How Is Sleep Apnea Treated
A continuous positive airway pressure machine, a machine that blows air into your airway at a pressure that is sufficient to keep the airway open during sleep, is the most consistently effective treatment for obstructive sleep apnea. The CPAP machine is connected by a tube to a face mask worn when sleeping through the night. It controls pressure in ones throat to prevent the walls of the throat from collapsing, creating better sleep quality. CPAP should be worn for the entire night and for naps.
Parkinsons Symptoms Including Pain And Frequent Urination
Pain is a common cause of sleep disturbances in Parkinsons, says Horvat. A study published in June 2019 in the Journal of Pain Research found that about one-third of people with Parkinsons had clinically relevant sleep disturbances, and that central parkinsonian pain was the pain subtype that was most often associated with sleep issues.
Central pain can vary widely from person to person. It can feel like a constant burning or tingling that affects the whole body or it can be an intermittent sharp episode of pain, according to the Parkinsons Foundation.
You should definitely talk to your doctor if pain or Parkinsons symptoms are waking you up or keeping you up at night, to see what your treatment options may be, says Horvat.
Frequent urination can be a sign of several different things, and so its important to pay attention to any other symptoms you may also be having, she says.
Autonomic instability is often present in Parkinsons disease, which basically means the autonomic system is not firing regularly, as it should be, says Horvat. The autonomic system controls functions that keep you alive, including your heartbeat, breathing, and digestion.
This condition can lead to incontinence or urinary retention, she says. This is something to talk with your doctor about there are some medications that can be helpful.
Cognition And Obstructive Sleep Apnoea In Parkinsons Disease Effect Of Positive Airway Pressure Therapy : Protocol Of A Randomized Controlled Trial
Annie C. Lajoie, Annie-Louise Lafontaine, Gabriel Leonard, R. John Kimoff, Andrea Benedetti, Ann R. Robinson, Joelle Crane, Marie Létourneau, Marta Kaminska
Abstract
Background: Parkinsons disease is the second most frequent neurodegenerative disease and is associated with cognitive dysfunction. Obstructive sleep apnea has been linked with cognitive dysfunction in the general population and in PD. Treatment with positive airway pressure , can improve cognition in the general population and in patients with other neurodegenerative diseases. However, the effect of PAP therapy on cognitive function has not been well studied in PD.
Methods: This randomized controlled trial will assess the effect of 6 months of PAP therapy versus placebo on global cognitive function in PD patients with OSA and reduced baseline cognition. Secondary outcomes will include quality of life and other non-motor symptoms of PD. Exploratory outcomes will be specific domains of neurocognitive function and symptoms of REM sleep behaviour disorder.
PD-related cognitive dysfunction often evolves towards dementia and has substantial personal, social and healthcare costs. Few interventions have been shown to improve cognition in PD to date. If positive, results from our study could prove OSA to be a new therapeutic target relevant to cognition and would support more systematic screening for OSA in PD patients with cognitive decline.
Trial Registration: Trial registration number is NCT02209363.
Keywords
Don’t Miss: How Long Does It Take For Parkinson’s To Progress
Rem Sleep Behavior Disorder
REM sleep behavior disorder is common in people with Parkinsons disease, says Horvat. REM stands for rapid eye movement, and REM sleep is a stage of sleep associated with dreaming.
People with RBD can have very vivid dreams in which they are defending themselves or a loved one from being attacked or are being chased by animals, insects, or people, said Joohi Jimenez-Shahed, MD, a neurologist at Mount Sinai Health System in New York City, in a caregiver presentation sponsored by the Houston Area Parkinson Society.
During these episodes, people with RBD will start acting out their dreams, usually in the last half of the night, says Horvat. Shouting, swearing, grabbing, punching, jumping, and kicking while asleep are all symptoms of RBD.
Ill have patients tell me, I was fighting someone in my dream, I woke up punching, and I hit my significant other who was in bed next to me, she says. This can be very dangerous for both the person with PD and their partner, says Horvat. It can cause someone to fall out of bed Ive had patients suffer brain bleeds because of this.
There are treatments that can help, such as melatonin or benzodiazepines , she says. We also look for other sleep disorders because they can make RBD worse: I actually have a patient where we resolved these episodes by treating their sleep apnea, says Horvat. If youre experiencing these types of dreams, you need to discuss this with your doctor, she adds.
Demographic Characteristics Of The Surgery Conservative And Control Groups

In a comparison of the three groups, the surgery group had the highest male percentage and the lowest average age . The lower quintile ratio of income was highest in the control group and lowest in the surgery group . The prevalence of comorbidities was higher in the conservative group than in the control group. The surgery group had a lower prevalence of comorbidities than the conservative group, but the prevalence was generally higher than in the control group. The demographic data is summarised in Table .
Table 2 Demographic characteristics of patients with OSA and controls.
Read Also: How To Prevent Parkinson Disease Naturally
Rem Sleep Behavioral Disorder
Rapid eye movement, or REM, sleep is the part of the sleep cycle when dreaming occurs. Usually the only part of the body that moves during REM sleep is the eyes.
- People with rapid eye movement sleep behavior disorder do not have the normal relaxation of the muscles during their dreams. Therefore, they act out their dreams during REM sleep.
- People with RBD may shout, hit or kick their bed partner or grind their teeth. Sometimes, in moderate to severe RBD, people may have aggressive, violent behaviors, like getting out of bed and attacking their bed partner.
- About half of people with PD suffer from RBD. It may develop after or along with the motor symptoms, but in most cases, it precedes the PD diagnosis by five to 10 years.
Cognitive Performance In Rapid Eye Movement Sleep Behavior Disorder And Epworth Sleepiness Scale Subgroups
Cognitive measures in patients with abnormal ESS scores indicating daytime sleepiness did not differ from patients with normal ESS values . When analyzing cognitive performance in patients with and without RBD, no differences were detected in the overall PANDA cognition results and the TAP scores , and no relevant differences in clinical and PSG parameters were detected between both groups .
Table 6. Cognitive parameters of patient subcohorts with and without REM Sleep Behavior Disorder .
Recommended Reading: How Long Does It Take To Die From Parkinson’s Disease
The Relationship Between Parkinsons Disease And Sleep
Its unclear whether poor sleep causes parkinsonian symptoms to worsen or whether worsening parkinsonian symptoms cause poor sleep. In many cases its likely a case of bidirectionality, with each one exacerbating the other.
Fragmented sleep and sleep deprivation appear to leave the brain more vulnerable to oxidative stress, which has been tied to the development of Parkinsons disease. Parkinsons disease is not usually diagnosed until individuals have developed sufficient motor symptoms, by which time a significant portion of brain cells have already been damaged. If poor sleep quality or having sleep disorders foreshadows the development of parkinsonian symptoms, these could be useful in early diagnosis of the disease.
More research is needed to clarify the multifaceted relationship between Parkinsons disease and sleep. A better understanding of this connection may offer medical experts the unique opportunity to screen at-risk individuals and perhaps delay the onset of the disease.
Sleep Disturbances And Sleep Disordered Breathing Impair Cognitive Performance In Parkinsons Disease
- 1Department of Neurology, Technische Universität Dresden, Dresden, Germany
- 2Sleep Centre, Department of Neurology and Department of Internal Medicine, Technische Universität Dresden, Dresden, Germany
- 3Department of Neurology, University of Rostock, Rostock, Germany
- 4German Center for Neurodegenerative Diseases , Research Site Rostock, Rostock, Germany
- 5German Center for Neurodegenerative Diseases , Research Site Dresden, Dresden, Germany
Background: Sleep disturbances and impairment of cognitive function are among the most frequent non-motor symptoms in Parkinsons disease with negative implications on quality of life of patients and caregivers. Despite the fact that sleep disturbances are a major issue in PD patients, only limited data are available regarding interactions of sleep disturbances and cognitive performance.
Objective: This post hoc analysis of the RaSPar trial was therefore designed to further elucidate sleep disturbances and their impact on cognition in PD.
Methods: Twenty-six PD patients with sleep disturbances were evaluated thoroughly including assessments of patients subjective and objective sleep quality by interview, questionnaires, and polysomnography . Cognitive performance was assessed by Parkinson Neuropsychometric Dementia Assessment and Test of Attentional Performance , and associations of sleep and cognitive function were evaluated.
You May Like: How To Get Rid Of Parkinson’s Disease
Nighttime Hallucinations Psychosis & Confusion
Nighttime hallucinations and confusion may result from any combination of cognitive impairment, dopaminergic medications, age and PD-related vision changes and lack of sleep. Psychosis may first appear after infection, trauma, surgery or prolonged hospitalization. Symptoms may range from a sensation that someone or something is standing at the side of or behind the person, to very detailed and often frightening visions. Delusions may occur as well.
Treating Parkinsons Psychosis
The first-line approach to treatment of PD psychosis involves simplification of the anti-PD medication regimen and adjusting dose timing , treating other sleep disturbances, providing a consistent and familiar sleep environment , and in more severe cases, the use of atypical antipsychotic drugs.
Most of the available anti-psychotics are always avoided in PD psychosis because they block dopamine receptors and can cause significant problems with movement. However, two anti-psychotic medications, quetiapine and clozapine, are sometimes used as they have less of an ability to worsen motor symptoms. However, data for the use of quetiapine is limited and clozapine requires the patient to undergo frequent blood draws to monitor blood counts. A newer medication pimavanserin, was approved by the FDA to treat PD psychosis. It has a different mechanism of action, and does not block the dopamine system, but rather the serotonin system, and therefore does not increase motor symptoms.
Treatment For Rem Sleep Disorder
Consider making environmental adjustments to protect the person with RBD and bed partner from injury. This may include padding the floor, creating a barrier between bed partners, or sleeping in separate beds or rooms.
Don’t Miss: What Does Parkinson Disease Affect In The Body
Drugs Used To Treat Parkinsons Disease
The common Parkinsons disease medication of carbidopa and levodopa can contribute to insomnia for some people, says Horvat. Thats because its replacing the dopamine that youve lost in Parkinsons disease, she says. Research has shown that dopamine receptors play a role in wakefulness.
Sometimes when people are first started on this medication, they will take a dose right before bed rather than closer to their dinner, says Horvat. Then theyre not able to get to sleep because the dopamine affects the reward center in the brain and gives people a high, she says.
Besides timing the medication further from bedtime, your doctor may suggest taking an extended-release capsule of carbidopa and levodopa, says Horvat. That has a lower peak dose effect, so the stimulation is milder, and it lasts a little longer. It can allow patients to have more of a baseline rather than a peak at night, which can cause the insomnia, she says.
If you suspect your medication is making sleep difficult, tell your doctor dont stop taking the medicine as prescribed, says Horvat. Sometimes we can time the medication in a different way or in some cases we do change the medication but this is not something to try to figure out on your own.
What Does Osa Look Like
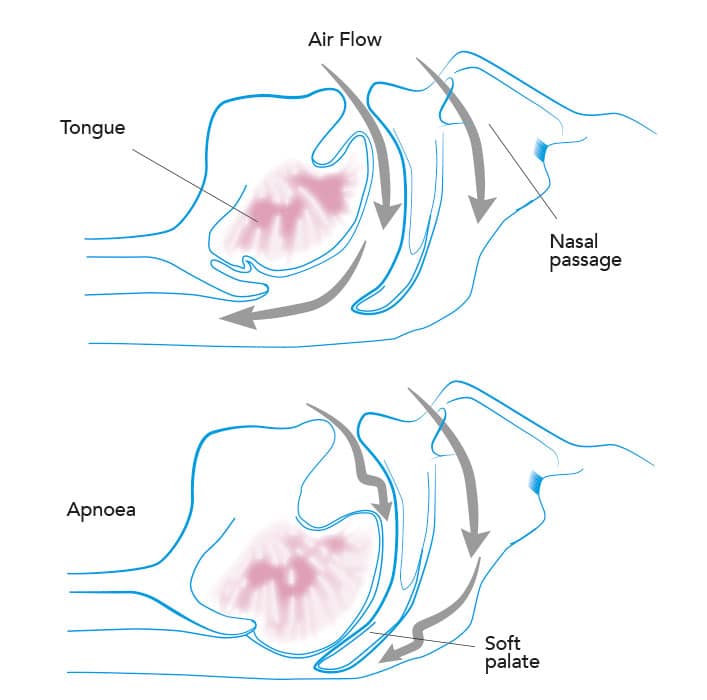
OSA is a sleep breathing disorder with several identifiable risk factors. Sleeping partners may have witnessed their loved ones choking or gasping for air in their sleep. Also, snoringthough not proof alone of OSAis still suspect if its loud and frequent.
OSA is identified as pauses of breathing during sleep which last at least 10 seconds each and which occur five times or more per hour, on average, during a full nights sleep. By comparison, healthy people without OSA experience less than three episodes of breathing pauses per hour per night.
When these pauses occur, a flurry of other processes within the body take flight: higher blood pressure and pulse, the release of stress hormones, and shifts in insulin-glucose ratios.
When experienced repeatedly over the long-term, but left untreated, OSA is a leading cause for many chronic health issues, including cardiovascular disease, hypertension, type 2 diabetes, major depression, and anxiety disorder. Untreated OSA is also a significant cause of motor vehicle accidents and dangerous mistakes and errors that occur during the day as a result of lingering daytime sleepiness.
Other classic symptoms include frequent nocturnal awakenings, and a variety of sensations upon awakening, such as shortness of breath, sore throat, dry mouth, and headache.
Recommended Reading: Does Stress Cause Parkinson’s
Ways To Manage Low Energy Activities And Sleep Issues With Parkinsons
Sleep Issues and Fatigue During the Day
Q: I am very tired by lunchtime and fall asleep in the afternoon. Is this normal?
A: People with PD may have fatigue at particular times during the day, occurring after a dose of medication. This can be very common. Sometimes the best solution is to take a short nap to regain energy for the rest of the day.
Q: My driving has been impacted by PD, causing difficulty with focus and I find myself dozing off while driving. What should I do?
A: Please be aware that medications for PD can cause falling asleep without warning. Talk with your doctor about whether this side effect may be a factor in your dozing off at the wheel. It goes without saying that the most important thing for you and those around you is to stay safe. If your fatigue and falling asleep cannot be solved with a change in medication or another approach, then you may not be able to drive anymore. Driving alternatives such as taxis, ride share options , municipal van services, and public transportation can help you maintain your independence. You can read more about the important topic of driving and PD.
Physical Activity Impacting Positive Sleep Schedules
Q: I notice that when I spend my day very active, it helps my sleep! Is this common?
Q: You suggest that to help keep a person awake during the day, his/her activities should be increased, but my husbands PD is very advanced, and he needs constant supervision to do anything. What are some good activities to consider?
How Are Sleep Problems Treated In People With Parkinsons Disease
Your provider will recommend treatments that address whats causing your sleeping challenges. Your provider may:
- Change your medication: If a medication could be causing your sleep issues, your provider may decide to adjust your treatment plan. Reducing the dose or switching medicines may solve the problem.
- Prescribe a new medication or therapy: If you have a sleep disorder, your provider will discuss your options. In some cases, your provider may recommend a new medication. If you have sleep apnea, wearing a special oral appliance can help. The device enables you to get a steady flow of oxygen, so your body doesnt gasp for air.
- Suggest lifestyle changes: Your daily habits and sleeping environment can help or hurt your sleep efforts. Setting regular sleep and wake times, keeping the room dark and avoiding electronic screens at bedtime may improve how well you sleep. If you have REM sleep disorder, your provider will discuss options for how best to protect you while you sleep.
Read Also: Best Charity For Parkinson’s Research
Identifying Sleep Apnea In Someone With Parkinson’s
We already know that PD is linked to the parasomnia known as REM sleep behavior disorder .
If a person with PD presents symptoms that resemble sleepwalking, they are urged to have an overnight test in a sleep lab. Not only is this important for treating RBD, but research suggests that, in severe OSA, its symptoms may mimic those in RBD .
Nocturnal polysomnography , more commonly referred to as an overnight sleep study, is the gold standard diagnostic assessment used to identify OSA.
If someone with PD is diagnosed with OSA, the go-to treatment is a form of noninvasive ventilation, usually along the line of therapies known as PAP, or positive airway pressure. Current research continues to support the long-term use of PAP therapy to treat OSA in people with PD. Kaminska et al found that PAP therapies improved the overall non-motor symptom burden of PD .
Rapid Eye Movement Sleep Behavior Disorder
Rapid eye movement sleep behavior disorder is a parasomnia that arises out of REM sleep and leads to a loss of paralysis of skeletal muscles where patients may exhibit dream enactment behavior . These behaviors during sleep may range from mild muscle twitches to vocalizations to violent and complex motor behaviors. This can lead to falling out of bed, self-injury, or injury to bed partners . In fact, bed partners may be the first to note these types of complex behaviors during sleep, as patients themselves are unaware of most episodes . The prevalence of RBD is estimated to be 0.51% of the general population, but up to 50% in the PD population . A diagnosis of probable RBD can be made clinically based on the presence of nocturnal behaviors associated with vivid or violent dreams . A definitive diagnosis requires polysomnography confirmation of abnormal tonic elevation and/or bursts of muscle tone measured by electromyography , termed loss of REM atonia . The underlying mechanism leading to loss of REM atonia in PD is likely mediated by accumulation of alpha-synuclein in pontine nuclei such as the sublaterodorsal nucleus and ventral medial medulla, which send inhibitory projections to the spinal motor neurons during REM sleep . For a number of patients with PD, the symptoms of RBD precede motor manifestations and a formal diagnosis of PD by a median time of 10 years, providing an opportunity for early diagnosis and neuroprotective interventions .
Fig. 2
Don’t Miss: How To Be Diagnosed With Parkinson’s Disease
