Rbd May Be Earliest Marker Of The Movement Disorder
A relatively rare sleep disorder characterized by acting out dreams during REM sleep — often violently — is closely linked to the movement disorder Parkinson’s disease and may warn of Parkinson’s decades before diagnosis.
People with REM sleep behavior disorder do not have normal muscle paralysis during the dream phase of sleep. The loss of motor inhibition is generally accompanied by often frightening dreams, which are “acted out” with arm flailing, kicking, punching, and sometimes, screaming and shouting.
“If patients are running in their dream, they ‘run’ in their beds. If they are fighting with someone in their dream, their arms may flail wildly. This can be dangerous for the patient and the patient’s bed partner,” Marina Romero-Ramos, PhD, of Aarhus University in Denmark, told MedPage Today.
The prevalence of RBD has been estimated to be from 0.38% to 1% in the general population, but the sleep disorder is much more common in patients with Parkinson’s disease.
In one study, 69% of patients with a diagnosis of Parkinson’s reported symptoms consistent with RBD, while no increased risk was seen in patients with the related movement disorders essential tremor and restless leg syndrome.
Even more significant, a large percentage of people with RBD go on to develop Parkinson’s years and even decades later, said Miranda Lim, MD, PhD, of the VA Portland Health Care System in Oregon.
“Of course these studies will take a long time — probably decades,” she said.
Limit Lights In Your Room
Minimize your exposure to artificial lights when preparing for bed. Sleep in a cool, dark place. Avoid bright lights when sleeping. You could keep dim night lights if sleeping in complete darkness is uncomfortable.
Avoid watching television and using mobile devices before bed or lying in bed. These devices emit blue lights that could affect your sleeping habits.
Dont Miss: Social Security Disability Parkinsons
Excessive Daytime Sleepiness In Pd
Excessive daytime sleepiness is a common symptom in PD and can occur anywhere from 15 to 21% early in the disease course and up to 46% as the disease progresses . A study of early and untreated PD showed that EDS may be related to disease progression and is independent of other sleep disorders, while others have shown that dopaminergic medication appears to increase EDS in a dose-dependent fashion . Some studies have also suggested an association of EDS in PD with depression . Interestingly, patients with PD and EDS appeared to have reduced uptake in the basal ganglia on dopaminergic terminal imaging compared to those without EDS . The PD and EDS groups also have worse scores on motor, nonmotor, autonomic, and cognitive testing . This suggests that more severe disease could be a contributing factor to development of EDS, in addition to dopamine medication levels .
The presence of EDS negatively impacts quality of life in PD. One study evaluated 198 patients with PD using the Parkinsons Disease Questionnaire 39 , a measure of quality of life . This study demonstrated that those with PD and EDS had a significantly lower overall score on the PDQ-39 than those without EDS , as well as individual emotional, social, and physical domains measured by this survey . EDS in PD also represents an additional risk of falling. One study evaluated 120 patients with PD and found that every point increase on the Epworth Sleepiness Scale was associated with a 20% higher risk of falling .
Read Also: How Do You Develop Parkinson’s Disease
Possible Signs Of Rbd
- You experience dream enactment behaviors.
- Your loved one appears to be acting out their dreams.
- You or a loved one awakens to find that injuries or damage have been sustained during sleep.
In any of these cases, please consult your physician. The good news? RBD may be treated successfully with clonazepam and melatonin.
You may also wish to safety-proof your sleeping place by padding corners of furniture, installing a bed rail, and putting dangerous items out of easy reach.
Take heart, however not everyone who experiences RBD goes on to develop PD.
Symptoms And Diagnostic Considerations
Rapid Eye Movement Sleep Behavior Disorder is a non-familial sleep disorder, characterized by the loss of the inherent muscle atonia observed during normal REM sleep. This phenomenon is often referred to as REM Sleep without Atonia . Whilst isolated RSWA is frequently an incidental finding in sleep studies, it forms the substrate of the dream enactment behavior which defines RBD. Here, individuals experience vivid dreams which they act out during sleep.
It is important to remember that dream enactment and limb movements during sleep can occur in the healthy population, often in the context of heightened emotional states . The same symptoms may also be experienced during withdrawal from sedatives or alcohol. In non-pathological dream enactment, individuals typically respond to dream content during the transition from REM sleep to the awake state and while maintaining REM atonia during much of the REM period. In contrast, RBD individuals will maintain REM sleep during and immediately after most of their dream enactments. As acute dream enactment is generally self-limiting, the chronicity of symptoms is a key distinguishing factor, and forms part of the diagnostic criteria for RBD .
Don’t Miss: What To Expect Living With Parkinson’s
How Can I Reduce The Consequences Of This Sleep Disorder
Treatment usually involves a combination of medication and a change in sleeping habits.
Before you see a doctor, you can use strategies to reduce the impact of these dreams on you and your partners safety. Here are some of these strategies:
- Make sure there are no sharp objects near the bed
- Place the bed against the wall or put pillows to prevent falls
- Consider installing safety rails on the bed
- Place sharp objects and furniture away from the bed
- Move the bed away from windows
- Sleep in separate rooms if your behaviour becomes too much of an inconvenience
An occupational therapists advice can also provide you with several concrete solutions to make your sleep environment safer and prevent injuries.
How Are Sleep Problems Diagnosed In People With Parkinsons Disease
If youre having problems sleeping, sit down with your healthcare provider to discuss the issue in detail. Your provider will ask you questions to better understand your symptoms.
Be prepared to explain when sleep disruptions happen and how they affect your life. Keeping a sleep journal for a few weeks can help you remember the details.
If your provider suspects you may have a sleep disorder, they may recommend you have a sleep study. This overnight test uses electrodes attached to your skin to track how your body functions when youre sleeping.
Read Also: Does Senator Susan Collins Have Parkinson’s Disease
Rapid Eye Movement Sleep Behavior Disorder
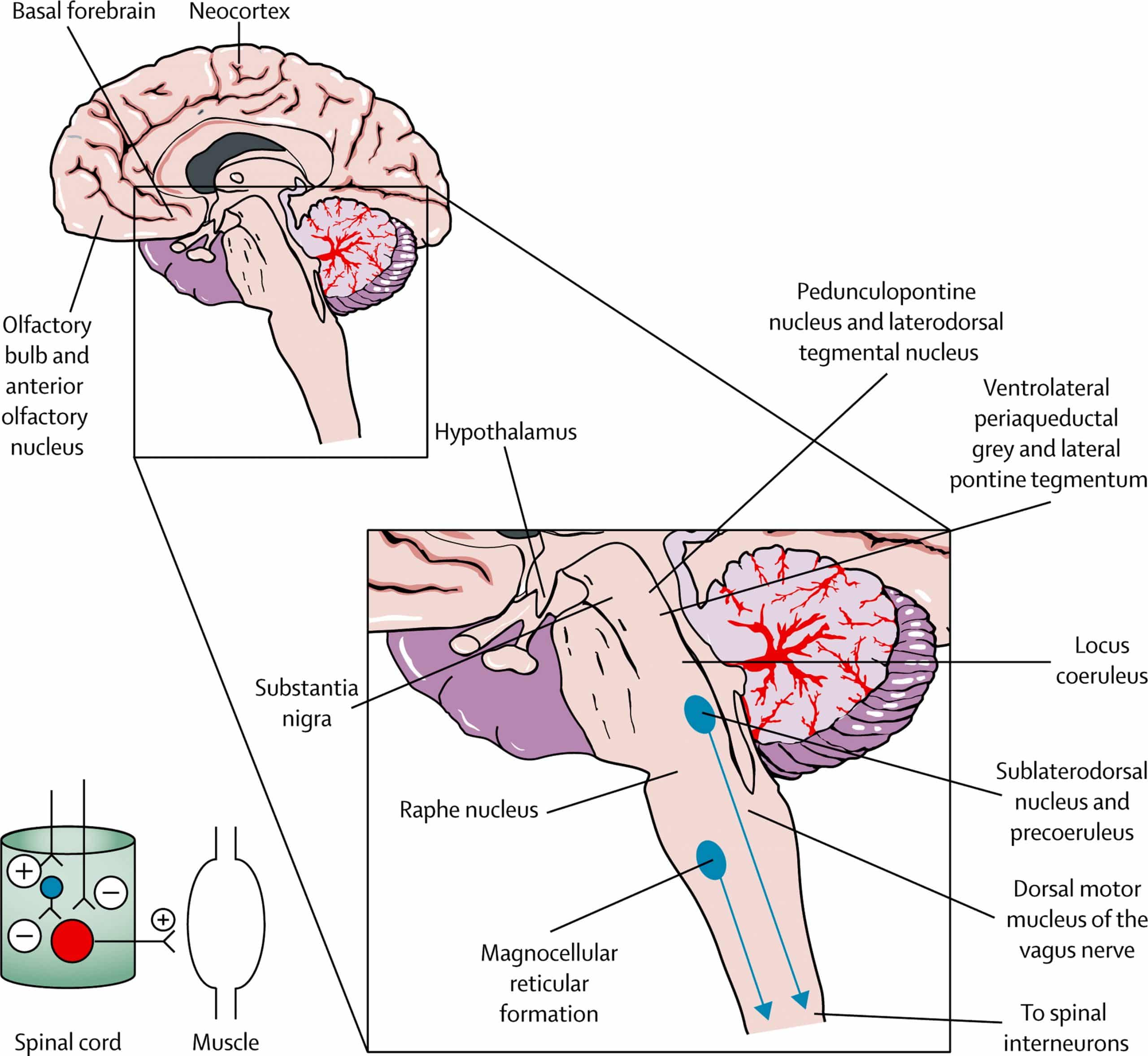
Rapid eye movement sleep behavior disorder is a parasomnia that arises out of REM sleep and leads to a loss of paralysis of skeletal muscles where patients may exhibit dream enactment behavior . These behaviors during sleep may range from mild muscle twitches to vocalizations to violent and complex motor behaviors. This can lead to falling out of bed, self-injury, or injury to bed partners . In fact, bed partners may be the first to note these types of complex behaviors during sleep, as patients themselves are unaware of most episodes . The prevalence of RBD is estimated to be 0.51% of the general population, but up to 50% in the PD population . A diagnosis of probable RBD can be made clinically based on the presence of nocturnal behaviors associated with vivid or violent dreams . A definitive diagnosis requires polysomnography confirmation of abnormal tonic elevation and/or bursts of muscle tone measured by electromyography , termed loss of REM atonia . The underlying mechanism leading to loss of REM atonia in PD is likely mediated by accumulation of alpha-synuclein in pontine nuclei such as the sublaterodorsal nucleus and ventral medial medulla, which send inhibitory projections to the spinal motor neurons during REM sleep . For a number of patients with PD, the symptoms of RBD precede motor manifestations and a formal diagnosis of PD by a median time of 10 years, providing an opportunity for early diagnosis and neuroprotective interventions .
Fig. 2
Sleepwalking Rem Sleep Behavior Disorder Linked With Parkinson Disease Risk In Men
Symptoms of sleepwalking and/or REM sleep behavior disorder in men were significantly associated with higher odds of having Parkinson disease , with PD-related neurodegeneration potentially impairing arousal regulation during sleep.
Men experiencing symptoms of sleepwalking and/or REM sleep behavior disorder may be at greater risk of having Parkinson disease , according to study findings published this week in JAMA Network Open.
As one of the most common nonmotor symptoms in PD, sleep-related symptoms affect more than 75% of people with the condition. Among these symptoms, researchers highlight that REM sleep behavior disorder and sleepwalking, which is caused by non-REM sleep, both have high prevalence in PD.
Given that sleepwalking is generally considered a rare condition in adults , this prevalence in patients with PD appears unusually high, but to our knowledge, no study to date has included a group of individuals without PD in direct comparison for risk estimation, said the study authors.
Researchers conducted a cross-sectional study of data from the Health Professionals Follow-Up Study , a population-based cohort of male health professionals, to assess the association between probable sleepwalking and probable RBD with PD.
Compared with those without sleep parasomnias, participants with probable sleepwalking or probable RBD were more likely to have longer sleep duration , prevalent daytime sleepiness , hypnotics use , and restless leg syndrome .
Read Also: How Effective Is Parkinson Medication
Rem Sleep Behaviour Disorder Is A Risk Factor For Parkinson’s Disease
Patients suffering REM sleep behaviour disorders dream nightmares in which they are attacked and pursued, with the particularity that they express them by screaming, crying, punching and kicking while sleeping. Lancet Neurology has published the third consecutive work in five years about the relationship between this disorder and Parkinson’s disease. The first work showed in 2006 that 45% of patients who suffer this sleep disorder develop Parkinson’s disease and other neurodegenerative diseases caused by a lack of dopamine in the brain. The second article discovered that neuroimaging tests that measure dopamine in the brain, such as the brain SPECT, are useful to identify patients with REM sleep disorders with increased risk of developing a neurodegenerative diseases such as Parkinson’s disease.
The new study applied brain SPECT to conclude that the levels of dopamine in the brain are quickly lowering over the years in patients with REM sleep behaviour disorder. This neuroimaging technique becomes the first tool to detect the disease progression at an early stage. The first author of the three articles is Dr. Àlex Iranzo, doctor from the Neurology Service at the Hospital Clínic of Barcelona, researcher at the Biomedical Research Institute of August Pi i Sunyer and member of the Multidisciplinary Sleep Disorders Unit , and the senior authors were to Dr. Joan Santamaria and Dr. Eduard Tolosa, from the same institution.
Rem Sleep Behavior Disorder
Kimberly Truong, Sleep Physician
Fact Checked
Our team of writers, editors, and medical experts rigorously evaluates each article to ensure the information is accurate and exclusively cites reputable sources. Learn More
We regularly assess how the content in this article aligns with current scientific literature and expert recommendations in order to provide the most up-to-date research.
Normally during REM sleep, the body experiences temporary paralysis of most of the bodys muscles while the brain is active and dreaming. This allows us to dream quietly and safely throughout the night. For individuals with REM sleep behavior disorder, paralysis does not occur during the REM stage. Instead, their body and voice perform their dreams while they remain asleep.
Less than one percent of people are estimated to have REM sleep behavior disorder. It usually begins after age 50, and the disease is associated with other neurodegenerative disorders, including Parkinsons disease, Lewy body dementia, and multiple system atrophy. Symptoms often worsen with time. The condition usually requires treatment because it increases the risk of injury to oneself and their bed partner.
Read Also: Is Parkinson’s Disease Chronic
Causes Of Rem Sleep Disorder
The exact cause of RBD is unknown, but it may happen along with degenerative neurological conditions such as Parkinson’s disease, multisystem atrophy , and diffuse Lewy body dementia. In 55% of people, the cause is unknown, and in 45%, itâs linked with alcohol or sedative-hypnotic withdrawal, tricyclic antidepressant , or serotonin reuptake inhibitor use or other types of antidepressants .
RBD often happens several years before the development of these neurodegenerative diseases. In one study, 38% of people diagnosed with RBD developed Parkinson’s disease within an average of 12 to 13 years after RBD symptoms began. Also, RBD is seen in 69% of those with Parkinson’s disease and multisystem atrophy. The relationship between RBD and Parkinson disease is complex not everyone with RBD will develop Parkinson’s disease.
Show Sources
Somnolence And Excessive Daytime Sleepiness
Somnolence and EDS occur commonly in PD. Etiologies of somnolence in PD include reversal of the sleepwake cycle, the disease process itself, disrupted sleep due to a variety of motor and nonmotor causes, and the use of dopamine agonists and other antiparkinsonian medications. Several studies have found that dopamine agonists are more likely to cause somnolence than levodopa. The soporific effects of the commonly used dopamine agonists appear to be similar as assessed by Epworth Sleepiness Scale scores.36
EDS occurs in PD patients, and is usually associated with dopamine agonist use. EDS may occur with use of other PD medications, including levodopa/carbidopa. However, EDS as measured by the ESS does not always correspond to shortened sleep latency as quantified by the Multiple Sleep Latency Test .10 In addition, nocturnal sleep disturbance as measured by polysomnogram may not account for the severity of daytime sleepiness in PD patients with EDS.10
Recommended Reading: Reishi Mushroom Parkinsons Disease
Read Also: Does Parkinson’s Affect Cognition
Search Of The Published Literature
Literature search and study selection processes are shown in Fig. 1. The electronic search yielded 3282 records, where 3203 were excluded due to irrelevant or duplicate articles. The remaining 79 studies were evaluated further. Of these, 32 studies were excluded due to the following reasons: patients without PD , reported the relation between PD and other diseases , and review articles . Finally, 47 studies met the inclusion criteria and were included in final analysis [8,9
Using The Genetics Of Rem Sleep Behavior Disorder To Predict Parkinson’s Disease Risk And Progression
When people develop REM sleep behaviour disorder, where they act out their dreams in their sleep, its often a precursor to an even more serious illness.
Up to 80 percent of people with this disorder later develop Parkinsons disease, Lewy body disorder or, more rarely, multiple system atrophy. Thats why identifying those at risk of having the sleep disorder, known as RBD, would also flag those at risk for the other neurodegenerative illnesses.
At McGill University, geneticist and neuroscientist Lynne Krohn, a PhD student, is screening genes to find those that increase the risk of RBD. So far, shes found five genes that make people more susceptible when the genes are mutated, or damaged.
These same genes are also implicated in Parkinsons disease risk, Krohn says.
The over-arching goal is better treatment of Parkinsons disease.
Using blood and DNA samples from volunteers diagnosed with RBD who are at risk of converting to neurodegenerative diseases, Krohn will screen the samples for these genes.
Shell then compare them with samples from people who are healthy, and create a polygenic risk score. She hopes that score will predict who is most likely to develop RBD, and subsequently, how fast RBD might convert to one of the other neurodegenerative disorders.
We have evidence that these genetic mutations are affecting how fast people develop Parkinsons disease or Lewy body dementia or, in some cases, multiple system atrophy, once they already have RBD, Krohn says.
Also Check: How Are You Diagnosed With Parkinson’s
Current Research: Rbd And The
The tests described in this section are used solely in experimental settings and therefore clinicians are not able to use them in the clinical RBD diagnostic or prognostic process. The majority of RBD research focuses upon the relationship between RBD and subsequent -synucleinopathy development. In particular, the search for biomarkers which identify underlying -synuclein pathology and predict RBD phenoconversion is perhaps the most relevant for clinical practice. As discussed previously there are no genetic markers with predictive power for RBD phenoconversion, and while rating scales may identify individuals with a high risk of phenoconversion, they do not have a binary outcome measure- a feature which is essential in prognostic testing.
Biomarkers for RBD conversion are essentially testing whether the RBD features of an individual are due to underlying -synuclein pathology or not. This can be done by testing for misfolded, pathological -synuclein in peripheral tissues and fluid samples. Dermal nerve fibers , cerebrospinal fluid , submandibular glands , colonic submucosal nerve fibers , salivary glands , and parotid glands have all been found to contain pathological -synuclein proteins in idiopathic RBD patient populations and confirmatory PD populations. Such investigations are in their infancy but show promise as a basis for relatively low-cost clinical diagnostic biopsy tests for alpha-synucleinopathy in RBD patients.
Sleep Abnormalities Linked With Increased Pd Risk In Older Men
Older adults who reported longer total sleep time, lower rapid eye movement sleep percentage, and higher minimum oxygen saturations during REM sleep had an increased risk of developing Parkinson disease .
Reduced rapid eye movement and other abnormalities during sleep were associated with a greater risk of Parkinson disease development in older adults, according to study findings published in Sleep.
Characterized by motor flunctuations, PD is also commonly associated with nonmotor symptoms such as sleep-wake disturbances. Study author Abidemi I. Otaiku, BMBS, BSc, AKC, Department of Neurology, Birmingham City Hospital, noted that 40% to 90% of patients experience at least 1 sleep condition, in which certain disorders, including REM sleep behaviour disorder , can predate the onset of PD by years or even decades.
Despite known alterations in the sleep macro- and microstructure of people with PD, as measured via polysomnography and sleep electroencephalogram , respectively, he said that it remains unknown whether these factors may also precede the development of PD.
Establishing the temporal relationship between objective sleep alterations and the development of PD may have important value for early diagnosis, better understanding the pathophysiology of PD, and might open up new approaches for delaying or preventing PD onset, noted Otaiku.
Reference
Don’t Miss: What Brain Structure Is Affected By Parkinson’s
