Q What Is The Role Of Depression In The Pain Experience In Pd
Dr. Fleisher: Depression is one of the most overlooked symptoms of PD, and it can affect over 30% of people with the disease at some point in their illness. I think there is a misconception that depression results from an adjustment disorder following diagnosis. While that may be partially true, patients with PD have alterations in various neurotransmittersincluding serotonin and norepinephrine in addition to dopaminethat predispose them to depression.
Depression is the primary factor related to quality of life in PD and is an independent risk factor for medication nonadherence. A physician could prescribe the most comprehensive regimen to control Parkinsons symptoms, including pain, but if depression symptoms are not being addressed simultaneously, the likelihood that that person is going to take that regimen is pretty minimal.
Given the link between depression and chronic pain, patients who are depressed should be screened for chronic pain and vice versa. In my practice, we screen every patient with the Unified Parkinsons Disease rating scale , which has both a patient-reported subjective component that includes questions about depression, pain, and altered sensation, as well as an objective component that includes a physical examination and questions about potential medication adverse effects . The patient fills out the subjective component every single time they come to the office.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinsons. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
It Can Sometimes Be The First Symptom Of Pd
According to a 1989 study published in the Journal of Neurology, Neurosurgery, and Psychiatry , roughly 43 percent of Parkinsons patients reported having shoulder complaints. A second study from 2015 published similar findings: 46 percent of their subjects with PD specifically experienced frozen shoulder.
Notably, the JNNP study also found that frozen shoulder was the first symptom of disease in 8 percent of their PD subjects, appearing up to two years before more traditional symptoms. Although it seems intuitive that immobilized patients in the later stages of their illness might have a high incidence of shoulder disturbances, we have been impressed that a number of our patients have experienced difficulties before other features of Parkinsons disease were recognized, the team wrote.
Read Also: Cleveland Clinic Parkinsons Bicycle Study 2017
Don’t Miss: Are There Any Cures For Parkinson’s Disease
Feet Exercises To Do At Home
Exercise 1
- Stand upright beside a chair or table, with your feet a few inches apart.
- Gently move your weight forwards, making sure your toes do not curl and your heels remain on the floor.
- Stay in this position for 5 seconds before moving back to upright. Again, keep your feet glued to the floor dont allow your toes to lift.
- Repeat this exercise a few times, forcing your feet to relax as your body is slowly moved over them in a controlled manner.
Exercise 2
- Sit on a chair and bring 1 foot up to rest on the other knee.
- Gently massage the soles of your feet in a long, steady stroke from the base of the heel to the end of each toe.
- Do this 5 times on each foot to stretch and loosen the skin, muscles and joints.
- If you have become stiff at the knees and hips, you may find getting into this position difficult.
- Its worth practising, but if its not possible, see if you can find a willing friend or family member to massage your feet for you!
Dont Miss: Mitochondria And Parkinsons Disease
Types Of Parkinson’s Pain
Most of the time, discomfort in muscles and joints is secondary to the motor features of Parkinsons lack of spontaneous movement, rigidity, and abnormalities of posture what is known as musculoskeletal pain. The most commonly painful sites are the back, legs, and shoulders and it is usually more predominant on the side more affected by parkinsonism.
But there are many other categories of pain associated with Parkinsons disease. Radicular or neuropathic pain is experienced as a sharp pain that can start in the neck or lower back with radiation to arm or leg respectively and is often associated with numbness or tingling, or a sensation of coolness in the affected limb. It is usually secondary to a pinched nerve due to something like a slipped disc.
Dystonia related pain occurs as its name suggests, at times of dystonia most often experienced in the foot, neck or face and arm at different points in the dosing schedule, particularly the off phase when there is not enough dopamine replacement but can uncommonly also occur at peak-dose times. It can be one of the most painful symptoms those with Parkinsons can face.
Akathisia pain is experienced as restlessness, a subjective inner urge to move, an inability to stay still and the inherent feelings of discomfort that it brings. It is primarily experienced in the lower limbs and can often be relieved by walking around.
Also Check: What’s The Difference Between Alzheimer’s And Parkinson’s Disease
Inflammation May Contribute To Both Joint And Nerve Degeneration
byNancy Walsh, Contributing Writer, MedPage Today June 9, 2021
Patients with osteoarthritis are at increased risk for developing Parkinsons disease, a longitudinal Taiwanese study found.
Incidence rates for developing Parkinsons disease were 0.99 per 1,000 person-years among patients with osteoarthritis compared with 0.71 per 1,000 for controls, reported Shin-Liang Pan, MD, PhD, and colleagues from the National Taiwan University in Taipei.
Accordingly, the risk among patients with osteoarthritis was 41% higher compared with controls, with an adjusted HR of 1.41 , the researchers wrote online in Arthritis Care & Research.
It is now recognized that inflammation plays a major role in the development of osteoarthritis, while neuroinflammation is characteristic of Parkinsons disease.
Because a growing body of literature reports that peripheral inflammation may induce neuroinflammation in the brain, leading to neurodegeneration, we hypothesized that having osteoarthritis may increase peoples risk of later developing Parkinsons disease, Pan and colleagues wrote.
Therefore, they analyzed data from Taiwans National Health Insurance system, which covers more than 97% of the population, identifying 33,360 individuals ages 50 to 64 who were diagnosed with osteoarthritis during the years 2002 to 2005, matching them by age and sex with the same number of controls.
- Knee or hip osteoarthritis, HR 1.55
- Non-knee or hip, HR 1.42
- Uncategorized, HR 1.32
Other Symptoms: Aging Or Pd
Because the biggest risk factor for developing PD is age , skeletal problems associated with aging are often experienced by people with PD. While it is not clear that PD increases the risk or even the severity of these other skeletal conditions, the problems of PD can make the symptoms of these conditions more prominent.
- Osteoarthritis, the joint damage associated with general wear and tear on the joints, is nearly universal in aging. Osteoarthritis tends to affect larger joints such as the hip and knee.
- Arthritis of the spine is also very common. This may contribute to the development of spinal stenosis, narrowing of the canal in the spine that houses the spinal cord. In severe cases, spinal stenosis causes damage to the nerves as they exit the spine or even to the spinal cord itself.
- Disorders of the fibrous discs between the bones of the spine can also cause pain, or limb numbness or weakness.
Read Also: Does Jesse Jackson Have Parkinson’s Disease
Fibromyalgia Vs Lupus Differences In Symptoms Pain Causes And Treatment
Fibromyalgia and lupus are two conditions that can cause pain, but its important to recognize the many significant differences between the two. Systemic lupus erythematosus , or lupus, is an autoimmune systemic disorder, which affects the joints, skin, and practically any organ in the body. Fibromyalgia affects the muscles causing pain, tender points, and extreme fatigue, and can contribute to anxiety or depression.
Both lupus and fibromyalgia are difficult to diagnose, and many patients with fibromyalgia are often wrongly diagnosed with lupus and vice versa. Furthermore, the two diseases can actually overlap one another, and there is a higher risk of rheumatic disease in fibromyalgia patients.
Fibromyalgia affects roughly two percent of the population and women are more likely to develop fibromyalgia than men. Estimates of lupus cases in the U.S. are 161,000 with definite lupus and 322,000 with definite or probable lupus. Like fibromyalgia, lupus often affects women more than men, too.
Also Check: Judy Woodruff Health Problems
Static And Dynamic Psychophysical Paradigms
So-called static psychosocial paradigms refer to a range of quantitative sensory testing protocols, which were recently standardised and defined by the German research network on neuropathic pain . In addition to sensory detection thresholds the DFNS protocol involves pain thresholds to thermal and mechanical stimuli. If QST responses are incongruous to normative reference values the dysfunction may be located anywhere along the neural axis, from peripheral nerve fibres,, to the spinal cord and cortical areas. However the value of QST to distinguish central and peripheral mechanisms is limited. Nociceptive withdrawal reflex thresholds offer a measure of central pain processing, specifically spinal nociceptive facilitation.
Read Also: What Part Of The Brain Does Parkinsons Affect
You May Like: Does Parkinson’s Qualify For Disability
How Is Pain Treated In Patients With Parkinson Disease
Pain serves as 1 of the most frequent nonmotor complaints in patients with Parkinson disease , affecting 68% to 95% of patients across all clinical stages. Published in the Journal of Parkinson Disease, researchers highlight that similar to PD, pain is complex and even has different classifications of subtypes within the disease.
While prominent, real-life pain data in PD remains scarce. Researchers sought to provide an overview on pain in PD, including classification, assessment, presentation, and the existing therapy landscape.
As researchers highlighted, todays classifications of pain in PD include musculoskeletal, radicular/neuropathic, dystonia-related, akathic discomfort/pain, and central pain. Notably, the difference in pain directly related to PD and central pain, which is attributed to objective painprocessing and pain-perception disturbance within ascending and descending pathways, was referenced. Most frequently, pain presents as musculoskeletal/nociceptive pain in PD patients, but in nearly half of the PD population, comorbid conditions, such as spine and joint arthrosis, serve as contributors.
When it comes to treating pain in PD, interventions remain a major unmet need as only approximately 50% of those with the disease receive at least some type of pain therapy. In managing pain, researchers recommend that therapy should be optimized to address dopaminergic issues, which has been shown to be effective in 30% of patients with PD.
Reference
Calf Stretches For Parkinsons
Seated Option: Calf Stretch with Strap
Standing Option: Wall Push-offs x 20
*To increase the intensity of the stretch, back away from the wall until you reach a distance where you feel a strong stretch in your calves when youre leaning forward against the wall. Be sure to keep your heels down throughout the exercise.
Recommended Reading: Parkinson’s Disease Equipment To Assist With Daily Living
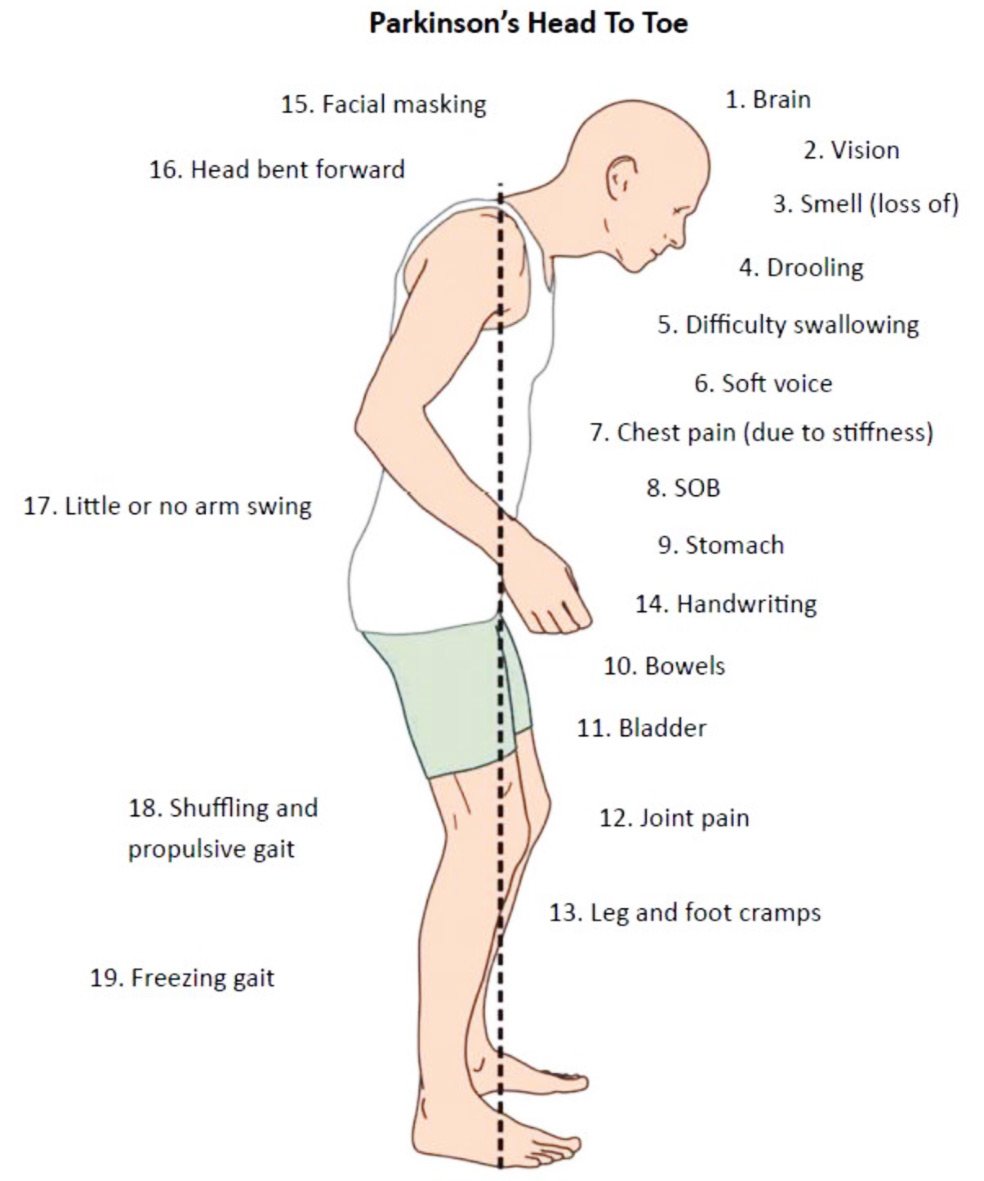
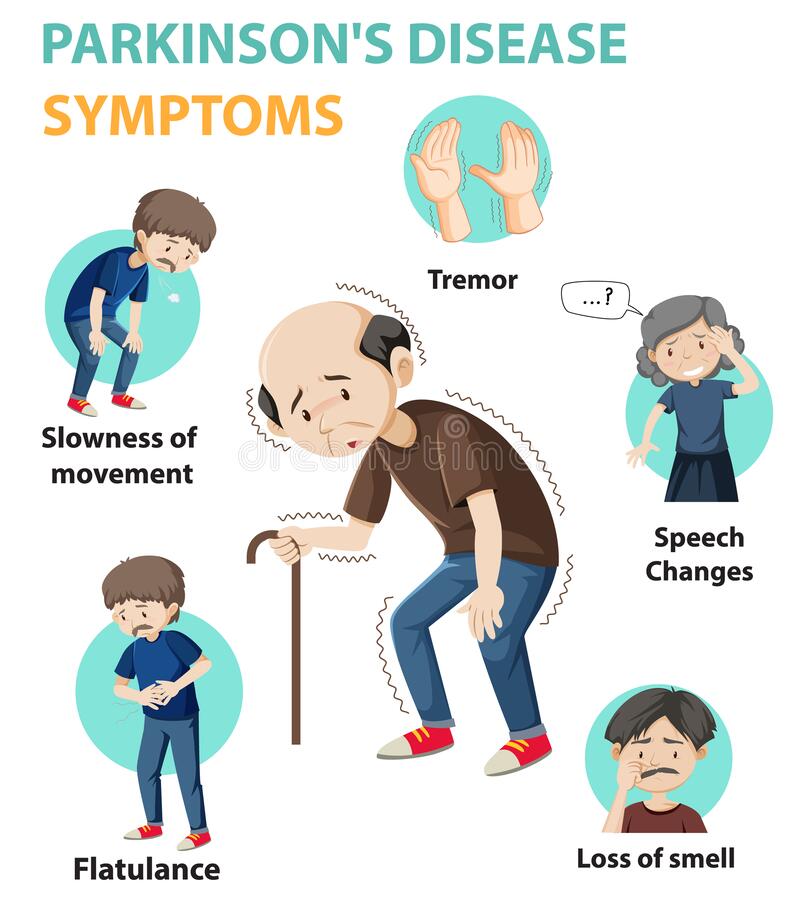
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
Parkinsons Disease And Its Accompanying Symptoms:
Parkinsons Disease is a progressive disease that affects the central nervous system and the ability to coordinate movement in the body. Since Parkinsons Disease affects many areas of the brain, symptoms can vary in individuals and progression can be either mild, moderate, or aggressive. Physical therapy, occupational therapy, and speech therapy are essential for people with Parkinsons Disease.
Parkinsons Disease typically affects ones ability to walk, with slower movements and difficulty with starting or stopping walking. In addition, movements tend to become slower, and it is common for tremors to develop in the hands. Muscles can become quite rigid, leading to loss of motion and poor posture. A dangerous symptom is called retropulsion, where the tendency of an individual is to fall backward with little to no ability to protect oneself.
Speech can also be affected with Parkinsons Disease, becoming slurred and slow, due to poor activation of the mouth, tongue, and throat muscles. In addition, eating and drinking can become challenging due to difficulty with swallowing.
Also Check: Are Diabetes And Parkinson’s Related
What Is Parkinsons Disease
Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
Mechanisms That Contribute To Persistent Pain In Pd
As the field progresses psychophysical testing has the potential to advance our understanding of persistent pain in PD by elucidating the mechanisms which underlie pain in PD, and in doing so, identifying subgroups of patients with susceptibility to developing persistent pain while assisting in the development and monitoring of personalised pain management strategies for these patients.
Recommended Reading: Eye Test For Parkinsons Disease
Read Also: How To Slow Parkinson’s Disease
Pain Is An Unfortunately Common Problem In Parkinsons Disease
Of course, pain is common in the general population, especially among older people. A recent American study found that pain affected about twice as many people with Parkinsons Disease than those of the same age and gender without PD. About 50% of Parkinsons Disease patients in that study suffered from painful disorders. Men and women seem to be about equally affected. A very well described scenario is the patient who is followed for a painful frozen shoulder for a year or so before a tremor develops leading to a diagnosis of PD. Pain clearly plays a major role in quality of life. Everyone with chronic pain enjoys life less, leading to a vicious cycle in which pain causes depression or isolation which in turn leads to more pain.
Parkinson patients suffer from the same pain problems that other people have, often amplified by the motor dysfunction, but they also have additional pain problems which are unique to PD.
One recent review classified the types of pain Parkinsons Disease patients have into: musculoskeletal, in which the pain results from problems with the muscles , bones or joints dystonic, which is due to abnormal muscle contractions caused by the Parkinsons Disease or the medications used to treat it radicular pain, which is feels like the pain caused by pinched nerves central pain, which is presumed due to abnormalities in the brain, and is a continuously present pain that cannot be explained otherwise and discomfort related to an unpleasant urge to move.
What Causes Pain In Cases Of Parkinsons Syndrome Sufferers
Parkinsons Syndrome Sufferers may present with various combinations of back, buttock and leg pain, numbness and muscle weakness, Symptoms are often aggravated by an abnormal asymmetrical gait arising from loss of spatial awareness muscle spasm and loss of limb control. The back pain may arise from irritation within the disc wall but more commonly arises from the pinching of the trapped nerve in the exit doorway from the spinal column. The foramen may be distorted and the nerve is tethered by years of scarring reaction to repetitive bruising, can not evade the pinching by the bulging distorted disc wall or overriding facet joints . The disc may be degenerate and bulging and contribute to the irritation of the tethered nerve. When advanced the compression causes numbness and weakness to develop. The patchy weakness or spasm of the muscles controlling the spinal segments results in asymmetrical loss of control or stiffness of the disc levels and aggravation of the effects of the local pathology at each level and aggravation of symptoms arising at these levels.
You May Like: Grants For Parkinsons Sufferers
Read Also: Does Parkinson’s Cause Pain

