Why Is This Important
This study reveals unmet needs among those in the late stages of Parkinsons and their families. These issues are likely to apply in other chronic progressive neurological disorders such as dementia.
The shift from hospital care to community services is complicated in England by the separation in social care and healthcare funding, and the separation in organisation of different service providers. This research underlines problems with this model.
The research demonstrates the importance of Parkinsons Disease Nurse Specialists in caring for patients in their homes by expertly managing symptoms, providing personalised information and a link to hospital services, and offering emotional support. It highlights the importance of finding better ways of managing and living with deterioration and eventually planning end of life care. In parallel, informal caregivers could be better supported to help people with late-stage Parkinsons retain their sense of self, maintain day-to-day life, and allow them to stay in their own homes for longer.
The Last Year Of Life In Parkinson’s Disease
The study also examined nearly 45,000 hospitalizations in people with terminal Parkinson’s, meaning their end-of-life period.
Of those with terminal PD, the most common reasons for being in the hospital were:
- Infection
- Heart disease
- Lung disease that was not from an infection
Less common causes for hospitalization were problems related to the stomach or intestines, muscles, nervous system, or endocrine system .
It is not surprising that infection was the most common hospitalization before death, as people with Parkinson’s are vulnerable to developing a number of infections as a result of their disease. For example, bladder dysfunction in Parkinson’s increases a person’s risk of developing urinary tract infections, which can become life-threatening if not detected and treated promptly.
In addition, research suggests that aspiration pneumonia is 3.8 times more common in people with Parkinson’s as compared to the general population. It has also been consistently reported to be the main cause of death in people with Parkinson’s.
Aspiration pneumonia results from underlying swallowing difficulties, which leads to stomach contents being inhaled into the lungs. Immobilization and rigidity, which can impair phlegm removal, also contribute to the development of pneumonia in people with Parkinson’s.
What Can You Expect From Parkinsons Disease
Because Parkinsons disease follows a broader pattern, it moves at different speeds among different people and brings out changes at a different rate. An individual affected by the disease shows the symptoms over a period, and they become worse with time. It is also possible for the patients to show new signs from time to time throughout the period.
The Parkinsons disease does not have any effect on your lifespan. However, it does possess the ability to change on how you lead the life. What we are talking about is the quality of life. Parkinsons disease changes it, and after a decade, many people will show some significant symptoms such as physical disability or dementia.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
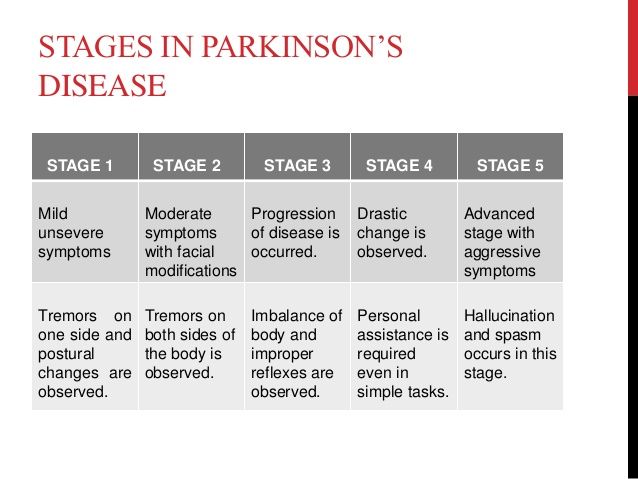
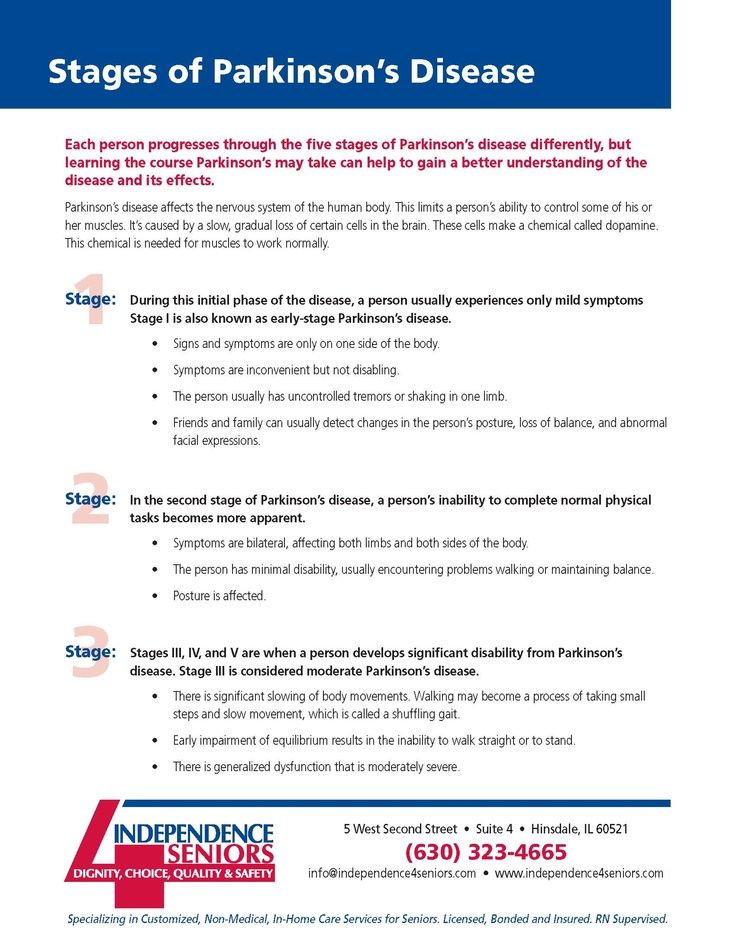
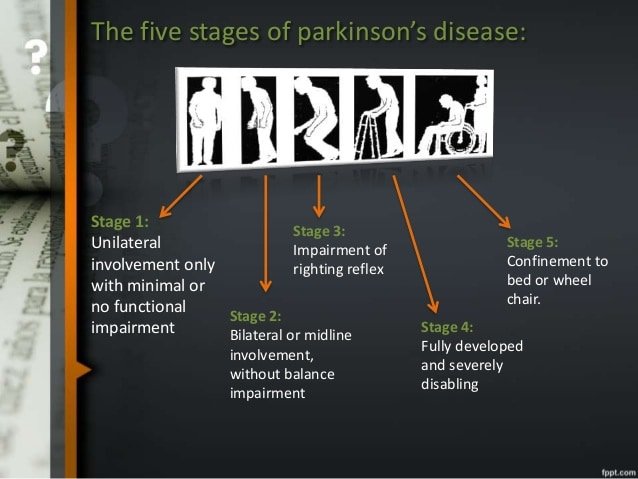
Stages Of Parkinsons Disease
Parkinsons follows a predictable pattern. In the early stages, symptoms are inconvenient. By the end, they are incapacitating.
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
Don’t Miss: Is Parkinson’s An Autoimmune Disease
Pharmacologic Issues At End
As PD progresses there are fewer dopaminergic neurons in the substantia nigra as well as a progressively lower capacity to store exogenous levodopa and convert it to dopamine for storage and release in the remaining neurons. Additionally, as the dose requirements of levodopa increase, the patient’s functioning is inhibited before his next dose of medication . This usually takes place 24 hours after a levodopa dose and may appear as sensory , psychiatric or autonomic symptom, or progression of motor symptoms or dystonia . This is called end of dose wearing off. Wearing off has not been fully explored, but may be connected to pharmacokinetic changes, and shortening of striatal levodopa half-life resulting from progressive degeneration of nigrostriatal dopaminergic terminals . To treat motor symptoms it is necessary to deliver medication effectively. Patients with advanced PD often notice that protein-rich meals will diminish the effectiveness of levodopa doses . This can be alleviated by reducing protein intake during daytime and limiting protein intake at night to 40 grams . There are some strategies to Improve absorption of Levodopa include: advise patients to take levodopa before meals, on an empty stomach , advise patients to avoid protein-rich meals and bulk-forming foods , advise patients against lying down, and encourage them to move around, after ingesting a dose , and advise patients to mix levodopa, crushed into a powder, into sparkling liquid .
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinson’s are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinson’s only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
Also Check: Demographics Of Parkinsons Disease
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
Physical Difficulties In The Later Stages Of Dementia
The physical changes of late-stage dementia are partly why the person is likely to need much more support with daily living. At this stage they may:
- walk more slowly, with a shuffle and less steadily eventually they may spend more time in a chair or in bed
- be at increased risk of falls
- need a lot of help with eating and so lose weight
- have difficulty swallowing
- be incontinent losing control of their bladder and bowels.
The persons reduced mobility, in particular, raises their chances of blood clots and infections. These can be very serious or even fatal so it is vital that the person is supported to be as mobile as they can.
You May Like: Can Parkinson’s Run In The Family
Is Parkinsons Disease Fatal
Parkinsons disease itself doesnt cause death. However, symptoms related to Parkinsons can be fatal. For example, injuries that occur because of a fall or problems associated with dementia can be fatal.
Some people with Parkinsons experience difficulty swallowing. This can lead to aspiration pneumonia. This condition is caused when foods, or other foreign objects, are inhaled into the lungs.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Complications In Advanced Pd
While worsening of motor function and drug-induced motor complications represents a major challenge in patients with mid-stage to advanced disease, in the advanced stage of PD the most troublesome and distressful complications are usually nonmotor symptoms, including psychiatric and cognitive disorders, autonomic disturbances, and sleep disorders that significantly increase the need for supportive care. Unfortunately, these symptoms are frequently neglected in clinical practice due to limited consultation time, perception of the patient and caregivers that their symptoms are unrelated to the disease, or insufficient awareness of the clinicians, who generally focus on motor symptoms .
Proper supporting care becomes increasingly important in advanced PD. Rehabilitative and support services for patients and family become key interventions as the disease reaches its more debilitating stages and pharmacologic or surgical treatment becomes less relevant. Management of motor and nonmotor complications in advanced PD requires careful and ongoing assessment of whether symptoms are a side effect of medication or related to the progression of the disease .
Medication Issues
|
End of Dose Wears Off Symptoms in Advanced PD |
|---|
|
Systems affected |
|
Progression of motor symptoms Dystonia |
Fragmentation of Dosing
Dopamine Agonists Contraindicated
L-dopa and Dietary Proteins
Motor Issues
Dyskinesias
Dystonia
Freezing
Nonmotor Complications
Hallucinations, Delusions, Psychosis
Depression and Anxiety
Hospice Eligibility For Parkinsons Disease
Due to the progressive nature of Parkinsons disease, it can be challenging for families to know when their loved one is eligible for the support of hospice care. If a loved one has been diagnosed with six months or less to live or if they have experienced a decline in their ability to move, speak, or participate in the activities of daily living without caregiver assistance, it is time to speak with a hospice professional about next steps.
Read Also: What Is The Life Expectancy Of Someone With Parkinson’s Disease
How Long Does It Take For Parkinsons Disease To Progress
It is quite common for any individual suffering from Parkinsons disease to wonder about the unfolding of the condition. If you belong to the group that in search for the answers related to the progression of Parkinsons disease, then you will try to learn about the symptoms that you can acquire with the condition, when they start, and the changes the disease brings in the body.
The questions are basic, but Parkinsons disease is not. Like other illnesses, Parkinsons disease does not have a specific path of progression. Due to this, it is difficult to state or pin down the exact time or the path of the progression.
My Parkinson’s Story: Advanced Parkinsons
This 10-minute video alternates between an interview with a man and his wife and his palliative care team, including a doctor, nurse, clerg and social worker. The man and his wife shares his experience with late stage Parkinson’s. The palliative care team explains that their job is to support the best physical, emotional and spiritual wellbeing of the immediate family as well as help the family make end of life decisions.
Don’t Miss: Life Expectancy With Parkinson Disease
Palliative Care Management Of Non
Patients with PD can develop non-motor manifestations, categorized into autonomic dysfunction, cognitive impairment, neuropsychiatric disorders, and sleep disturbances. At the end-stage of PD, non-motor symptoms become more common and can become the most prominent medical problem, leading to increasing decline in quality of life both for patient as well as increasing caregiver burden . Non-motor symptoms occur in up to 50% of PD patients especially in association with the medication off state and may become worse by anti-PD medications . Almost one third of patients reports their non-motor symptoms to be at least as debilitating as their motor symptoms .
All patients with motor fluctuations face at least one non-motor problem during the off phase . In end-stage of PD, dementia, psychosis, and falls become more complex to manage than the motor complications as a result, managing non-motor aspects is important to increase quality of life and decrease the burden of illness . Chaudhuri and co-workers, using a new 30-item non-motor symptom screening questionnaire , found noticeably high scores among PD patients for impaired taste/smell, impaired swallowing, weight loss, constipation, urinary urgency, forgetfulness, dribbling, sadness, hallucinations, anxiety, sexual dysfunction, falling, reduced concentration, daytime sleepiness, vivid dreams, and sweating .
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
Don’t Miss: What Essential Oils Are Good For Parkinson’s Disease
Preparing For End Of Life
Whether you are a person with Parkinson’s or a relative, friend or carer, thinking about the future now may help you feel more in control and confident about what lies ahead.
This section looks at the practical and emotional issues relating to Parkinson’s and the later stages of life.
This includes decisions you may need to make and the care you would like to have, and how to put your affairs in order. There is also advice and information for carers, close family and friends, including how to arrange a funeral and finding bereavement support.
Thinking about the future now, and discussing your wishes and preferences with the people in your life, may help you feel more in control and confident about what lies ahead.
It also takes away the burden from family or friends of having to make decisions on your behalf, should you become too ill to make decisions for yourself.
For the majority of people, Parkinson’s will not significantly affect their life expectancy. However, some of the more advanced symptoms can lead to increased disability and poor health, which can make someone more vulnerable to infection.
Parkinson’s is a progressive condition. This means it will get worse over time. Its difficult to predict at what speed your Parkinson’s will progress or what symptoms you may get, because the condition is different for everyone.
Your GP, Parkinson’s nurse or specialist should be able to advise on treatments to help with this, too.
This can mean:
Motor Symptoms And Global Disability
Motor symptoms, as measured using the Unified Parkinsons Disease Rating Scale , Hoehn and Yahr Scale and the Progressive Supranuclear Palsy Rating Scale , were significant predictors of mortality in patients with PDRD. Beyer et al found higher mean UPDRS scores, 65 versus 42 , suggesting that greater motor impairment predicted death. Studies with median follow-up times ranging from 4 to 8 years estimated the association of 10-unit increases in baseline motor UPDRS Score on mortality and found statistically significant increased HRs for mortality of 1.17 up to 1.4 for each 10-unit increase in UPDRS Score. Baseline H& Y staging was significantly higher among those who died ) compared with those who survived ). Posada et al went further by splitting H& Y into early and later progression stages at baseline as a predictor for mortality and found that HRs increased by stage, from 1.5 for H& Y stages 1 and 2 to 2.3 for H& Y stages 35, both compared with patients with no PD and after controlling for comorbidities and demographic characteristics. Oosterveld et al stratified UPDRS total motor scores by greater than or equal to 30 compared with less than 30 and found an HR of 1.63 . Chiu et al compared the association of PSPRS scores on mortality and found increased HRs of 1.96 for 3548 on the PSPRS, 2.99 for 4862 and 8.55 for greater than 62 when compared with scores of 034.
Read Also: Parkinson’s Life Expectancy After Diagnosis