Im In Pain But I Dont Want To Take Carbidopa/levodopa Yet Because My Doctor Says It Will Only Work For Five Years Any Advice
It is true that as time passes and your disease progresses, you will have to take higher doses to replace the dopamine your body can no longer produce. However, the rate of dopamine loss is different for everyone. What your doctor may be telling you is that after taking carbidopa/levodopa for some time, you may begin to experience side effects like dyskinesia. It is important to understand that while you may experience this unwanted side effect, for example, you still benefit from the carbidopa/levodopa. If you believe your pain is Parkinsons-related, and you have already tried other medications and complementary therapies without relief, it is probably time to try carbidopa/levodopa.
Multivariate Regression Analysis With Mcid
Multivariate regression analysis was used to adjust for confounders between the two groups, and improvement in QOL over MCID was taken as the result . After adjustment for confounders, PD patients failed to achieve the MCID for EQ-5D . PD was also not a significant independent predictor of PDQ improvement over MCID. The improvement of PHQ-9 in PD patients also did not exceed that in MCID. However, the surgery age , prior depression and anxiety , and the duration of symptoms before operation was significantly correlated with PHQ-9 failing to reach MCID. In contrast, increased follow-up time was associated with an improvement in PHQ-9 over MCID .
Table 4 Multivariate regression model with MCID
What Kinds Of Pain Can Be Part Of Parkinsons
At its simplest, pain means the body hurts. When a person feels pain, nerves in the skin, joints and organs alert the brain to the location of an injury. Researchers have found that in early PD, there are already changes in the way that the body detects and regulates pain. Pain is complex and can take many forms. In PD, pain tends to affect the side of the body where motor symptoms first appeared. If your PD started with a tremor in the right hand, youre more likely to develop pain in the right shoulder, wrist or fingers. Here are a few common types.
Musculoskeletal pain
Musculoskeletal pain is experienced by up to 75 percent of people with PD and includes pain in the muscles, bones or skeleton. It is related to rigidity and decreased movement, and to arthritis. Many people with PD experience muscle cramps and tightness in the neck, spine and arms. Muscles may feel stiff or achy. Joint pain, especially in one shoulder, is also common. Its not uncommon for people with PD to be diagnosed with frozen shoulder or rotator cuff problems, and even undergo surgery.
Dystonic pain
Neuropathic pain
Central pain
Central pain affects about 10 percent of people with PD at some point. It can be difficult to describe but may include a vague, constant boring sensation abdominal pain, reflux, shortness of breath or feeling flushed painful sensations around the mouth, genital or rectal areas or simply pain all over.
Don’t Miss: What Not To Eat With Parkinson’s
What Type Of Pain Occurs With Parkinsons Disease
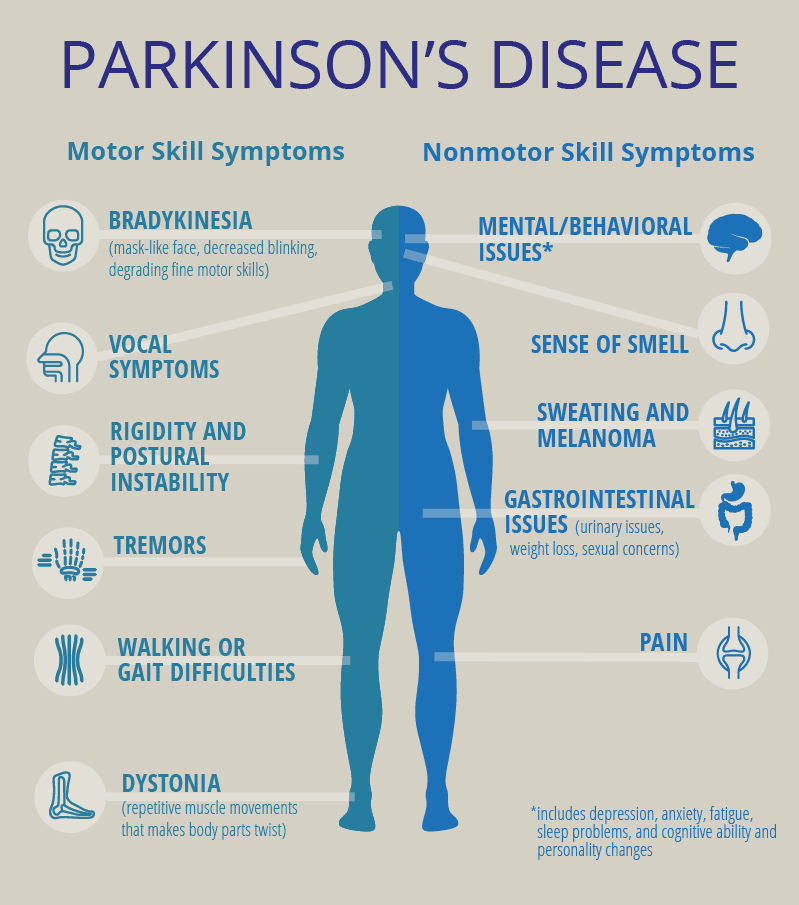
The types of pain associated with Parkinsons include: aching or burning pain from muscles or skeleton, sharp pain from a nerve or nerve root, numbness or pins and needles pain also radiating from a nerve or nerve root, pulsing or aching pain that results from tightness or ongoing twisting and writhing movements , restlessness caused from akathisia, and sudden, sharp burning pain that occurs for no known reason.
Shooting Pain And Paraesthesia
Radicular pain is a sharp pain that shoots down a limb and often affects fingers or toes. Paraesthesia is sometimes described as a feeling of pins and needles or perhaps numbness in a limb which has fallen asleep. Such pain is usually related to trapped nerves in the spinal cord and can feel similar to an electric shock, a tingling or a burning sensation.
Treatment: Painkillers and exercise will generally settle the pain. If not your specialist may refer you for tests such as an MRI scan to check for a trapped nerve in the spinal cord.
You May Like: What Are The New Treatments For Parkinson’s Disease
Inflammation May Contribute To Both Joint And Nerve Degeneration
byNancy Walsh, Contributing Writer, MedPage Today June 9, 2021
Patients with osteoarthritis are at increased risk for developing Parkinson’s disease, a longitudinal Taiwanese study found.
Incidence rates for developing Parkinson’s disease were 0.99 per 1,000 person-years among patients with osteoarthritis compared with 0.71 per 1,000 for controls, reported Shin-Liang Pan, MD, PhD, and colleagues from the National Taiwan University in Taipei.
Accordingly, the risk among patients with osteoarthritis was 41% higher compared with controls, with an adjusted HR of 1.41 , the researchers wrote online in Arthritis Care & Research.
It is now recognized that inflammation plays a major role in the development of osteoarthritis, while neuroinflammation is characteristic of Parkinson’s disease.
“Because a growing body of literature reports that peripheral inflammation may induce neuroinflammation in the brain, leading to neurodegeneration, we hypothesized that having osteoarthritis may increase people’s risk of later developing Parkinson’s disease,” Pan and colleagues wrote.
Therefore, they analyzed data from Taiwan’s National Health Insurance system, which covers more than 97% of the population, identifying 33,360 individuals ages 50 to 64 who were diagnosed with osteoarthritis during the years 2002 to 2005, matching them by age and sex with the same number of controls.
- Knee or hip osteoarthritis, HR 1.55
- Non-knee or hip, HR 1.42
- Uncategorized, HR 1.32
Disclosures
Common Skeletal & Bone Changes With Pd
- Frozen shoulder: stiffness, pain and loss of range of movement in the shoulder, many people experience this symptom before a PD diagnosis.
- Flexed fingers, toes or feet : one finger may extend, the thumb may fold inwards, fingers may clamp down onto the palm. In the leg, the foot may flex down or turn in, the big toe may flex upward while the other toes curl under.
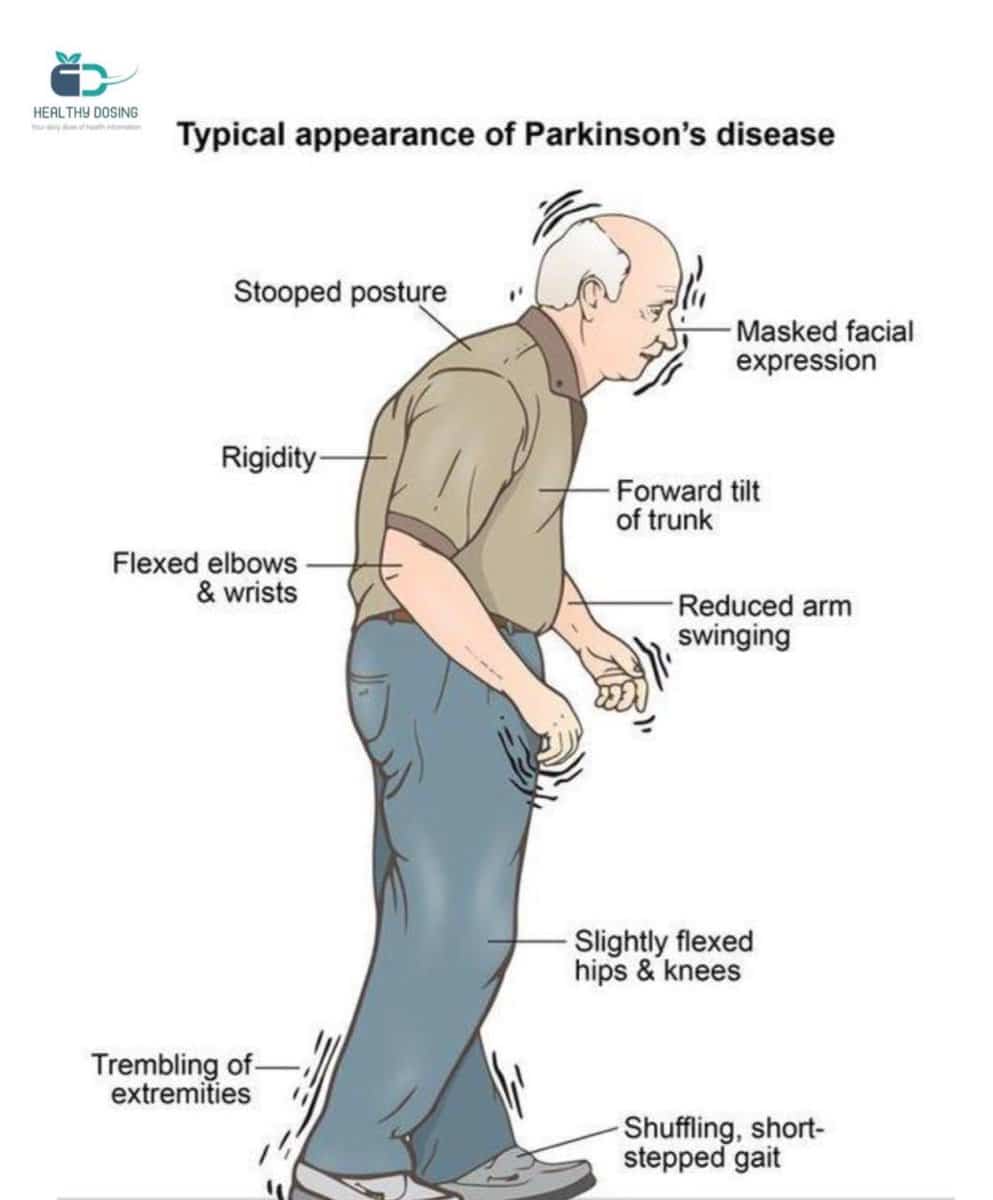
- Stooped posture : the spine bends forward when walking, in the most severe cases by as much as 90 degrees. This posture arises because the hips and knees are flexed and will go away when lying down.
- Leaning sideways : involuntarily tilting of the trunk to one side when sitting, standing or walking always to the same side.
- Scoliosis: sideways twisting, or curvature, of the spine.
- Dropped head : the head and neck flex forward the chin may drop all the way down to the sternum or breastbone .
- Bone fractures: people with PD are at risk of broken bones from falling, especially from landing on the hip. Kneecap fractures also are common, painful and sometimes overlooked.
- Low bone density/osteoporosis: bones may become weak and at risk for osteoporosis from lack of weight-bearing exercise, like walking, and from too little calcium and vitamin D. Other risk factors for osteoporosis include older age, female sex, low body weight, and smoking. A person with PD who has osteoporosis is more likely to break a bone if they fall.
Recommended Reading: Can Acupuncture Help With Parkinson’s
Potential Complications Of Missing Medication
The consequences of missing Parkinsons medication can vary enormously. Some people can tolerate a missed tablet without experiencing any major effects. Others become immobile. However, in some situations, missing dopaminergic medication can precipitate a condition known as neuroleptic malignant like syndrome, associated with fever, confusion, raised concentrations of muscle enzyme, and even death. This syndrome is most common in people with more severe Parkinsons symptoms and those on the largest doses of levodopa.6
Survival Of The Implant In Patients With Pd
In 2018, Rondon et al. revealed that the overall survival of TKA at 2, 5, and 10 years was 95.2%, 89.8%, and 66.2%, respectively . In 2019, Rong et al. found a survival rate of 87.5% at 60 months . In the study by Baek et al. published in 2021, a KaplanMeier survival analysis with revision of either component as an endpoint in the PD and control groups estimated an 89.7% and 98.3% chance of survival over 10 years, respectively . It should be noted that the three articles mentioned above show different survival rates that we can neither understand nor explain. Unfortunately, difficult-to-explain data such as these are frequent in the literature.
You May Like: What Not To Eat With Parkinson’s Disease
Peripheral Neuropathy And Parkinsons Disease
A number of studies have tried to determine if PN is more common among people with PD as opposed to people without PD. PN is a relatively common condition in the general population, which makes it difficult to ascertain whether or not it is even more common among people with PD.
The available studies have varying results and are difficult to compare with each other as they:
- Include different types of populations of people with PD
- Assess peripheral neuropathy differently
- Assess for causes of peripheral neuropathy differently
A recent review looked at all the available data and determined that large fiber neuropathy was present in 16% of patients with PD, about double the prevalence of this condition in the general population. Skin biopsy-proven small fiber neuropathy was present in over 50% of people with PD, although this result was based on a small sample of patients.
Types Of Knee Replacement Surgery
The types of knee replacement surgery include- Total Knee Replacement Surgery in which both of your knee joints are replaced, Partial Knee Replacement Surgery in which only one of your knee joints is replaced in a smaller operation with a shorter hospital stay and recovery period, Kneecap replacement and Complex or revision knee replacement. The type of surgery required will be decided by your orthopaedic surgeon after taking into account your condition.
Recovering from a total knee arthroplasty or knee replacement and managing the post-operative pain is done with many aids like self-administered analgesics. Recovery begins right after the surgery with managing to stand and walk on the first day and to be able to do daily activities at home after discharge. The average duration of hospital stay is generally 5-8 days but can vary from person to person. Walkers or crutches are generally required for ease of movement and subsequently, physiotherapy is also essential for a smooth and quick recovery. It takes about 3 weeks to 3 months for the knee to recover to a point where one is back to full activity and about a year for absolute recovery to occur.
During recovery after total knee arthroplasty, its necessary for the patient to try and progressively remain active.
You May Like: Best Probiotic For Parkinson’s Disease
Types Of Parkinsons Pain
Most of the time, discomfort in muscles and joints is secondary to the motor features of Parkinsons lack of spontaneous movement, rigidity, and abnormalities of posture what is known as musculoskeletal pain. The most commonly painful sites are the back, legs, and shoulders and it is usually more predominant on the side more affected by parkinsonism.
But there are many other categories of pain associated with Parkinsons disease. Radicular or neuropathic pain is experienced as a sharp pain that can start in the neck or lower back with radiation to arm or leg respectively and is often associated with numbness or tingling, or a sensation of coolness in the affected limb. It is usually secondary to a pinched nerve due to something like a slipped disc.
Dystonia related pain occurs as its name suggests, at times of dystonia most often experienced in the foot, neck or face and arm at different points in the dosing schedule, particularly the off phase when there is not enough dopamine replacement but can uncommonly also occur at peak-dose times. It can be one of the most painful symptoms those with Parkinsons can face.
Akathisia pain is experienced as restlessness, a subjective inner urge to move, an inability to stay still and the inherent feelings of discomfort that it brings. It is primarily experienced in the lower limbs and can often be relieved by walking around.
Also Check: Tremor Predominant Parkinson Disease Treatment
Wear Loose Comfortable Clothes
As I mentioned above, you will have staples in your knee for about 12 days. Short pants or athletic shorts make it easy to dress and also keeps the fabric from long pants off the wound.
Even after the staples have been removed long pants especially denim can cause discomfort. If you have to wear long pants, I recommend thin fabric or zippered pants that are specially made for post-surgery . Check out my article on what to wear after TKR.
This is another good reason to plan your surgery and recovery during warmer weather when less clothing is necessary.
Recommended Reading: Who Is The Best Parkinson Doctor
What Causes Parkinsons Disease
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
What Does Leukemia Pain Feel Like
Medically Reviewed by: Dr. BautistaUpdated on: May 28, 2020
Leukemia is a cancer of the bone marrow cells and it can come with a wide range of symptoms. These symptoms might be subtle and slow at first and include things like fatigue, headaches, unintentional weight loss, abnormal bleeding and bruising, and frequent infection. Although leukemia cant be diagnosed solely on these symptoms, being aware of them is important. 1
Leukemia is a type of cancer that typically affects healthy blood cells in the bone marrow. Instead of creating normal blood cells, the bone marrow will begin to produce abnormal blood cells called leukocytes. This blood cancer usually leads to an overproduction of white blood cells which can overcrowd and outnumber the red blood cells within the body.7 These abnormal white blood cells can cause havoc on your system, leading to a number of complications and side effects.
These are the four main types of leukemia:
- Acute myeloid leukemia
- Acute lymphocytic leukemia
- Chronic lymphocytic leukemia
As you can see, there are several different types of leukemia. One of the most common symptoms to look for in both children and adults is bone and joint pain.
If youre wondering exactly what does leukemia bone pain feel like, read on. Our guide will detail this and more from the experts at ITC.
You May Like: What Does A Parkinson’s Tremor Look Like
Identify The Cause Of The Pain
The first step in treating pain is to try to identify the cause. As I noted in the last essay, there are many different causes of pain for people with PD. If we look at the most common pain problems, low back and neck pain, we can see that there are many different causes for each. Many doctors order x-rays of the spine for these conditions, and they may be needed. The main problem with x-rays of the spine is that they always show arthritis, which is because virtually everyone over the age of 60 has arthritis in the spine. Whether thats the cause of the pain or not is usually not clear.
However, x-rays will show if theres a compression fracture , or a tumor. Since older women frequently develop compression fractures even without a fall, this can be important because we know then that the pain is likely severe, but time limited, and will resolve in a month or two. This makes it easier to treat with strong medication, like narcotics, because there is less concern for addiction. X-rays do not show discs, but disc herniation is much less common in older people so its of less concern.
Physical Therapy
Alternative treatments
Chiropractors focus entirely on spine pain and may be very helpful. Since many medical doctors are not very familiar with PD, I assume that many chiropractors probably arent either. Therefore it will be helpful to find one who is familiar with PD. Probably the best way to do this is through a Parkinsons Disease support group in your area.
The Parkinsons Disease News Today Forums Are A Place To Connect With Other Patients Share Tips And Talk About The Latest Research Check Them Out Today
PD pain can resemble pain from other disease processes, especially as the patient ages and faces a multitude of other pain-causing conditions such as arthritis, spine degeneration, poor muscular conditioning, and such. In my case, PD pain is distinguished by the following:
- The progression of body pain correlated with the progression of the disease over time.
- Levodopa, a dopaminergic therapy, successfully reduces the pain.
- The pain is worse during off periods.
My PD pain also has a particular characteristic: stinging , irritating tingling, burning, and muscle heaviness with increased pain on movement. This pain happens over large regions of the body and varies in severity. At its worst, it can last several days and reach level 7, inducing spontaneous tears.
PD with episodic chronic pain is disabling in several ways. First, high levels of pain obstruct clear thinking. Second, high levels of pain induce the fight-or-flight response, which interferes with emotion management. Third, the amount of energy necessary to manage it is very tiring . Chronic PD pain entails much more than body symptoms.
I have been a communicator most of my life, but it remains a struggle to find words that describe the unique character of PD pain. If you experience PD pain, please share your descriptors in the comments. Together we may find a common dialogue that will help others.
Don’t Miss: Does Parkinson’s Affect Your Legs

