The Overlaps Between Allergic Reactions And Parkinson’s Disease
Intriguingly, however, the New Scientist article also revealed that other hormone activity in the gut can indirectly influence the production of dopamine in the brain too:
“Stress also leads the gut to increase its production of ghrelin, a hormone that, as well as making you feel more hungry, reduces anxiety and depression. Ghrelin stimulates the release of dopamine in the brain both directly, by triggering neurons involved in pleasure and reward pathways, and indirectly by signals transmitted via the vagus nerve.”
Again, none of my health professionals have ever mentioned ghrelin to me before – I will write a sequel post on what I discovered about this. However, here I would like to underline the point that many people with PD experience “blocking” of their medication after large or hard to digest meals, and now the above helps make sense of this: hunger is a way to stimulate the Vagus Nerve and hence to promote the relaxational “feel good” state of the body, increasing the system’s call on conversion of PD drugs into dopamine in the brain.
“Nevertheless, nerve signals sent from the gut to the brain do appear to affect mood. Indeed, research published in 2006 indicates that stimulation of the vagus nerve can be an effective treatment for chronic depression that has failed to respond to other treatments .“
The New Scientist article links these findings directly to PD – because the gut as well as the brain becomes short of dopamine supplies :
Urinary Difficulties In Parkinsons Disease
The most common urinary difficulty experienced by people with PD is a frequent and urgent need to urinate. Urinary incontinence, the involuntary loss of urine, is also a symptom of PD. This may occur even when the bladder is not full. Recent research studies estimate approximately 27-39% of people with PD experience urinary difficulties, although urinary incontinence only develops in about 15% of those with PD. Bladder issues usually develop in the later stages of PD.2
There are several medications that can help manage urinary difficulties, such as tolterodine, oxybutynin, darifenacin, and solifenacin. These medications work to block or reduce overactivity in the bladder. However, these medications may make the symptoms of PD worse. It is recommended to discuss these treatments with a movement disorders specialist who has been trained to understand the effects of various medications on the disease.2
What You Can Do To Help
- Discuss bladder problems with your family doctor or neurologist, who may perform some tests to rule out urinary tract infection or other problems.
- Speak with your family doctor or neurologist about a referral to a urologist . The urologist will be able to look into any bladder symptoms and provide treatment plans.
- Be aware that bladder difficulties can be a sign of wearing off. Wearing off is where some of the symptoms of Parkinsons occur or worsen between doses of medication and are related to the level of medication becoming too low. Taking your medication on time every time helps reduce fluctuations and that will help reduce bladder difficulties.
- Managing constipation and making sure that you have regular bowel movements will also assist in minimising bladder problems.
Take Control Of Your Parkinsons Treatment
Our Every Victory Counts® manual gives people living with Parkinsons, their care partners and their family members the tools they need to take control of their own Parkinsons treatment through a proactive approach to self-care.
a powerful new print edition
Its jam-packed with up-to-date information about everything Parkinsons, plus an expanded worksheets and resources section to help you put what youve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
Treating And Managing Bowel Problems
The first step in dealing with bowel disorders is to talk to your doctor. He or she will probably review your medication to see if this is a contributory factor. Whilst it is usually possible to control any difficulties with diet, fluid intake and exercise, your doctor, or Parkinsons nurse specialist if you have one, will be able to advise further, and may, for example, prescribe laxatives in severe cases of constipation. If you have any alarm features such as unintentional weight loss or rectal bleeding, then you may need to be referred for specialist assessment.
The following healthcare professionals can also advise on aspects of bowel care:
- A dietician will be able to advise on diet and fluid.
- A physiotherapist may be able to help with advice and abdominal exercises which will help in passing stools.
- A speech and language therapist can help with swallowing problems. They may be able to advise on ways of relaxing your throat, and give guidance on posture and exercises to help overcome any difficulties you have.
- An occupational therapist may also be able to suggest practical ways to overcome any difficulties you have with eating and drinking.
Bowel Issues In Parkinson’s
Recently, I was doing an interview about Parkinsons troublesome issues and I had to admit that by far my most troublesome and annoying problem is related to the effects of my gut. This is true for the majority of us living with this disease. Whether it be a direct or indirect consequence of our illness is irrelevant in my opinion when the effect is the same. Plus to be honest I am not sure anyone of us can tell the difference most of the time.
As I have re-discovered the agony of suffering from one of these ailments over the last several months when I had several bouts of ileus. In my opinion, there is nothing worse than having stomach pain, bloating, nausea, indigestion, and gas to make life miserable.
Below are all the plausible GI symptoms all of us can experience throughout our journey with PD.1 The most common symptoms are those related to poor motility or dysmotility and can be compounded by the effect of the medication.
Treatment For Over Active Bladder In Parkinsons
Overactive bladder affects up to 27% of men and 43% of women of the global population. Now, add a neurological condition and the problem becomes more challenging. First, there is a list of medications which make the problem worse, so should be avoided. Then, a thorough evaluation and physical exam. Treatment depends on the cause, but evaluating all medications and an adjustment of dopamine medication is often necessary. If you are still having problems, five further treatment options are included.
Leaky Blood Brain Barrier And Parkinson’s Disease
which explains how both the blood brain barrier and the gut lining can lose their protective functions in a variety of ways. Given that leaky gut and leaky brain are both heavily implicated in the disease, the road blocks between chemicals produced in the gut reaching the brain is not so assured for people with Parkinson’s. For example, unusually high levels of histamine, which is naturally produced in the gut as part of digestion, have been found in the brains of people with PD
Tips For Caregivers: Reducing Accidents
Incontinence often happens due to timing. It may help to recognize potential signs that a person needs to go, such as straining, turning red in the face, and tugging at their clothing. If you help them get dressed, use clothing thats easy to remove such as pants with elastic waistbands instead of buttons and belts.
One successful technique is prompted voiding. This is a type of bladder retraining that helps people to maintain a regular bathroom schedule. For example, every two hours, ask if theyve had an accident, have the person use the toilet, and praise successes.
A New Toilet Or An Alternative
If you have real difficulties getting to the toilet, it may be possible to get a grant to build a new one, perhaps downstairs. An occupational therapist can advise you on this.
Not all homes are suitable for building new toilets, so a commode might be needed. A commode is a moveable toilet that doesnt use running water. It looks like a chair, with a container underneath that can be removed and cleaned after someone has used it. They can be very discreet.
Urinary Problems In Parkinson’s Disease
Parkinsons disease has many features that have little or nothing to do with movement. Among these non-motor symptoms are problems with the autonomic nervous system the part of the nervous system that controls automatic bodily functions, such as heart rate, blood pressure, sweating, sexual function and both gastrointestinal and urinary function. These symptoms are often among the most serious and complex issues faced by people with PD.
Unlike bowel dysfunction , which often occurs before Parkinsons movement symptoms, urinary dysfunction is not typically a problem until the later stages of the disease.
The Overlaps Between Stress And Parkinson’s Disease Part 2
for detailed articles about the central role of the Vagus Nerve and fight-flight-freeze stress responses in Parkinson’s Disease. Note also the studies which show that, when the Vagus Nerve was surgical severed, this provided a significant protective factor for preventing Parkinson’s Disease – strongly suggesting that the communication of gut problems via the ENS to the autonomic nervous system is linked to PD onset.
“The ENS is capable of carrying reflexes and acting as an integrating center completely independently. The sensory neurons report on mechanical and chemical conditions. Through intestinal muscles, the motor neurons control peristalsis and churning of intestinal contents. Other neurons control the secretion of enzymes.”“The enteric nervous system also makes use of more than 30 neurotransmitters, most of which are identical to the ones found in the brain, such as acetylcholine, dopamine, and serotonin. More than 90% of the body’s serotonin lies in the gut, as well as about 50% of the body’s dopamine.”
Problems Caused By Limited Mobility
Some people with Parkinsons might soil their underwear. This is because mobility problems can make it difficult to wipe after using the toilet. If this is the case, it might help to use wet wipes, a bidet, or an adapted bottom wiper. An occupational therapist or the Disabled Living Foundation can offer further advice.
Bowel problems are common. But you should tell your GP if there are any changes in your bowel habits, particularly if you see blood in your stool. Some problems are difficult to avoid, but there are things you can do to make them less likely to happen.
Gastrointestinal Issues In Advanced Parkinsons Disease
Problems with motility of the gut can be a major source of difficulty throughout the disease course and can be particularly problematic in advanced PD as well. . Constipation, which can be one of the earliest symptoms of PD is a very common problem throughout the disease course. Two gut issues that tend to be particularly problematic in people with advanced PD are abdominal pain and fecal incontinence.
What If I Am Unable To Do A Bowel Program Or It Doesnt Work
A serious injury may keep some people from carrying out a bowel program. For others, the program just may not work. Every person is different. Surgery may be a good option in a few cases, for example:
- If you cant achieve regular, complete bowel movements, which can lead to recurrent severe constipation .
- If you have frequent stool incontinence or lack caregiver support, both of which may contribute to a poor quality of life and confinement in the home.
Other options include two kinds of surgery.
How Can Parkinsons Affect Your Feet
Many people with Parkinsons gradually develop a stooped posture, which affects the feet in 2 ways.
Firstly your body compensates for your weight being held more to the front of your feet, and causes your toes to claw as they grip the ground or your footwear. Over time, your toes get stuck in this position and cannot flatten properly to help you keep your balance.
The second change is in the length of the muscles around your ankle to cope with the shift in your weight. The changes in position mean that some muscles get stretched, while others shorten. Both of these changes alter how efficiently you walk and mean you dont put your heel down first as much as you used to.
The heel striking the ground is the bodys signal to the brain to generate the power to push forward. If youre not doing this it means that your steps will be shorter, youll have less power to propel yourself and it will be harder to balance when standing on 1 leg to step the other forward.
People with Parkinsons can also experience balance problems if their brain isnt receiving the right messages from their body about movement and which areas are bearing weight. This means the brain cant work out how to move the body safely. Without signals from the rest of the body, the brain resorts to judging things visually. For example, looking at the ground while walking, rather than looking straight ahead.
Tips For Caregivers: Management
Medications are available to calm an overactive bladder, if overactive bladder is the cause of the incontinence. But some have side effects that can make dementia worse. Talk with the doctor about options that apply to the person youre caring for. In some cases, where incontinence is caused by an underlying medical condition, treating the condition may help.
Could You Be Malnourished If You Have Parkinsons
While Dr Bloem pointed out that a regular diet shouldoffer all the necessary nutrients, he did note that vitamin D and vitamin C canbe exceptions. Many people, particularly when you age and particularly whenyoure a woman, are at risk of developing a vitamin D deficiency. There arefascinating anecdotal reports of people taking vitamin D and experiencingimproved motor symptoms.
Meanwhile, he explained, vitamin C supplements can help toprevent bladder infections in Parkinsons patients by acidifying the urine. Bladderinfections can trigger a cascade that leads to worsening Parkinsons symptoms.
Dr Bloem also debunked the use of supplements like vitamin E, curcumin and Coenzyme Q190, which have been found to offer no benefits to people with Parkinsons.
Gmb: Sharon Osbourne On Ozzy Suffering From Parkinsons
We use your sign-up to provide content in ways you’ve consented to and to improve our understanding of you. This may include adverts from us and 3rd parties based on our understanding. You can unsubscribe at any time. More info
Parkinsons disease is a harsh reality for many families. Yet, early diagnosis can make living with the condition much more manageable. What’s the change in bowel habits that may signal the brain disease?
According to Parkinson’s Foundation, the disease affects dopamine-producing neurons in a part of the brain called substantia nigra.
Symptoms develop slowly over years, with the condition affecting people in different ways.
An early warning sign of Parkinson’s is experiencing difficulty with passing stools.
Fecal Incontinence In Advanced Parkinsons Disease
Fecal incontinence is a very debilitating symptom that can occur in advanced PD and refers to the involuntary release of fecal matter.
Once again, fecal incontinence, especially if it is a new symptom, should be fully evaluated to determine if there is a cause unrelated to PD. Diseases of the gut such as inflammatory bowel disease or compression of the lower spine cord can be the reason.
If related to PD, there are typically two situations to consider. One possibility is that severe constipation with impacted bowel movement allows loose stool from higher up in the gastrointestinal tract to escape around the edges of the obstruction. In this situation, fecal incontinence could be a harbinger of bowel obstruction. Aggressive and continuous treatment of constipation can help avoid this potential scenario.
Fecal incontinence can also be related to nerve dysfunction of the anal sphincter, or the ring of muscle that controls when feces is released. Cognitive dysfunction and mobility issues may further interfere with getting to the bathroom in time. Some treatment options are similar to urinary incontinence including the use of bedside equipment to minimize mobility issues and introduction of pelvic floor exercises to strengthen the musculature that keeps feces in place.
As with urinary incontinence, frequent and rapid exchange of dirtied incontinence products can keep skin intact and prevent infection.
Tips and Takeaways
Dr. Rebecca Gilbert
Addressing Practical Aspects Of Eating And Drinking
Some people with Parkinsons have problems chewing and swallowing. This can make it difficult to eat a diet with plenty of fibre. A speech and language therapist can give advice about this. Ask your GP, specialist or Parkinsons nurse for a referral. If it takes a long time to eat and your meal goes cold, eat smaller portions and go back for seconds that have been kept warm. You can also get special plates that keep your meals hot the Disabled Living Foundation has more information.
An occupational therapist will also be able to give you some tips and practical advice.
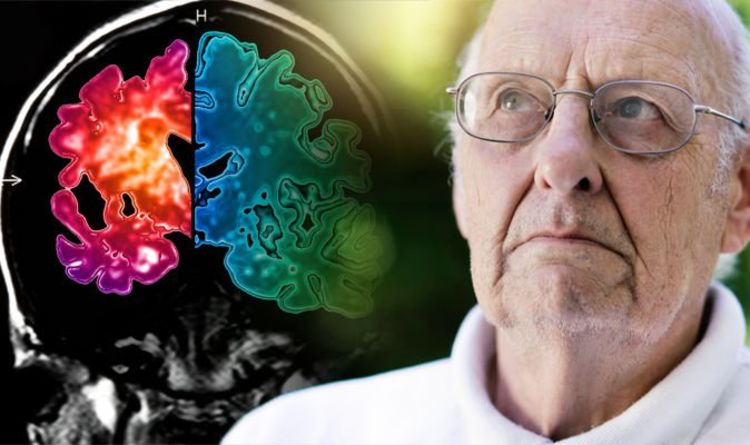
Parkinsons Disease Is A Neurodegenerative Condition
Parkinsons disease is a chronic condition in which neurons within a region of the brain responsible for the control of movement break down and die. These neuronal cells use a chemical called dopamine to communicate with each other. It is this complex dopamine-based communication between neurons that is responsible for control of movement. Death of these neurons is referred to as dopaminergic neurodegeneration, and directly leads to the movement-related symptoms of the condition . These include tremors, changes in posture, stiffness, and a slowness of movement, also referred to as bradykinesia.1,2
Importantly, and often little appreciated, is the fact that Parkinsons disease can also affect neurons outside of the brain. Neuronal connections are made throughout the body, and connect all parts of the body to the brain and spinal cord, including to the GI tract. In particular, Parkinsons interferes with normal communication between the central nervous system, and the esophagus and stomach.3 Parkinsons can also affect the enteric nervous system, a network of neurons that functions with a considerable level of independence from the brain and central nervous system, and that is highly involved in controlling the intestinal tract and digestion.3,4 By affecting both the central and enteric nervous systems, Parkinsons disease may give rise to an array of GI symptoms.
Evaluating And Treating Urinary Issues In Parkinson’s Disease Multiple System Atrophy And The Other Atypical Parkinsonism Disorders
In this hour-long webinar, neuro-urologist Ekene Enemchukwu, MD focuses on urinary incontinence, overactive bladder, urinary retention, and other urinary issues in PD, MSA, and the atypical parkinsonism disorders. Following the presentation, moderator Candy Welch, Brain Support Networks MSA caregiver support group leader, asks Dr. Enemchukwu many questions submitted by webinar participants.
Bladder And Constipation Problems
Parkinsons commonly leads to problems with constipation and bladder control, including urinary urgency, frequency, retention and nocturia.
These problems add to the challenge of living with Parkinsons and can have a negative effect on a persons quality of life. It is important to seek help in managing these problems, as both issues can be effectively managed.
The Gastrointestinal Tract And Parkinsons
As promised in a previous blog, I now return to the topic of the gastrointestinal tract and Parkinsons disease . As most of you know, GI symptoms are very common in PD. We will discuss what those symptoms are, why they occur, and the current research that links what is happening in the gut to theories as to why PD occurs at all. Many of you have suggested gut-related topics for this blog including a discussion of symptoms such as bloating and constipation, and a discussion of the use of probiotics in PD. I will address these issues as well. Submit additional topics that you would like to read about here.
GI symptoms can be among the most bothersome of the non-motor symptoms of PD. Constipation is the most common of these symptoms, affecting 80-90% of people with PD. APDA has a helpful brochure with practical tips to prevent and treat constipation in PD.
GI pathology in Parkinsons disease however, can involve the entire GI tract and includes sialorrhea and dysphagia . In addition, delayed gastric emptying, in which the digestive contents are held up in the stomach and do not move normally into the small intestine, can cause sensations of nausea and bloating.
The gut has its own nervous system
The gut as a biomarker
Entry to the brain
How do Lewy bodies propagate?
Medication Side Effects And The Gut
The interactions between PD medication ingestion and the gut can play a major role in motor fluctuations the phenomenon in which a patients response to Levodopa varies widely during the day. A recent APDA webinar helps to explain this interplay.
Delayed gastric emptying
Delayed gastric emptying can interfere with medication absorption. Medication doses that are ingested by mouth may sit in the stomach before being transported to the small intestine where they are absorbed. Delayed gastric emptying could be responsible for dose failures when a dose of medication does not have a robust enough effect.
Protein effect
Levodopa crosses the wall of the small intestine via a molecule in the intestinal wall that transports amino acids, the building blocks of protein. When dietary protein is also present in the small intestine, then there are fewer transporters available for Levodopa to use. A patient may therefore experience the protein effect, in which he or she feels that medication is not as effective after a high-protein meal. Sources of dietary protein include: beef, chicken, pork, fish, eggs, nuts and dairy.
Helicobacter pylori and small intestinal bacterial overgrowth
About a third of PD patients are infected with Helicobacter pylori, a common bacteria which can cause gastritis and ulcers. Infection with Helicobacter pylori has been linked to worsened motor fluctuations. It can be diagnosed with a urea breath test that analyzes exhaled air.
Study Reveals Ibs Risk
BERLIN — Irritable bowel syndrome may be a more frequent symptom in Parkinson’s disease than constipation, researchers reported here.
In a case-control study, about a quarter of Parkinson’s patients had IBS compared with only 5% of healthy controls , according to Tuomas Mertsalmi, MD, of the University of Helsinki, and colleagues.
On the other hand, the prevalence of constipation was higher among Parkinson’s patients, but the difference from healthy controls wasn’t significant, they reported at the Movement Disorders Society meeting here.
“Gastrointestinal symptoms in Parkinson’s disease are more complex than just constipation,” Mertsalmi told MedPage Today. “Usually constipation is just seen as decrease bowel frequency, but it is also about straining during defecation, hard and lumpy stools, and diarrhea in these patients.”
Previous work has shown that the majority of patients with Parkinson’s suffer from gastrointestinal symptoms. About 70% have been estimated to have constipation, which is considered to be a premotor symptom of the disease and is one of the strongest risk factors for Parkinson’s, Mertsalmi said.
IBS is among the most common functional gastrointestinal disorders, and is characterized by symptoms of abdominal pain or discomfort, and alteration of bowel habits.
All patient with a pre-existing diagnosis of IBS were excluded, he added.
The two most common subtypes in Parkinson’s patients were mixed IBS and constipation-predominant , they reported.
Urinary Issues In Advanced Parkinsons Disease
Urinary dysfunction and symptoms in PD are most commonly caused by overactivity of the detrusor muscle, or the muscle of the bladder, which contracts excessively despite the fact that it is not filled with urine. This causes an increased urge to urinate and/or an increased frequency of urination, which can be especially prominent at night. In advanced PD, this could culminate in urinary incontinence, or involuntary release of urine. Mobility issues which make getting to the bathroom slower and more cumbersome, compound the problem.
Always remember that people with advanced PD may have other medical problems that affect their urination such as an enlarged prostate. Make sure to have a complete evaluation before assuming that the problem is only related to PD. It is also essential to keep in mind that if changes in urination occur suddenly, there could be a urinary tract infection present.
Once other medical issues and urinary tract infection are ruled out, there are a number of approaches to the issue of urinary incontinence in a person with advanced PD:
Unfortunately, for some, the above available options may not be sufficient to effectively treat urinary incontinence in advanced PD. If this is the reality, it becomes extremely important to keep the skin dry with frequent changes of incontinence products to prevent skin breakdown and the potential development of skin infection.
