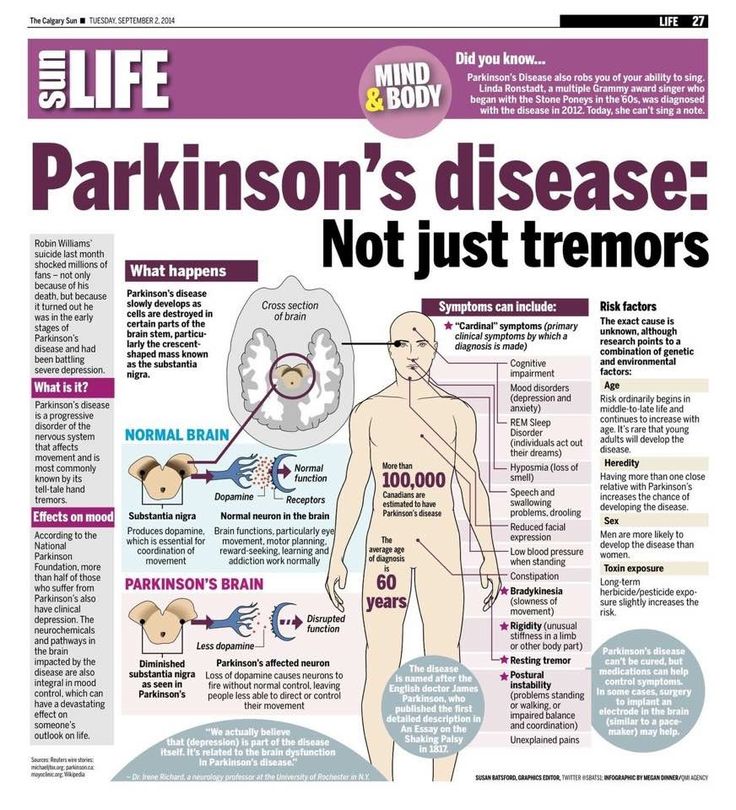
Parkinson’s diseasea progressive disorder of the brain and central nervous system that can impair movement and speechmay have vague or subtle symptoms at first. But it’s important to know what the first signals may be, so a proper diagnosis can be made and treatment can begin as soon as possible. These are some of the most common signs of Parkinson’s disease, according to the Parkinson’s Foundation. Read on to find out moreand to ensure your health and the health of others, don’t miss these Sure Signs You’ve Already Had COVID.
Also Check: What Is Early Onset Parkinson’s Disease
Cognitive And Psychiatric Symptoms
- depression and anxiety
- mild cognitive impairment slight memory problems and problems with activities that require planning and organisation
- dementia a group of symptoms, including more severe memory problems, personality changes, seeing things that are not there and believing things that are not true
If You Develop A Tremor
Urgent medical care isn’t needed if you’ve had a tremorâshaking or tremblingâfor some time. But you should discuss the tremor at your next doctor’s appointment.
If a tremor is affecting your daily activities or if it’s a new symptom, see your doctor sooner.
A written description will help your doctor make a correct diagnosis. In writing your description, consider the following questions:
- Did the tremor start suddenly or gradually?
- What makes it worse or better?
- What parts of your body are affected?
- Have there been any recent changes in the medicines you take or how much you take?
Don’t Miss: Does Adderall Help Parkinson’s
What Is Parkinsons Disease
Parkinson’s disease is a common neurodegenerative disorder, affecting about one percent of the population over the age of 60 years. While the typical age at onset is in the sixth decade of life , about five percent of patients with PD have onset of their symptoms before age 40. Parkinsons disease is twice as common in men as in women in most populations. It is a chronic, progressive disorder of the nervous system that affects movement. It develops gradually and can commonly cause tremor, stiffness, and slowness of movement. The symptoms of Parkinsons disease worsen as the condition progresses over time. Although there is no cure for Parkinsons disease, medications may markedly improve the symptoms of the disease.
Taking Medicine With Food
Early in the disease, it might be helpful to take pills with food to help with nausea, which may be caused by some of the medicines for Parkinson’s disease.
Later in the disease, taking the medicines at least 1 hour before meals may help them work best.
Some medicines for Parkinson’s disease don’t work as well if you take them at the same time you eat food with protein in it, such as meat or cheese. The protein can block the medicine and keep it from working as well as it should.
You May Like: Pathogenesis Of Parkinson’s Disease
How Is It Treated
At this time, there is no cure for Parkinson’s disease. But there are several types of medicines that can control the symptoms and make the disease easier to live with.
You may not even need treatment if your symptoms are mild. Your doctor may wait to prescribe medicines until your symptoms start to get in the way of your daily life. Your doctor will adjust your medicines as your symptoms get worse. You may need to take several medicines to get the best results.
Levodopa is the best drug for controlling symptoms of Parkinson’s. But it can cause problems if you use it for a long time or at a high dose. So doctors sometimes use other medicines to treat people in the early stages of the disease.
The decision to start taking medicine, and which medicine to take, will be different for each person. Your doctor will be able to help you make these choices.
In some cases, a treatment called deep brain stimulation may also be used. For this treatment, a surgeon places wires in your brain. The wires carry tiny electrical signals to the parts of the brain that control movement. These little signals can help those parts of the brain work better.
There are many things you can do at home that can help you stay as independent and healthy as possible. Eat healthy foods. Get the rest you need. Make wise use of your energy. Get some exercise every day. Physical therapy and occupational therapy can also help.
Improve Your General Fitness
Increasing your level of fitness will help you manage your weight and ensure your joints arent under any added pressure. You could try walking, swimming, dancing, cycling or aerobics its up to you.
Many of Parkinsons UKs local groups have physiotherapist-led exercise classes you can join. Visit our Local Support page or call our helpline on 0808 800 0303 to find one near you.
You May Like: Does Parkinson’s Cause Hallucinations
Types Of Parkinson’s Pain
Most of the time, discomfort in muscles and joints is secondary to the motor features of Parkinsons lack of spontaneous movement, rigidity, and abnormalities of posture what is known as musculoskeletal pain. The most commonly painful sites are the back, legs, and shoulders and it is usually more predominant on the side more affected by parkinsonism.
But there are many other categories of pain associated with Parkinsons disease. Radicular or neuropathic pain is experienced as a sharp pain that can start in the neck or lower back with radiation to arm or leg respectively and is often associated with numbness or tingling, or a sensation of coolness in the affected limb. It is usually secondary to a pinched nerve due to something like a slipped disc.
Dystonia related pain occurs as its name suggests, at times of dystonia most often experienced in the foot, neck or face and arm at different points in the dosing schedule, particularly the off phase when there is not enough dopamine replacement but can uncommonly also occur at peak-dose times. It can be one of the most painful symptoms those with Parkinsons can face.
Akathisia pain is experienced as restlessness, a subjective inner urge to move, an inability to stay still and the inherent feelings of discomfort that it brings. It is primarily experienced in the lower limbs and can often be relieved by walking around.
Interested In Parkinsons Disease Research Sign Up For Our Forums And Join The Conversation
A total of 97 Parkinsons patients at a mean age of 67.7 years, including 60 men, and 97 individuals used as controls at a mean age of 67.5 years, including six men, without the disorder or other neuromuscular diseases, filled out a questionnaire on the intensity of local lumbar back pain. The intensity of leg radicular pain caused by inflammation and/or injury to a spinal nerve root was quantified by the visual analogue scale a continuous scale used to measure pain intensity.
In addition, the participants permanent functional disability was assessed via the Oswestry Low Back Pain Disability Questionnaire a self-completed questionnaire that includes 10 different topics: intensity of pain, lifting, ability to care for oneself, ability to walk, ability to sit, sexual function, ability to stand, social life, sleep quality, and ability to travel.
Patients were further asked to describe the painful sensation they experience as pricking, tingling, burning, paresthesia often described as feelings of pins and needles, or numbness or other.
The team also assessed Parkinsons duration, medications being used, severity of motor symptoms as assessed by the Unified Parkinsons disease rating scale part III and the Hoehn and Yahr stage, which is a system used to assess symptom progression.
According to the ODI results, minimal disability was reported by 43.8% of Parkinsons patients, moderate disability by 27.5%, severe disability by 22.5%, and crippled by 6.3%.
Read Also: How Can Parkinson’s Disease Kill You
What Can You Do If You Have Pd
It is possible to have a great quality of life with PD. It is essential to work with your doctor and follow recommended therapies in order to successfully treat symptoms.
- Develop a plan with your doctor to stay healthy. This might include:
A referral to a neurologist, a doctor who specializes in the brain, or a Movement Disorder Specialist, a neurologist with additional training in PD
Care from an occupational therapist, physical therapist and/or speech therapist
Meeting with a medical social worker to talk about how Parkinsons will affect your life
- Start a regular exercise program to help manage symptoms and maintain well-being.
- Talk with family and friends who can provide you with the support you need.
The Parkinsons Foundation is here to help. Contact the Parkinsons Foundation Helpline for answers to your questions in either English or Spanish. Staffed by Parkinsons disease information specialists, the Helpline is free and here to support you and your loved ones in any way possible, including:
- Current information about Parkinsons
- Emotional support
- Referrals to health care professionals and community resources
A wide variety of free publications are also available. To order, call or email our Helpline: 1.800.4PD.INFO / .
Not ready to talk to someone about PD? Visit Parkinson.org for reliable information.
Impact On Mental Health
Living with chronic pain from PD can have a deep impact on your mental health. A study by the Parkinsons Foundation found that mood, anxiety, and depression have greater influence on your overall health than the other symptoms of PD.6
Depression is a medical condition that deserves treatment. If you have depression, know that you are not alone in feeling this way. Your doctor can help you get the treatment you need.6
The different types of pain that can occur in PD can be challenging. Knowing the symptoms and treatments available can help guide your conversations with your doctor. Treatment can bring hope and reduce suffering for many. Ways to treat pain will vary from person to person, but include:1
- Physical therapy
Recommended Reading: Will There Ever Be A Cure For Parkinson’s Disease
Q Are There Any Alternative Therapies That Are Effective For Pain In Pd
Dr. Fleisher: Although alternative therapies may be helpful, there is little evidence-based research to support their use. Certainly massage therapy, anecdotally, seems to be helpful for managing pain. Small studies suggest that acupuncture might improve sleep in patients with PD, but data on the effects on pain in PD is lacking. Larger, more well-controlled and reproducible studies of these therapies are needed.
Patients frequently ask about the effects of medical marijuana in managing PD, including pain symptoms. Several studies have looked at efficacy of marijuana in PD and have found that it probably is ineffective for most PD symptoms.¹¹ However, we just dont have enough evidence to know for sure. The most rigorous study of medical marijuana in PD showed a trend toward worsening tremor.¹¹¹²
For most people, stress and anxiety worsen tremor, and anything that relieves anxiety will improve tremor. Thus, modalities such as yoga, meditation, and mindfulness training will improve tremor. Similarly, medical marijuana may improve tremor in certain people by temporarily reducing anxiety and stress, but the evidence has not borne this out yet.
My Parkinson’s Story: Pain
This 10-minute video alternates between an interview with a man and and doctors. The man shares his experience with pain as a symptom of Parkinson’s disease. The doctors explain that pain is common in Parkinson’s disease, often due to rigidity or dystonia, which can be exacerbated by “off” periods. Pain caused by Parkinson’s symptoms can be relieved by Parkinson’s medications, exercise, DBS and botox injections. Pain is an invisible symptom that should be mentioned to your neurologist.
Recommended Reading: Who Can Diagnose Parkinson’s
Types Of Pain In Parkinsons
One review classified the types of PD pain as follows:
- musculoskeletal, in which the pain results from problems with the muscles , bones or joints
- dystonic, which is due to abnormal muscle contractions caused by PD or the medications used to treat it
- radicular pain or nerve pain
- central pain, which is poorly understood and thought to be due to abnormalities in the brain itself
Pain Sites And Assessments
All patients were asked to indicate the distribution of pain sites, duration of pain, and rate average pain intensity over the past 3 months on an 11-point numeric rating scale , with 0 indicating the absence of pain and ten indicating the most intense pain imaginable. The patients reported NRS scores in both the ON and OFF states of motor function on the same day. NRS scores were then transformed into WHO severity stages of mild , moderate , and severe , respectively . MSP responsiveness to Levodopa was defined as a 30% reduction in NRS scores from baseline, 2 h after taking the medication . Data regarding multiple types of pain were also recorded. The ID-pain scale detected central parkinsonian pain.
Don’t Miss: How I Was Diagnosed With Parkinson’s
If You Have Parkinson’s Disease
If you have been diagnosed with Parkinson’s, call your doctor if:
- You notice any significant change in your symptoms, such as severe episodes of freezingâa sudden loss of mobilityâwhich may affect walking.
- Your response to your medicine changes.
- Any other symptoms occur, such as constipation, sexual problems, or incontinence.
- You have symptoms of depression, such as feeling sad or losing interest in daily activities.
- You or your family notice that you have problems with memory and thinking ability.
Which Type Of Hip Replacement Should I Have
Your surgeon will discuss this with you. It will depend on who you are. In other words, how old you are, whether you have any other medical conditions and what you want to be able to do once you have had your hip replaced. It will also depend on what types of hip replacements your surgeon is used to performing and which ones are used in their hospital. In the UK the National Institute for Health and Care Excellence only recommends devices that are known to last at least 10 years in 95 out of every 100 people who have that type fitted.
All hip replacements can be divided into either cemented or uncemented.
Dont Miss: Best Walking Cane For Parkinsons
Recommended Reading: Parkinson’s Disease Big And Loud Therapy
Lower Back Pain And Back Of The Neck Pain Are Most Common
Pain occurs for a number of reasons and its not always clear what the cause is, making it difficult to figure out how best to treat it. I believe that most common pain problems in Parkinsons Disease are the same as in the general population, but amplified. Low back pain and back of the neck pain are probably the most common pain conditions in PD. The reason Parkinsons Disease patients have so many problems with their low back and their neck is their posture. Parkinsons Disease causes a stooped posture. Some of this happens with age anyway, particularly in women after menopause when their bones soften, but is always worse from the PD. All Parkinsons Disease patients have some degree of stooped posture and many also tilt to one side. Because of the stooped posture, the muscles in the lower back have to pull much harder to keep the spine upright.
The Parkinsons Disease News Today Forums Are A Place To Connect With Other Patients Share Tips And Talk About The Latest Research Check Them Out Today
PD pain can resemble pain from other disease processes, especially as the patient ages and faces a multitude of other pain-causing conditions such as arthritis, spine degeneration, poor muscular conditioning, and such. In my case, PD pain is distinguished by the following:
- The progression of body pain correlated with the progression of the disease over time.
- Levodopa, a dopaminergic therapy, successfully reduces the pain.
- The pain is worse during off periods.
My PD pain also has a particular characteristic: stinging , irritating tingling, burning, and muscle heaviness with increased pain on movement. This pain happens over large regions of the body and varies in severity. At its worst, it can last several days and reach level 7, inducing spontaneous tears.
PD with episodic chronic pain is disabling in several ways. First, high levels of pain obstruct clear thinking. Second, high levels of pain induce the fight-or-flight response, which interferes with emotion management. Third, the amount of energy necessary to manage it is very tiring . Chronic PD pain entails much more than body symptoms.
I have been a communicator most of my life, but it remains a struggle to find words that describe the unique character of PD pain. If you experience PD pain, please share your descriptors in the comments. Together we may find a common dialogue that will help others.
Don’t Miss: Is There A Test To Diagnose Parkinson’s Disease
