Falls Can Be Prevented With Appropriately Prescribed Exercise In People With Mild To Moderate Pd
Physiotherapy aimed at preventing falls in people with PD should consider the individuals risk of falls and their fall risk factors. A systematic review showed that exercise reduces the frequency of falls in PD by 60 per cent . However, detailed investigation of randomised controlled trials indicates that when exercise is semi-supervised , falls are reduced in people with milder disease , but are increased in those with more advanced disease .
It is recommended that physiotherapists use the three-step clinical prediction tool to quickly and accurately predict an individuals probability of falling in the next six months as low , moderate or high . People with a low to moderate risk are suitable for group or semi-supervised physiotherapy that targets their remediable fall risk factors commencing as soon as possible after diagnosis.
Evidence is scant regarding intervention for people with high fall risk. However, a carefully monitored multidisciplinary approach, including medical review and higher levels of exercise supervision, along with environmental and behavioural modifications, is suggested.
Health Economic Evidence Statements
The found no significant difference in mean increase in annual costs between groups from the year before the study to the second year of the study. This mean annual cost estimated the provision of nurse care to cost £200 per person per year and excluded the cost of apomorphine. The mean annual cost in the specialist nurse group increased from £4,050 to £5,860 and from £3,480 to £5,630 in the group based on 1,859 people from 438 general practices in nine randomly selected health authority areas of England.
It is not always clear whether care is substituting some or all of the consultant care or is serving as additional care. By varying the cost-savings of other health professional costs by PDNS care, costs for 1 year of PDNS care range from an additional cost of £3,289 to cost-savings of £4,564. Full details of these analyses are shown in .
Why Big Is Better
BIG has one primary focus: amplitude. It asks those following the program to move big, encouraging a vigorous range of movement and pushing participants to use all parts of the body, from the feet to the hands and fingers. In a BIG session, the patient mimics or mirrors the therapist through a series of large stepping or rocking movements with their arms moving in various directions.
In recent studies, the principles of LSVT BIG were applied to limb movement in people with Parkinsons disease. The documented results demonstrated improvements in amplitude that generalized to improve speed , balance, and quality of life. In addition, people were able to maintain these improvements when challenged with a dual task.
At Progressive Physical Therapy, our programs are designed to meet the individual needs of the patient and their ability in a safe and fun manner. This, combined with doing a home exercise program one to two times a day helps clients with Parkinsons Disease improve their skills. The goal is for patients to use their bigger movements automatically in everyday living and for long-term carryover of increased amplitude. The therapy can be used in a walking, standing or sitting position.
Don’t Miss: When Was Muhammad Ali Diagnosed With Parkinson’s Disease
What Other Services Does Physical Therapy Provide
Recommendations. A physical therapist can make recommendations for physical therapy at home, at an outpatient facility, or at a nursing or rehabilitation facility.
Work capacity evaluations. Many physical therapists can perform functional capacity evaluations to provide more information for disability claims based on physical performance. This functional capacity evaluation can be useful when the Social Security office denies disability to a person who is unable to work for an eight-hour day.
Data Collection And Management
Patients will be given a unique personal identification code not containing any information that refers back to the individual. The key file connecting personal identification codes to the individual patient will be stored on a secure Radboudumc data server. Only the research team has access to this key. The key file will be stored on a different server from the one with acquired study data for 5 years, allowing the research team to contact patients after they have finished the study. After 5 years, the key file will be destroyed.
Data from all paper-based case report forms completed by the researcher will be entered manually into an online certified data management system . Online CRFs will automatically be recorded in Castor EDC. When patients or caregivers are not able to complete questionnaires online, they also have the opportunity to do this on paper. We will send out the questionnaires by post, and patients can return the completed questionnaires using a self-addressed envelope. These questionnaires will be entered manually into Castor EDC. Both online and paper-based CRFs only contain the personal identification code.
Clinical notes taken by the PDNS in the online study report will also not contain any information that refers back to the individual. PDNSs are instructed to make notes according to a predefined structured format without mentioning personal information that traces back to an individual patient. The study report will be completed in Castor EDC.
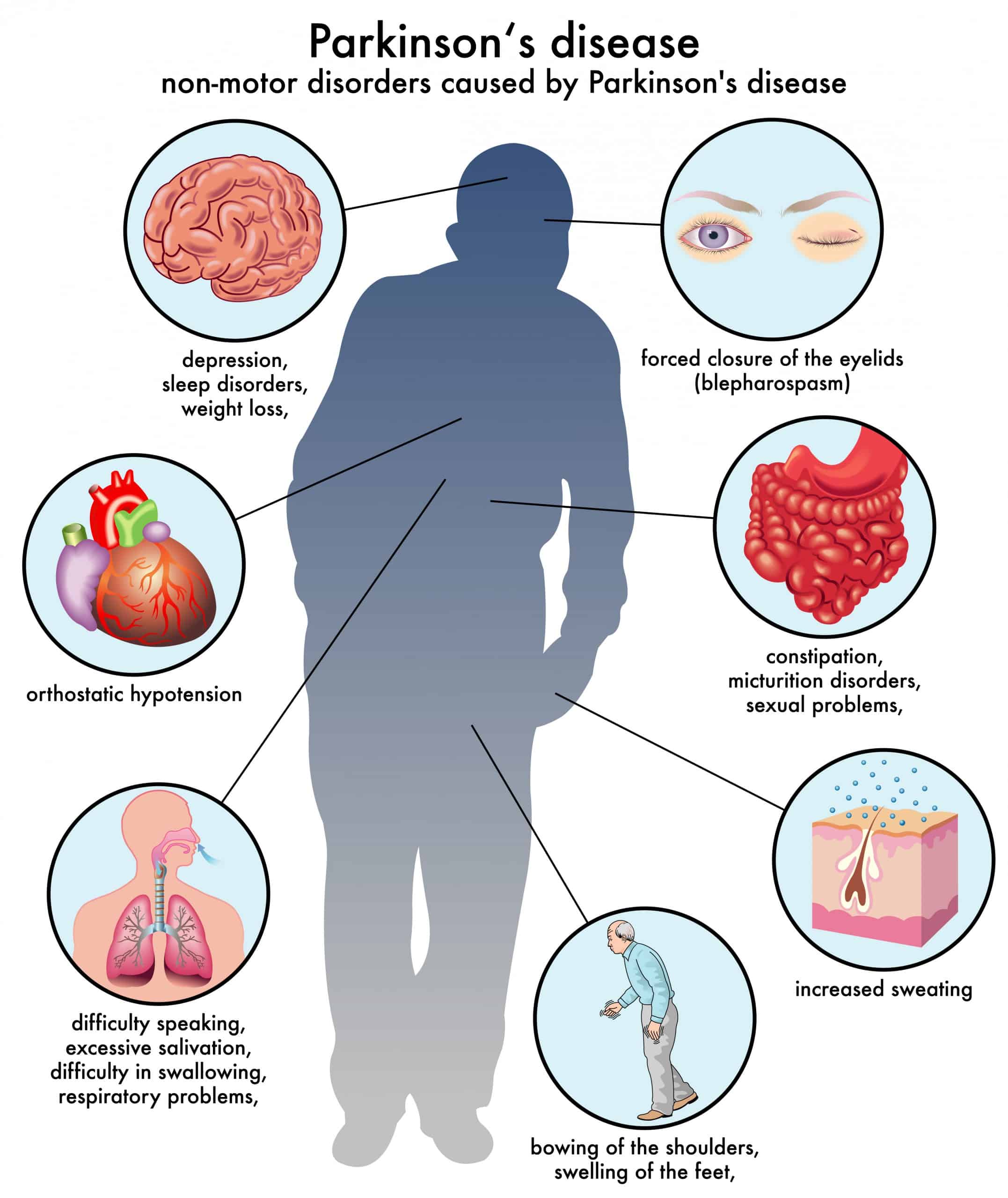
You May Like: How Does Parkinson’s Disease Affect Your Body
How Can Physical Therapy Help Parkinson’s Disease
Physical therapy is an important part of a treatment plan for Parkinson’s disease. It aims to help individuals with Parkinson’s disease remain active and independent as long as possible. According to a recent meta-analysis, physical therapy significantly improves symptoms related to motor skills. The Parkinson’s Foundation states that increasing physical activity to 2.5 hours a week or more can help people with Parkinson’s disease maintain their quality of life.
Overall, physical therapy can help with the following:
- Increasing endurance
Because physical therapy improves motor skills and decreases pain, you can expect it to help with many of your regular activities, such as getting up from a chair, climbing stairs and getting into and out of a car.
Physical therapy can also improve other symptoms associated with Parkinson’s disease, such as depression, anxiety and fatigue. Lastly, it can help with other health issues that impair mobility, like joint pain.
Doctors recommend beginning an evidence-based physical therapy program as soon as possible. Exercise can induce neuroplasticity, or the brain’s ability to change in response to behavioral changes. When you begin physical therapy, your brain learns new ways to move and think. Exercise also helps brain cells stay healthy. In other words, physical therapy may slow the progression of Parkinson’s disease.
Feasibility And Preliminary Effectiveness Design Of The Empower
Study design and settings
This 12-week pilot for a randomized clinical trial will assess the feasibility and preliminary effectiveness of the EMPOWER-PD and make comparisons with conventional physical therapy . The EMPOWER-PD intervention protocol was developed according to template for intervention description and replication checklist . The study protocol was described according to the SPIRIT guideline , and its feasibility will be analyzed according to the aspects mentioned in the CONSORT checklist for pilot and feasibility clinical trials . The research project was submitted to the University Research Ethical Review Board of the Santa Catarina State University , Florianópolis, Santa Catarina, Brazil, according to the terms of Resolution 466/2012, and approved under report n° 2.145.010. The trial was registered on ReBECBrazilian Registry of Clinical Trials: Rio de Janeiro : Scientific Information and Technologic in Health Institute Registry name: A Physiotherapy protocol based on the preferences of the individual with Parkinson Disease for health empowerment, Identifier RBR-7ZBXQ5, Registered 18 August 2017, .
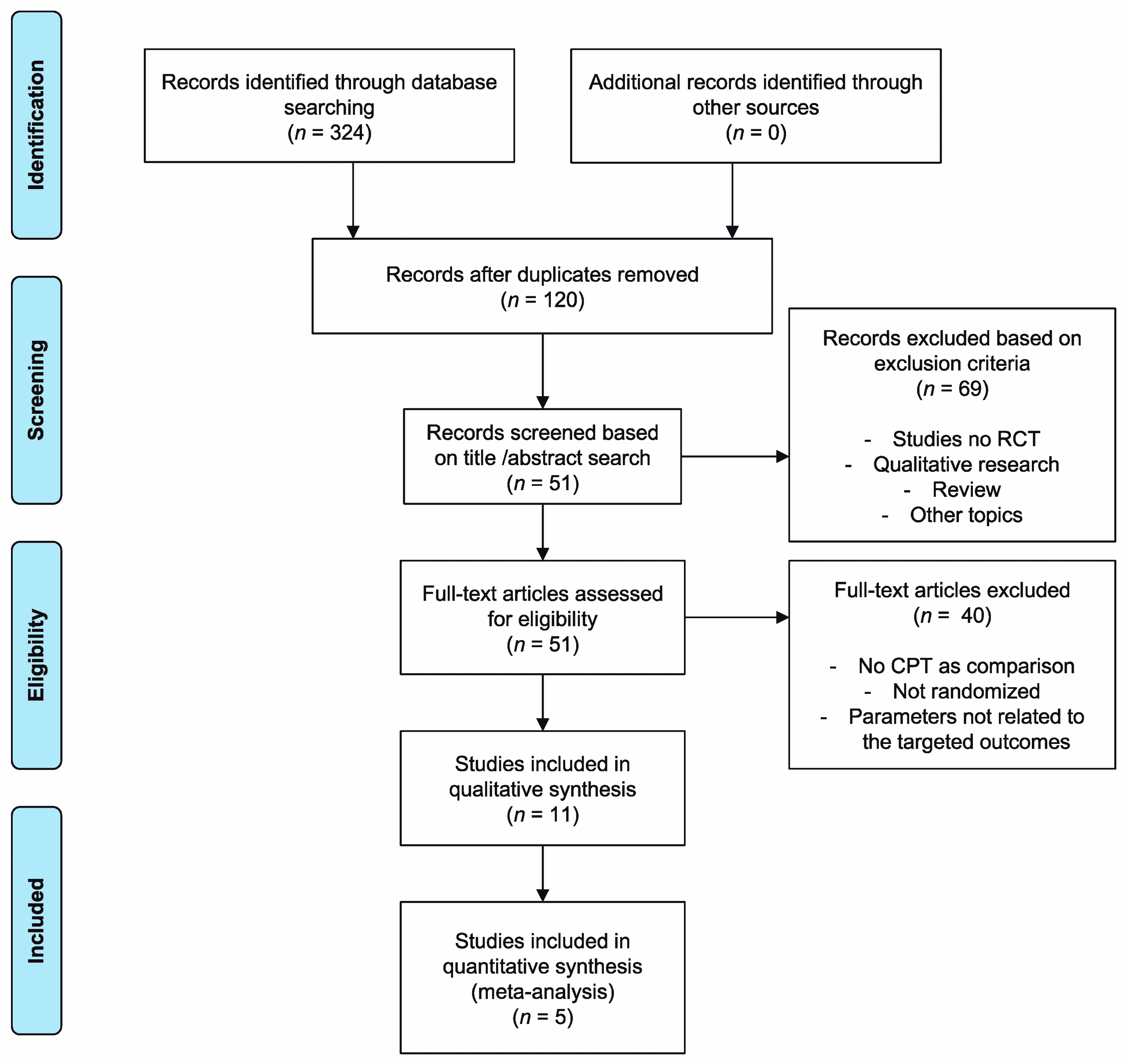
Fig. 1
Sample size
Randomization
Participants
Read Also: What Is Focused Ultrasound For Parkinson’s
How Does Physical Therapy Help Parkinson’s Disease
Physical therapy cannot cure Parkinson’s disease, because at this time, neurological damage cannot be reversed. But therapy can help you compensate for the changes brought about by the condition. These “compensatory treatments,” as they’re called, include learning about new movement techniques, strategies, and equipment. A physical therapist can teach you exercises to strengthen and loosen muscles. Many of these exercises can be performed at home. The goal of physical therapy is to improve your independence and quality of life by improving movement and function and relieving pain.
Physical therapy can help with:
- Balance problems
Important note: Some physical therapists may apply diathermy to relieve muscle aches and pains. This could be dangerous to patients who have deep brain stimulators.
Promoting Physical Activity And Preventing Falls
Because PD is a chronic progressive disorder, it is probable that sustained exercise is necessary to maintain benefits. Indeed, follow-up data from a number of human exercise interventions have demonstrated a gradual return to baseline abilities after the supervised intervention is finished.7,25,38
Because weekly intervention with a physical therapist, throughout the entire course of PD, is neither realistic nor desirable, patients need to take responsibility for their physical activity and exercises. Methods have been developed, based on theories of behavior, for improving exercise habits. Strategies include exploration of the patient’s beliefs about exercise and barriers to regular exercise and discussing the possibility of looking at things differently to change beliefs and overcome barriers.4345 Together, the clinician and patient then establish reasonable goals that the patient thinks are attainable they build on those goals as exercise habits improve. Regular follow-up appointments also are important to monitor progression and provide support to the patient.
You May Like: How To Treat Constipation In Parkinson’s Disease
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
Risk For Falls And Injury
With Parkinsons disease, bradykinesia, rigidity and tremors can lead to gait problems and a risk for falls and injury.
The nursing assessment includes evaluating the patients movement and gait and understanding his/her home environment. Improving movement and gait can reduce the risk of falls .
To promote safety and avoid falls, suggest removing potential hazards in the home, such as loose rugs or obstacles in pathways.
Recommend handrails on both sides of stairways, non-skid surfaces and grab rails in showers and tubs, and raised toilet seats. Suggest that patients with PD wear appropriate shoes with smooth, non-slippery soles. Encourage the family or caregiver to supervise ambulation, as needed. A bedside urinal or commode may be helpful for some patients to prevent nighttime falls.
Some patients with Parkinsons disease experience orthostatic hypotension. If patients become dizzy when moving from a lying to a standing position, teach them to rise slowly, to remain seated for a few minutes with legs dangling over the side of the bed and ex feet upward, then to stand, sitting back down immediately if they feel dizzy. Recommend having someone with them when they stand up.
Review medications, as some anti-Parkinsons drugs may cause dizziness these can be discussed with the physician to see if alternative medications might be beneficial.
Dont Miss: On Off Phenomenon
Don’t Miss: Solutions For Parkinson’s Disease
Nursing Care Plan For Parkinsons Disease 6
Nursing Diagnosis: Deficient Knowledge related to lack of knowledge about Parkinsons disease, difficulty understanding the disease process, lack of coping skills, and cognitive impairment secondary to Parkinsons disease as evidenced by verbalization of questions and incorrect information from the patient and family, presence of preventable complications, and inappropriate behavior.
Desired Outcomes:
- The patient and the patients family will be able to express an accurate understanding of the disease process, medication regimen, and treatment plan of care for Parkinsons disease.
- The patient will be able to fulfill the medication regimen and will notify the physician if the patient experiences unusual side effects.
- The patient will be able to prevent injury by demonstrating safety precautions.
- The patient and the family members will identify the need for long-term goals and the potential for end-of-life decisions to be done.
Training Of Trial Therapists
Before the start of the trial, the participating occupational therapists follow a three-day training to inform them about the study procedures and to train them to treat the patients and caregivers according to the OTiP intervention protocol. Special attention is given to enhancing the therapists skills in coaching and motivational interviewing and in eliciting and collaboratively defining meaningful, individualized goals with the patient and caregiver. Ways to achieve sufficient treatment intensity in ten weeks are discussed. Halfway through the inclusion period a booster training session is planned. Therapists can use a secure online platform to share issues and experiences and can consult an expert OT to discuss the intervention.
Recommended Reading: Parkinsons Off Time Symptoms
Also Check: How To Get Checked For Parkinson’s Disease
Inclusion And Exclusion Criteria
The inclusion and exclusion criteria for patients are kept purposefully broad in order to represent the full diversity of the PD spectrum and thus generate results that apply to real clinical practice. All patients with PD, regardless of disease severity or disease duration, male and female, aged 18years or older at the time of PD diagnosis are eligible. We will only exclude patients for the following reasons:
-
Lack sufficient knowledge of the Dutch language to complete questionnaires
-
Have received care from a PDNS in the past 2 years
-
Have a score < 18 on the Mini Mental State Examination and < 12 on the Frontal Assessment Battery
-
Have a type of atypical parkinsonism caused by medication , a metabolic disorder , encephalitis, or a neurodegenerative disorder
-
Residing in a nursing home or another type of residential care facility
-
Have any other medical or psychiatric disorder that, in the opinion of the researcher, may compromise participation in the study
Dont Miss: Similar To Parkinsons
Search Strategy And Selection Criteria
A systematic search of the literature to the end of January 2012 was undertaken using a highly sensitive search strategy as recommended by the Cochrane Collaboration. We combined text and, where appropriate, Medical Subject Heading terms for physiotherapy, physical therapy, exercise, or rehabilitation and Parkinson, Parkinsons disease, or parkinsonism. No language restrictions were applied. We identified relevant trials by electronic searches of general biomedical and science electronic databases , rehabilitation databases English language databases of foreign language research and third world publications conference and grey literature databases , and trial registries . We also hand searched relevant general and specific journals , abstract books, and conference proceedings , as well as examined the reference lists of identified papers and other reviews.
Recommended Reading: Parkinson’s And Foot Cramps
Can You Apply The Results Of The Systematic Review To Your Own Patients
On the basis of the patient-intervention-comparison-outcome analysis, the results of the Cochrane review can be applied to patients such as Mr Jennings. Clinicians should, however, consider several limitations of the data. First, the outcomes were related to gait and balance but not to overall functional ability. This fact is important because improvements in gait do not necessarily lead to improvements in basic activities of daily living, such as dressing and hygiene, or overall household activities, such as cooking, cleaning, and managing laundry. Second, only short-term outcomes were examined. Parkinson disease is a progressive condition, and although short-term benefits are important, true benefits may be realized only if the patient develops the skills and strategies for long-term adherence to appropriate exercise and activity. Data regarding the best strategies for assisting patients in developing appropriate activity and long-term exercise habits are needed.
Furthermore, evidence is not yet available to determine the best intervention strategies on the basis of subgroups of PD or H& Y stages of PD. Finally, many patients have substantial comorbid conditions that should be taken into account in the design of a plan of care, both because of safety implications and because they can contribute to deficits in movement and function.
How Can Occupational Therapy Help People With Parkinsons Disease
Occupational therapists can work with people with Parkinsons Disease and their families to provide advice, support and guidance during their journey. For some they may require advice on a specific item of equipment whilst for other clients we are involved in more substantial home modifications and support as their needs change with the progressing condition. Below are some ways that an occupational therapist can help:
How we can help
We aim to solve the difficulties associated with Parkinsons Disease. Some of the common ones we treat are listed below.
Also Check: How Does Parkinson’s Cause Death
Physical Therapy For Parkinsons Disease
Its well-known that exercise of all kinds is beneficial for patients with Parkinsons disease. But physical therapy, in particular, is key. Why? A professional can guide you through the right moves to increase mobility, strength and balance, and help you remain independent, says Denise Padilla-Davidson, a Johns Hopkins physical therapist who works with patients who have Parkinsons. Here are things a therapist may work on:
Note: Please discuss any exercise program with your physician/neurologist and get a referral to a physical therapist or trainer with expertise in Parkinsons disease before starting any specific program.
When To Find A Physical Therapist
Physical therapists can be helpful at all stages of PD. Movement impairments in the early stages of the disease may not be obvious. Talk to your doctor about getting a baseline physical therapy evaluation and then continue with periodic re-evaluations.
According to the Parkinsons Outcomes Project, the largest clinical study of Parkinsons disease through our Global Care Network, increasing physical activity to at least 2.5 hours a week can slow decline in quality of life. The Parkinsons Foundation has identified specific care approaches associated with better outcomes across people who seek expert care at our designated Centers of Excellence. Among others, best practices include early referral to physical therapy and encouragement of exercise as part of treatment.
Recommended Reading: Can Lead Poisoning Cause Parkinson’s
