People Who Already Have Pd: Should I Get Tested And What Do I Do With The Results
Up until recently, even people with PD with a very extensive family history of PD would not necessarily receive genetic testing because there were no clear uses for the results. There has been research directed at figuring out whether PD caused by or associated with certain mutations have particular clinical characteristics . However, there remains so much variability in clinical characteristics even among people with the same PD mutation, that there are still no clear practical implications in knowing whether a PD patient harbors a particular mutation. There is also, so far, no difference in treatment or management of PD whether or not the patient harbors one of the known mutations. That may change however, with the advent of clinical trials that target particular mutations.
There are two genes that have received particular attention recently because medications are being developed that target those with mutations of these genes.
GBAis a gene that increases the risk of developing PD. The gene encodes for the GBA enzyme, a protein used by the body to break down cellular products. Having two abnormal GBA genes causes Gauchers disease, which is characterized by the buildup of these cellular products resulting in fatigue, bone pain, easy bleeding and an enlarged spleen and liver. When a person inherits only one abnormal gene, he or she does not develop Gauchers disease, but does incur a small increased risk of PD. Most people with one mutated GBA gene do not develop PD.
Looking For Signs Of Parkinsons
Your specialist will examine you to look for common signs of Parkinsons. You may be asked to:
- write or draw to see if your writing is small or gradually fades
- walk to see whether theres a reduction in the natural swing of your arm or in your stride length and speed
- speak to see if your voice is soft or lacks volume
The specialist will also look at and ask you about your:
- face to see if there is a masked look or if you have difficulty with facial expressions
- limbs to see if you have a tremor, any stiffness or slowness of movement
As well as examining you for any of the typical signs of Parkinsons, the specialist will also look for signs that may suggest a different diagnosis.
It may be helpful to take someone with you for support when seeing a specialist. Taking a list of questions you want to ask can also be useful so you dont forget to mention something you want to know about. If a healthcare professional says something you dont understand, dont be afraid to ask them to explain what they mean.
Metabolomics And Other Omics For Pd Diagnostics
In addition to gene analysis, approaches related to the study of the transcriptome of PD patients attract much attention . In particular, minimally invasive approaches that are not associated with CSF selection are of great interest. Wang and co-authors proposed a method for determining individual handwriting combinations in the blood cells, whose expression significantly changes in PD patients . In the work of Karlsson and co-authors a biochip was proposed for analyzing the expression of 650 informative genes in the blood of PD patients at different stages of the disease with a sensitivity of 8488%, which is close to the results of clinical diagnostics . A set of several differently expressed microRNAs in CSF can classify PD and MSA patients from controls with good diagnostic accuracy by evaluating the receiver operating characteristic . An important diagnostic value is the analysis of the content of that micro-RNAs. The article by C. Starhof and co-authors shows that the analysis of Mir-7-5p, miR-331-5p, and miR-145-5p microRNAs in CFS made it possible to diagnose PD with sensitivity of 88% . Another study of 35 untreated and 12 treated patients with the sporadic form of PD proposed a method for analyzing the expression of micro-RNA levels of ATP13A2, PARK7, and ZNF746 in the peripheral blood, which can be suggested also as potential biomarkers of the preclinical stage of PD .
How Is Parkinson’s Diagnosed
Current evidence suggests that tends to develop gradually. It may be many months, even years, before the become obvious enough for someone to go to the doctor.
This information looks at what is, how Parkinsons and other similar conditions may be diagnosed, and explains some of the tests that may be involved in the process.
Parkinsonism is a term used to describe symptoms or signs that are found in Parkinsons, but which can also be found in other conditions that cause slowness of movement, and .
Most people with a form of parkinsonism have idiopathic Parkinsons disease, also known as Parkinsons. Idiopathic means the cause is unknown.
Other less common forms of parkinsonism include multiple system atrophy , progressive supranuclear palsy , drug-induced parkinsonism and vascular Parkinsons.
If youre concerned about symptoms youve been experiencing, you should visit your GP. If your GP suspects you have Parkinsons, clinical guidelines recommend they should refer you quickly to a specialist with experience in diagnosing the condition .
Its not always easy to diagnose the condition. So its important that you see a Parkinsons specialist to get an accurate diagnosis and to consider the best treatment options.
Diagnosing Parkinsons can take some time as there are other conditions, such as essential tremor , with similar symptoms. There is also currently no definitive test for diagnosing Parkinsons.
How Parkinsons Disease Is Diagnosed

editorial processMedical Review Board
Diagnosing Parkinsons disease can be complicated because there isnt a specific blood test or screening test that can determine whether or not you have it.
Instead, Parkinsons is diagnosed clinically, which means a doctor will examine you, review your symptoms and medical history, and diagnose accordingly.
Parkinsons disease is a neurological condition that can make movement difficult. If your general practitioner thinks you might have Parkinsons, they may refer you to a neurologist who specializes in movement disorders for a diagnosis.
It can be challenging to catch Parkinsons in the early stages because the symptoms may be too mild to notice or meet the diagnostic criteria. Also, early Parkinsons symptoms are often mistaken for typical signs of .
The symptoms of Parkinsons disease are also similar to those of other health conditions, which may be misdiagnosed as Parkinsons at first. Your doctor may suggest specific tests and scans to help eliminate other conditions that can mimic the symptoms of Parkinsons disease.
Obtaining A Parkinson’s Disease Diagnosis
During the exam, the neurologist will look for cardinal symptoms of the disease. Facial expressions and features will be assessed. The doctor will look for signs of while the patient is at rest. The doctor may watch how easily the patient stands up from sitting in a chair. The doctor may also stand behind the patient and gently pull back on the patients shoulders and look for how easily the patient can regain balance. Good responsiveness to also helps support the diagnosis of PD. However, taking levodopa may exclude patients from clinical studies that need to recruit recently diagnosed patients who have not yet had treatment . Participation in a clinical trial should be discussed with the doctor.
PD can be challenging to accurately diagnose, particularly in early stages of the disease, which is why a neurologist trained in movement disorders is critical. Approximately 5-10% of patients with PD are misdiagnosed, as many of the of PD are similar to other diseases. If the patient thinks that he or she has been misdiagnosed, a second opinion may help.1,2
Breakthrough Skin Test Detects Early Signs Of Parkinsons Disease With Amazing Accuracy
AMES, Iowa For patients dealing with Parkinsons disease, a tremor in their hands may be the first symptom they notice. While this is a common sign, its not always a reliable gauge of an otherwise difficult disease to diagnose in its early stages. A team at Iowa State University say theyve made a breakthrough in Parkinsons research which may lead to an extremely accurate way of spotting the condition. Their study reveals a simple skin test can identify changes in the body caused by the disease.
Parkinsons is a progressive neurological disorder which impairs movement, causes stiffness and a loss of balance. The symptoms commonly include tremors in the hands and slurred speech that worsens over time. Currently, there is no cure for the disease.
Prof. Anumantha Kanthasamy says Parkinsons is particularly hard to diagnose and doctors often misdiagnose it early on. Even worse, the disease is only definitively diagnosed through an autopsy following the patients death.
The study finds the new skin examination detects clumping in alpha-synuclein proteins. Misfolded alpha-synuclein proteins accumulating in the brain are a telltale sign of Parkinsons. These buildups lead to neuronal damage, bringing on the impaired motor functions in patients. While these clumps center in the brain, study authors say theyre also detectable in skin and tissue samples.
Obtaining A Parkinsons Disease Diagnosis
During the exam, the neurologist will look for cardinal symptoms of the disease. Facial expressions and features will be assessed. The doctor will look for signs of while the patient is at rest. The doctor may watch how easily the patient stands up from sitting in a chair. The doctor may also stand behind the patient and gently pull back on the patients shoulders and look for how easily the patient can regain balance. Good responsiveness to also helps support the diagnosis of PD. However, taking levodopa may exclude patients from clinical studies that need to recruit recently diagnosed patients who have not yet had treatment . Participation in a clinical trial should be discussed with the doctor.
PD can be challenging to accurately diagnose, particularly in early stages of the disease, which is why a neurologist trained in movement disorders is critical. Approximately 5-10% of patients with PD are misdiagnosed, as many of the of PD are similar to other diseases. If the patient thinks that he or she has been misdiagnosed, a second opinion may help.1,2
Physical Examination And Tests
A trip to the neurologists office often includes what seems like dozens of questions, along with multiple tests.
There currently are no diagnostic blood tests for Parkinsons disease, but your doctor may do some routine blood and urine tests to assess your overall health. Your blood pressure will be taken sitting and standing to look for orthostatic hypotension.
A movement disorder specialist will do a variety of physical tests to assess you as well.
Network Analysis And Cognition
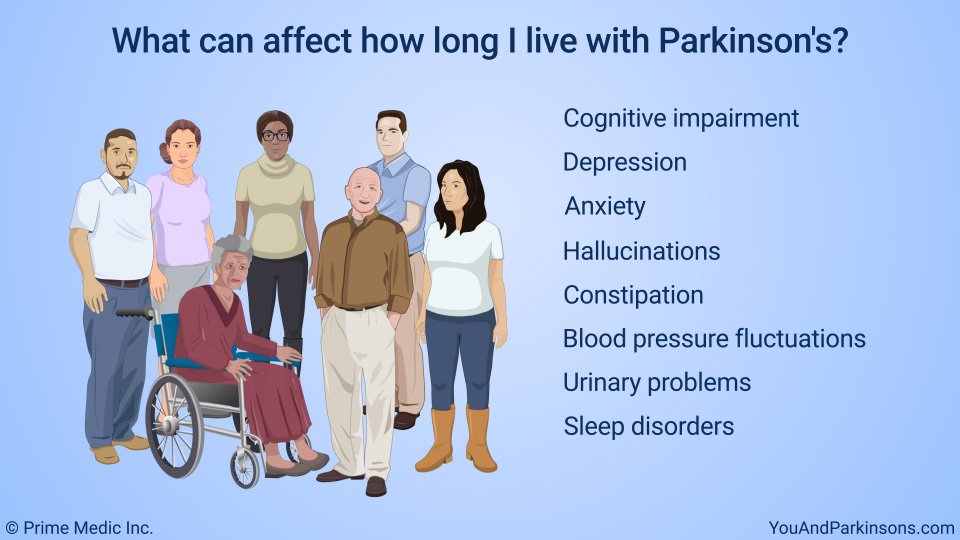
While the clinical diagnosis of PD rests largely on the motor signs and symptoms , non-motor symptoms can be prominent and even precede the motor symptoms . For example, RBD, as discussed earlier, represents a strong risk factor for PD . Cognitive dysfunction can be substantial in PD, typically appearing later in the disease and progressing slower. Nevertheless, the point prevalence of PD is high , and with time the majority of patients will develop cognitive impairment or dementia .
Neurology87Cold Spring Harbor Perspectives in Medicine2Neurology87Neuroimage78
The partial relation between PDCP expression and dopaminergic dysfunction may help explain why non-demented PD patients can have different changes in cognition when receiving dopaminergic treatments. Specifically, improvement in verbal learning that some patients exhibit with levodopa treatment, depends on baseline PDCP expression . PD patients with caudate tracer uptake in the 3550% range exhibit modest PDCP elevations and show improved cognitive response with medications. In contrast, those with a relatively intact caudate dopaminergic system exhibit cognitive decline with levodopa, which is in accordance with a dopamine overdose hypothesis . Similarly, patients with advance dopaminergic dysfunction and high PDCP scores lose the cognitive benefit from levodopa, possibly due to advance pathology in key PDPC nodes .
How Is Parkinsons Disease Managed
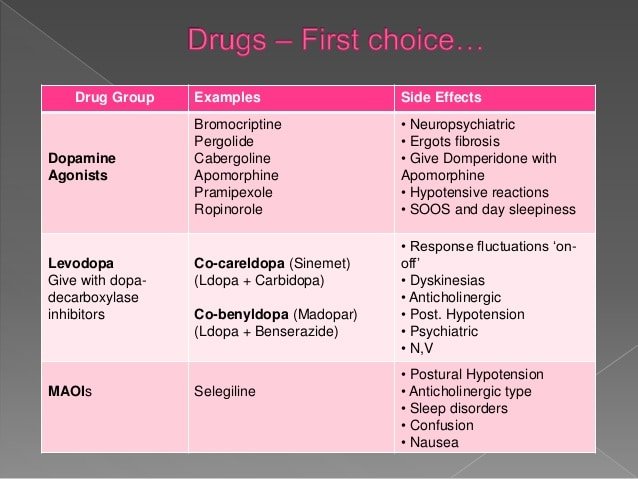
Your doctors will tailor your treatment based on your individual circumstances. You will manage your condition best if you have the support of a team, which may include a general practitioner, neurologist, physiotherapist, occupational therapist, psychologist, specialist nurse and dietitian.
While there is no cure for Parkinsons disease, symptoms can be treated with a combination of the following.
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms noticed by the patient or his or her loved ones are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctors office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinsons disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
What Tests Diagnose Parkinson’s Disease
editorial processMedical Review Board
There currently are no tests that can definitively diagnose Parkinsons Disease. A diagnosis is based on the clinical findings of your physician in combination with your report on the you are experiencing.
In situations where an older person presents with the typical features of Parkinsons and they are responsive to dopamine replacement therapy, there is unlikely to be any benefit to further investigation or imaging.
What Are The Symptoms Of Parkinsons Disease
The main symptoms of Parkinsons disease are:
- tremor or shaking, often when resting or tired. It usually begins in one arm or hand
- muscle rigidity or stiffness, which can limit movement and may be painful
- slowing of movement, which may lead to periods of freezing and small shuffling steps
- stooped posture and balance problems
The symptoms of Parkinsons disease vary from person to person as well as over time. Some people also experience:
- loss of unconscious movements, such as blinking and smiling
- difficulties with handwriting
- drop in blood pressure leading to dizziness
- difficulty swallowing
- sweating
Many of the symptoms of Parkinsons disease could be caused by other conditions. For example, stooped posture could be caused by . But if you are worried by your symptoms, it is a good idea to see your doctor.
Diagnosis Of Parkinson Disease: Motor Symptoms
The clinical diagnosis of Parkinson’s disease is based on the presence of characteristic motor symptoms: bradykinesia, rigidity, postural instability, and resting tremor but neuropathology is still considered the gold standard for definite diagnosis. Differentiating PD from other movement disorders can be challenging throughout the disease course, because signs and symptoms often overlap. Indeed, neuropathology studies reveal that clinical diagnosis of PD can be confirmed with an accuracy of about 75%. Good response to levodopa is often used to support the diagnosis of PD. However, cases of pathologically proven PD with poor response to levodopa have also been reported.
Misdiagnosis of PD can occur for several reasons. In a community-based study of patients taking antiparkinsonian medication, the most common misdiagnosis were essential tremor, Alzheimer’s disease, and vascular parkinsonism. In addition, many of the prominent features of PD may also occur as a result of normal aging or from comorbid and multifactorial medical conditions .
R. Savica, … G. Logroscino, in, 2016
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinsons disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the persons symptoms strongly suggest to the physician that idiopathic Parkinsons disease is the correct diagnosis.
Helping diagnose Parkinsons with DaTscan and other tests
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinsons. Imaging studies to evaluate Parkinsons disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinsons disease from certain other neurologic disorders. Most physicians offices will have access to MRI; however, DaTscan imaging may only be available at larger hospitals or medical centers.
New Diagnostic Standards For Parkinsons
Until recently, the gold-standard checklist for diagnosis came from the U.K.s Parkinsons Disease Society Brain Bank. It was a checklist that doctors followed to determine if the symptoms they saw fit the disease. But thats now considered outdated. Recently, new criteria from the International Parkinson and Movement Disorder Society have come into use. This list reflects the most current understanding of the condition. It allows doctors to reach a more accurate diagnosis so patients can begin treatment at earlier stages.
Early Signs Of Parkinson’s
Early physical signs include the common motor symptoms: tremor, muscle rigidity and slowness. They may also include the following:
- Symptoms starting on one side of the body
- Change in facial expression
- Failure to swing one arm when walking
- Stooped posture
- Loss of sense of smell
- Depression or anxiety
Some of these symptoms are quite common and by no means exclusive to Parkinsons, so if you have some of them, it does not mean you have Parkinsons.
How It All Fits Together
Diagnosing Parkinsons disease can be tricky. The process relies heavily on your doctors judgment. In addition, the causes and risk factors of Parkinsons are not entirely clear yet, which contributes to the difficulty in diagnosing this condition.
However, there have been efforts to try and detect this disease earlier. For instance, clinicians have started focusing more on prodromal symptoms, which are early symptoms that appear before movement-related difficulties begin.
These symptoms include:
- Loss of smell, which can sometimes occur years before other symptoms
- Chronic constipation, without any other explanation
Who Do I Contact For A Diagnosis Of Parkinson’s Disease
If you are worried, see your GP. He will be able to support you and refer you to appropriate specialists.
The diagnosis of Parkinsons disease is based on your doctors description of symptoms and his neurological examination. There is no blood test or x-ray examination to confirm the diagnosis.
The first symptoms of the disease are not specific. Taken one by one, they do not make it possible to rule on the disease. However, it is the general portrait of the symptoms that will concern your doctor.
If your doctor suspects that you have Parkinsons disease, they will put you on a waiting list to get an appointment with a neurologist. Depending on the availability of resources in your area, you should get an appointment within 6 months. If you have had a fall in the past few weeks, tell the doctor. This could reduce your wait time.
Keep a symptom diary and bring it to your appointment. This will help you describe the changes you have observed.
- What are your concerns?
- What medications do you take?
- What changes have you observed?
- Are there any situations that make your symptoms worse?
- Are your daily activities affected? Which ones?
- Do you have difficulty smelling certain smells?
- Do you have trouble sleeping?
- Have you noticed any changes in your memory or mood?
Have someone accompany you to your appointment. Not only will your loved one be able to provide important information during the meeting, but will also be able to support you in the process of accepting the diagnosis.
Gauging Speed Of Movement
Bradykinesia occurs in most people who have Parkinsons.?? It may cause a lack of spontaneous facial expression and fewer eye blinks per minute than usual, and your doctor will look for these signs in your physical exam.
Your doctor also may assess your speed of movement by asking you to open and close each hand or tap your index finger against your thumb repeatedly, making large movements as quickly as possible. In people with Parkinsons disease, the movement may start off fast and precise, but it will deteriorate quickly, becoming slow and limited.
Gait is also another way to test for this. Observing a patient while they walk, noting the length of their stride as well as the speed at which they move, can tell doctors quite a bit. Lack of arm swing is also a feature that appears fairly early in those with Parkinsons.
Bradykinesia in Parkinsons Disease
Response To Parkinsons Drugs
After examining you, and depending on the severity of your symptoms, your specialist may suggest you take medication for Parkinsons. If your symptoms improve after taking Parkinsons medication for a few weeks or months, your specialist may confirm a Parkinsons diagnosis. However, some people with other forms of parkinsonism will also respond well to these drugs.
Your specialist may suggest you have a scan to help make a diagnosis. However, scans alone cant make a definite diagnosis of Parkinsons, so they are not commonly used.
Who Are The Specialists In The Treatment Of Parkinson’s Disease In Quebec
The doctors who treat Parkinsons disease are neurologists. Some of them are specialized and work in clinics for movement disorders.
In these clinics, interdisciplinary teams made up of health professionals, such as physiotherapists, speech therapists, specialist nurses, can help you manage the symptoms of the disease as they appear.
How Is Parkinsons Disease Tested And Diagnosed
At Banner Health, our neurologists have years of experience in testing and diagnosing Parkinsons disease. Our team of compassionate experts knows that each patient is different, so we work with you to quickly find the right diagnosis to begin building your treatment plan.
Parkinsons is not simple to diagnose. No test exists to diagnose Parkinsons disease. Doctors test and diagnose Parkinsons based on your medical history, symptoms and neurological and physical exams.
Many times a primary care provider is the first to suspect a Parkinsons diagnosis. If youre experiencing symptoms such as tremors, shaking, slow movement, stiffness and/or trouble with balance, talk to your doctor or seek the opinion of a neurologist. Banner Health neurologists are movement disorder specialists, who have experience and specific training to assess and treat Parkinsons.
What Research Has Been Done And The Need To Improve:
CANTAB Connect for Parkinsons disease is a rapid, reliable, and highly sensitive system for academic research or clinical trials. The CANTAB battery has demonstrated potential advantages when compared to other neuropsychological tests, such as for detecting cognitive impairment in Parkinsons disease7 and also avoiding floor and ceiling effects. It is highly sensitive to disease progression, can discriminate cognitive impairment due to comorbid depression, and detects untoward effects of medications on cognition11-14. It has also been shown to predict conversion to dementia in patients with Parkinsons disease15. The use of CANTAB in research of Parkinsons disease is clinically relevant: cognitive decline measured by the battery correlates with loss of day-to-day functioning in patients with Parkinsons disease16.
Furthermore, CANTAB maximises scope for sample enrichment, and for demonstrating disease modifying capability of interventions.
There are currently over 125 peer-reviewed publications supporting the application of CANTAB in research of Parkinsons disease. To find out more, .
Diagnosing Parkinson’s Disease With Skin Samples Could Lead To Earlier Detection
- Date:
- Iowa State University
- Summary:
- New research shows a simple skin test can accurately identify Parkinson’s disease, which could lead to earlier detection of the disease and better outcomes for patients. Currently, Parkinson’s disease is diagnosed by clinical signs and symptoms but only definitively diagnosed at autopsy. The researchers conducted a blinded study of 50 skin samples using an assay originally designed to detect mad cow disease.
New research shows a simple skin test can accurately identify Parkinson’s disease, demonstrating for the first time the feasibility of the method. Currently diagnosed by clinical signs and symptoms but only definitively diagnosed at autopsy, Parkinson’s disease is commonly misdiagnosed early in the disease course, complicating clinical trials of potential treatments.
The study, published in the scientific journal Movement Disorders, shows how a chemical assay can detect clumping of the protein alpha-synuclein in skin samples to help diagnose Parkinson’s disease . The study’s authors said using the assay can lead to earlier detection of PD and better clinical trials.
“Since there’s no easy and reliable test available for the early diagnosis of Parkinson’s disease at present, we think there will be a lot interest in the potential use of skin samples for diagnosis,” said Anumantha Kanthasamy, Distinguished Professor of Biomedical Sciences at Iowa State and lead author of the study.
Story Source:
