In A Sense The Certainty Of Diagnosis Was Good I Belonged Somewhere
Post-misdiagnosis
I still have no confirmed diagnosis. The swathe of neurological symptoms still persist today some aspects of movement are identified as functional movement disorder, but otherwise it has been a question of ruling in/out alternative causes for some symptoms.
One theory is that an initial brain insult during the 2006 anaesthetic, together with a gastro drug I was taking at the time that has Parkinsonism as a side effect, combined to give me Parkinsons disease. But now this original brain insult plus nine years of my brains neuroplasticity being driven into new behaviours by Parkinsons drugs, plus issues that arose during Parkinsons drug withdrawal are the current neurological problems that I have to contend with.
Fortunately, while there is widespread dysfunction, I have been told that there does not appear to be any brain disease processes associated with these symptoms. Again, there are no tests to prove/disprove this and one remains reliant on the expertise of brilliant neuroscientists.
Patients With A Previous Diagnosis Of Parkinson’s Disease
The diagnosis of probable Parkinson’s disease was confirmed in 109 of the 131 patients with this diagnosis , including three in whom atypical features were found but were insufficient to invalidate the diagnosis of Parkinson’s disease . Two additional patients were found to have possible Parkinson’s disease. However, in 20 of the 131 patients the diagnosis of Parkinson’s disease was unequivocally rejected . The alternative diagnoses were non-parkinsonian tremor in four patients , vascular parkinsonism in six , progressive supranuclear palsy in four , and multiple system atrophy in three . Two patients received a diagnosis of idiopathic torsion dystonia, and one of dementia without parkinsonism. When only those patients who had seen a specialist at some point in the past were considered, the diagnosis was changed from Parkinson’s disease to a different diagnosis in 11%.
Patients with an initial diagnosis of Parkinson’s disease
Testing For Parkinsons Disease
There is no lab or imaging test that is recommended or definitive for Parkinsons disease. However, in 2011, the U.S. Food and Drug Administration approved an imaging scan called the DaTscan. This technique allows doctors to see detailed pictures of the brains dopamine system.
A DaTscan involves an injection of a small amount of a radioactive drug and a machine called a single-photon emission computed tomography scanner, similar to an MRI.
The drug binds to dopamine transmitters in the brain, showing where in the brain dopaminergic neurons are.
The results of a DaTscan cant show that you have Parkinsons, but they can help your doctor confirm a diagnosis or rule out a Parkinsons mimic.
Conditions That Mimic Shuffling Gait Seen In Parkinsons:
Please read the article on shuffling gait. It describes 5 causes of shuffling of gait.
The most crucial mimic to remember is Normal Pressure Hydrocephalus .
The person with NPH feels like he is stuck to the ground. This is a magnetic gait. It is easy to mistake this for Parkinsons disease.
For example, see this video posted by the Hydrocephalus Association of America on youtube:
NPH can be treated by implanting a small shunt pipe. This shunt drains excess water around the brain into the abdomen.
How Is Parkinson Disease Diagnosed

Parkinson disease can be hard to diagnose. No single test can identify it. Parkinson can be easily mistaken for another health condition. A healthcare provider will usually take a medical history, including a family history to find out if anyone else in your family has Parkinson’s disease. He or she will also do a neurological exam. Sometimes, an MRI or CT scan, or some other imaging scan of the brain can identify other problems or rule out other diseases.
What Health Conditions Mimic The Symptoms Of Parkinson’s Disease
Parkinsonism is a medical term that refers to the symptoms experienced by people with the disease, which include slowness of movements, stiffness of the joints, as well as tremor and imbalance. However, there are a series of conditions whose symptoms are very similar to those of Parkinson’s disease, which is why so many people are misdiagnosed.
Being aware of these health conditions is essential if you have a history of exposure to paraquat, as it may facilitate the assignment of a correct diagnosis. The following are some of the conditions that mimic the symptoms of Parkinson’s disease:
If you have a history of exposure to paraquat and were diagnosed with one of the above conditions, we strongly advise you to seek a second opinion from a specialist, as you may be in fact struggling with Parkinson’s disease, which qualifies you for compensation.
It is essential to receive a correct and precise diagnosis, as it will not only help you obtain the money you deserve from the liable companies but will also improve your quality of life.
For over 35 years, the team of experts at Atraxia Law has been helping people recover the compensation they were eligible for by evaluating their personal injury or product liability claims and are ready to provide you with quality assistance as well if your health was affected by exposure to paraquat.
So What Is It Is It Parkinsons Disease Or Is It Something Else
The answer is not easy, but many who feel they have more than Parkinsons may in fact have multiple system atrophy .MSA is a very rare disorder that has similarities and features of Parkinsonism.However, it is so rare that many physicians are unfamiliar with it and so the diagnosis is not considered. As a result, a likely diagnosis of MSA might be delayed by years and even missed all together. Whats more, due to many symptoms that could possibly be attributed to other conditions diagnosing MSA can be challenging, even to the most experienced doctors. This can be very frustrating to those who know it is more than PD.
Myth 1: Parkinsons Is Only A Motor Condition
Fact: While its true that Parkinsons disease symptoms include shaking and tremor, rigid muscles, slowness of movement, and a frozen or flat expression, its a lot more than that.
Nonmotor symptoms deserve and are getting more attention from doctors and researchers. These symptoms include cognitive impairment or dementia , anxiety and depression, fatigue, sleep problems and more.
For some patients, nonmotor symptoms are more disabling than motor symptoms, which are the focus of treatment. Be sure to talk to your doctor about other issues so you can get all of your symptoms addressed.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Parkinsons Disease Symptoms Of Dementia
Up to one-third of people living with Parkinsons disease experience dementia, according to the Parkinsons Disease Foundation. Problems with dementia may include trouble with memory, attention span, and what is called executive function the process of making decisions, organizing, managing time, and setting priorities.
RELATED: 12 Famous People With Parkinsons Disease
Parkinson’s Misdiagnosis: Pinched Nerve
Pinched nerves do affect your bodys ability to send internal messages. This usually causes joint pain and can lead to a lack of limb or joint mobility. However, this does not align with most other PD symptoms.
A pinched nerve in my neck.
My doctor said I had a pinched nerve and degenerative discs in my neck, which were causing my arm to basically not move. Then my driving foot started to not work. I grew tired of not getting answers, so went for an extensive stay at the Mayo Clinic and now have a great doctor at UCLA.
Patients In Whom A Diagnosis Of Parkinson’s Disease Was Or Was Not Previously Made
Patients in whom a diagnosis of Parkinson’s disease was previously made had a longer disease duration and greater disease severity , with more severe akinesia , postural instability, and rigidity than those in whom the diagnosis was not made before. They were also more likely to be depressed , to have experienced dyskinesias , and to live alone or with their family than in a nursing home .
Confusion With Essential Tremor
The tremor of Parkinsons disease is often confused with the tremor of a condition called Essential Tremor, or Benign Familial Tremor . Katherine Hepburn had Essential Tremor, and was originally misdiagnosed with Parkinsons. Ronald Reagan also had Essential Tremor. Both had a head tremor and a vocal tremor. In Essential Tremor, the hands are most commonly involved, followed by the head and then the voice. Essential Tremor can also cause the jaw to tremor, and it may be difficult to figure out if a jaw tremor is from Essential Tremor or Parkinsons. Unfortunately, some people may have both disorders. Some authorities believe that there is, in fact, an increased association between the two conditions, so that more people with Parkinsons disease have Essential Tremor than would be expected by chance alone, but this has not been established.
Parkinson’s Disease Is Often Misdiagnosed In People With Paraquat Exposure
Because the symptoms of Parkinson’s disease are very similar to those of other health problems, it is often misdiagnosed in people with a history of exposure to paraquat, which prevents victims of toxic exposure from recovering the financial compensation they deserve. According to medical studies, Parkinson’s disease is misdiagnosed in up to 30% of cases and the rate of misdiagnosis is even higher in people whose disease is in the early stages. 1 in 4 people with Parkinson’s disease will receive a wrong diagnosis
Therefore, seeking a second and even a third opinion is essential in being assigned a correct and accurate diagnosis. It is a known fact that frequent exposure to paraquat in agricultural workers increases the risk of developing Parkinson’s disease by 250%.
Thereby, if you have a history of paraquat exposure, it is crucial to keep a close eye on your health for the symptoms of Parkinson’s disease.
A poll from the American Journal of Managed Care found that over 26% of people with Parkinson’s disease were initially misdiagnosed and 21% had to see their general healthcare provider 3 times before being referred to a specialist to have their health problem correctly diagnosed.
What is more alarming is that 48% of the participants received treatment for the wrong health condition, with 36% being prescribed medication and 6% undergoing surgical procedures. Consequently, a significant decline in the quality of life was noted in the misdiagnosed patients.
Why It Is Hard To Detect The Progression Of Parkinsons Disease
As we stated above that Parkinsons disease is not basic, it becomes difficult to detect it in its early stage due to 2 symptoms it affects motor issues such as the rigid muscles and tremors, and the other is the development of non-motor symptoms such as dementia, pain, and loss of smell.
Although one cannot see that a person suffering from Parkinsons disease will show all the symptoms, you cannot even tell or predict which symptoms will be present and their severity. For instance, one patient may show severe dementia with slight tremors. Another patient displays a critical condition of tremors but does not have any problem related to memory or thinking. In another case, the patient can show a severe state of all the symptoms. Therefore, it is difficult to predict the progression of the condition.
In addition to this, the medicines that help in treating Parkinsons disease also make it difficult to predict the results because a few patients show positive results while others do not show any improvement.
Conditions That Can Cause Tremors Besides Parkinsons:
The tremor of Parkinsons disease occurs even at rest. Hence it is called a rest tremor. Very few other conditions produce rest tremor.
But, many other diseases produce a tremor which is seen only when moving, for example when writing. This is called an Action tremor or posturokinetic tremor. Even these diseases are sometimes misdiagnosed as Parkinsons disease.
| Causes of Rest Tremor |
|---|
|
2. Excessive stress, coffee or smoking 3. Medications such as bronchodilators, valproate and lamotrigine 4. Chromosomal problems such as Fragile-X syndrome 5. Parkinsons disease itself! And many others |
What Makes Them Different
MS and Parkinsonâs have different causes. They usually start to affect you at different ages, too.
MS often affects people between ages 20 and 50, but children get it, too. Parkinsonâs usually starts at age 60 or older, but some younger adults get it.
MS is an autoimmune disease. That means your bodyâs immune system goes haywire for some reason. It attacks and destroys myelin. As myelin breaks down, your nerves and nerve fibers get frayed.
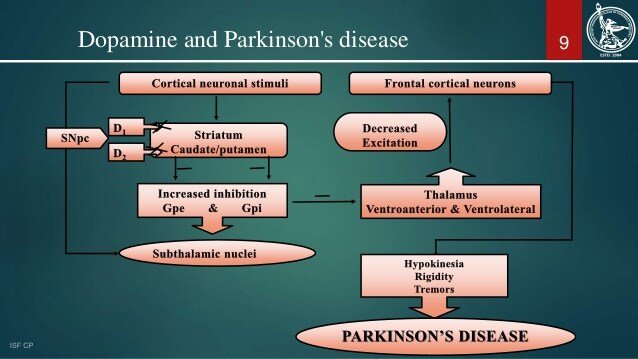
In Parkinsonâs, certain brain cells start to die off. Your brain makes less and less of a chemical called dopamine that helps control your movement. As your levels dip, you lose more of this control.
Some genes may put you at risk for Parkinsonâs, especially as you age. Thereâs a small chance that people who are exposed to toxic chemicals like pesticides or weed killers can get it, too.
These symptoms are more common if you have MS. They not usually found in Parkinsonâs:
What It Looks Like:
You feel a general level of physical or mental exhaustion that stretches beyond normal tiredness. Just starting any workout is an accomplishment due to your utter lack of energy and motivation. When you do manage to exercise, youre wiped out. You may notice walking seems incredibly difficult, due to heaviness in your legs or extreme freezing. Exercise is such an endeavor that youre tempted to just avoid it altogether.
Is It Possible That Youve Received A Parkinsons Misdiagnosis
Learn from the elder care team in Marin County about a common cause of Parkinsons misdiagnosis.
Every year, thousands of American seniors are told they have Parkinsons disease when they actually have received a Parkinsons misdiagnosis. For many of these patients, the correct diagnosis is a very similar but not as well-known disease: dementia with Lewy bodies . Contact us online or call us at 940-4343 to learn about how we can help your family after a diagnosis.
Dementia with Lewy bodies affects around 1.4 million Americans, as reported by the Lewy Body Dementia Association . That approximation may very well be too low considering that a number of people whove been inaccurately identified as having Parkinsons still have not been given the correct diagnosis.
Both dementia with Lewy bodies and Parkinsons disease dementia are considered Lewy body dementias, but there are differences. The most significant difference is in the one-year rule associated with cognitive symptoms. People with Parkinsons disease typically do not show cognitive issues until at least a year after mobility symptoms begin. DLB is the exact opposite, with cognitive symptoms presenting themselves around a year prior to movement issues.
Hired Hands Homecare, providing elder care in Marin and the surrounding counties, provides the signs and symptoms of DLB that you should be aware of, according to the LBDA:
Knowing That It Is Msa And Not Parkinsons Is Important
Over the years MSA Coalition Board Members have heard the frustration about a slow diagnosis after the initial diagnosis of Parkinsons.While MSA is fatal, knowing the correct diagnosis, is still important.
Multiple system atrophy affects multiple systems in the body.As a result, while there are not MSA specific treatments, treating the various symptoms from sleep disorders, urinary and bowel issues, blood pressure control, etc. can vastly improve quality of life. The earlier an MSA patient is diagnosed, the earlier doctors can establish a plan of action to improve symptoms that can be very disabling. Another factor is that Parkinsons medications typically stop working in MSA patients.
An early diagnosis also allows patients and their families to spend quality time together while they are still able.It also provides time to prepare for end-of-life issues, such as preparing wills and living wills.
Caregiving For People Living With Parkinsons

Caring for a loved one with PD can be a challenging job, especially as the disease progresses. Former caregivers of a loved one with PD suggest doing the following : Get prepared, Take care of yourself, Get help , Work to maintain a good relationship with your loved one, and Encourage the person with PD for whom you care, to stay active.
Preparing for caregiving starts with education. Reading this fact sheet is a good start. More resources are available to you in theResources section of this fact sheet. Early Parkinsonâs disease usually requires more emotional support and less hands-on care. It is a good time for family members/caregivers to educate themselves about the disease.
Quarter Of Parkinson’s Sufferers Were Wrongly Diagnosed Says Charity
Poll of more than 2,000 people found 26% of respondents were told they had something else
More than a quarter of people with Parkinsons disease were initially misdiagnosed, new research has found.
The poll of more than 2,000 people found 26% were first told they had something else, while 21% saw their GP three or more times before being referred to a specialist.
Of those who were misdiagnosed, 48% were given treatment for their nonexistent condition, with 36% receiving medication, 6% undergoing operations or procedures and a further 6% given both medication and operations or procedures.
Of those who received unnecessary treatment, 34% said their health had got worse as a result.
The poll, for the charity Parkinsons UK, also found that women were more likely to be misdiagnosed than men, and errors were most common in people aged 51 to 60.
Katie Goates of Parkinsons UK said: Parkinsons is an incredibly complex condition with more than 40 symptoms, and it affects everyone differently.
One of the biggest challenges for Parkinsons research is that there is no definitive test for Parkinsons, and as a result weve heard of people being misdiagnosed with anything from a frozen shoulder or anxiety to a stroke.
Our survey has shown that because of this, people are being left in limbo and seeing their health deteriorate, which is unacceptable.
About 145,000 people in the UK are diagnosed with Parkinsons every year.
Signs of Parkinsons can include:
What Causes Parkinsons Disease
Parkinsons disease occurs when nerve cells, or neurons, in an area of the brain that controls movement become impaired and/or die. Normally, these neurons produce an important brain chemical known as dopamine. When the neurons die or become impaired, they produce less dopamine, which causes the movement problems of Parkinsons. Scientists still do not know what causes cells that produce dopamine to die.
People with Parkinsons also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinsons, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.
Many brain cells of people with Parkinsons contain Lewy bodies, unusual clumps of the protein alpha-synuclein. Scientists are trying to better understand the normal and abnormal functions of alpha-synuclein and its relationship to genetic mutations that impact Parkinsons disease and Lewy body dementia.
Surgery And Deep Brain Stimulation
Deep brain stimulation is a treatment for Parkinsonâs disease that uses an implantable pacemaker-like device to deliver electrical pulses to parts of the brain involved in movement. The DBS system consists of leads precisely inserted into a specific brain target, the neurostimulator implanted in the chest, and extension wires that connect the leads to the neurostimulator. Though implantation of the system requires a neurosurgical procedure, the treatment itself consists of long-term electrical stimulation. Advantages of DBS include its ability to reduce the high doses of medications , its adjustability , and its reversibility DBS was approved by the Food and Drug Administration as a treatment for PD in 2002 and according to Medtronic , more than 80,000 patients have undergone DBS surgery worldwide.
Typical candidates are those who have motor fluctuations or periods of âoffâ time with troublesome symptoms alternating with periods of âonâ time with good symptom control, and also with possible periods of excessive movement .
Not all patients with Parkinsonâs disease are good candidates for treatment with DBS. Approximately 10â20% of patients considered for possible treatment with DBS include those:
Parkinsons Is Easily Identified By A Pathologist But Is Difficult To Diagnose For A Clinician
When I state that Parkinsons Disease is well defined, I mean that the pathologist, looking at slides of the brain under a microscope, can say, knowing nothing about the patient, that the person had PD. Parkinsons Disease causes certain, easy to detect changes that are seen under the microscope. This, of course, requires that the person is dead, which isnt much use to that particular person or his family. The absence of a reliable test, in life, means then that there is room for mistakes. And, in fact, we make a fair number of mistakes, and Ill discuss below the types of cases in which we are most likely to make mistakes. Unfortunately, we are never in the position of being 100% certain that weve diagnosed someone correctly, until the autopsy.
Misdiagnosis With Dlb Alzheimer’s And Parkinson’s
In life, comedian Robin Williams had been diagnosed with Parkinson’s disease, but an autopsy revealed dementia with Lewy bodies.
Misdiagnosis could lead to patient mismanagement.Getty
Researchers in the United Kingdom and Portugal confirmed that a brain imaging technique can differentiate, with high accuracy, between people with Alzheimers disease, Parkinsons disease, and dementia with Lewy bodies .
The study examined 36 patients using qualitative analysis of in vivo 123IFP-CIT SPECT scans. Of the 36, nine had Alzheimers, ten had Parkinsons, eight had PLD and nine had other diagnoses. Visual analysis of the scans had 88 per cent accuracy in identifying the status of all the individuals and a 96 per cent accuracy when considering only patients with Alzheimers, Parkinsons and DLB.
The study provides some hope for people with any of the three diseases as easier identification could lead to better management and treatment of their conditions.
To be able to quantitatively make these distinctions between diseases is crucial, said Dr. Francisco Oliveira, one of the authors of the study. These diseases may present overlapping symptoms, which makes the clinical diagnosis difficult in some cases and gives rise to a considerable percentage of misdiagnoses. Studies have shown that, frequently, patients with DLB are clinically diagnosed as AD .
It is the second most frequent cause of degenerative dementia in elderly people , the researchers wrote.
Which Test Can Be Done When The Diagnosis Is In Doubt
I request a small set of tests on almost all patients I diagnose with Parkinsons. These detect some mimics of Parkinsons disease.
Some doctors dont request all these tests. And for a good reason.
The diagnosis of Parkinsons mimics is primarily based on a careful history and examination. Even in my practice, these tests change the diagnosis only in a minority of patients.
I like the additional confirmation provided by these tests. They also have other benefits. For example, they help me determine the proper dosages of medications like Amantadine.
| Simple tests to detect Parkinsons Mimics |
|---|
| 1. MRI-Brain with size measurements of brain parts called the midbrain and pons. I usually also request a unique picture called SWI, which shows iron inside the brain.
2. Blood tests: |
But when the diagnosis s really in doubt, there is another brain scan that can be done.
A Trodat scan. Or even better an F-DOPA scan. Both these scans measure dopamine activity inside the brain.
You can read more about Trodat & F-DOPA scans by clicking here.
These scans are not perfect. Let me tell you why very quickly:
In Parkinsons disease, dopamine activity inside the brain is deficient. This deficiency produces an abnormal scan. If the Trodat/F-DOPA scan is normal, it is unlikely that you have Parkinsons disease.
