Parkinsons Symptoms Including Pain And Frequent Urination
Pain is a common cause of sleep disturbances in Parkinsons, says Horvat. A study published in June 2019 in the Journal of Pain Research found that about one-third of people with Parkinsons had clinically relevant sleep disturbances, and that central parkinsonian pain was the pain subtype that was most often associated with sleep issues.
Central pain can vary widely from person to person. It can feel like a constant burning or tingling that affects the whole body or it can be an intermittent sharp episode of pain, according to the Parkinsons Foundation.
You should definitely talk to your doctor if pain or Parkinsons symptoms are waking you up or keeping you up at night, to see what your treatment options may be, says Horvat.
Frequent urination can be a sign of several different things, and so its important to pay attention to any other symptoms you may also be having, she says.
Autonomic instability is often present in Parkinsons disease, which basically means the autonomic system is not firing regularly, as it should be, says Horvat. The autonomic system controls functions that keep you alive, including your heartbeat, breathing, and digestion.
This condition can lead to incontinence or urinary retention, she says. This is something to talk with your doctor about there are some medications that can be helpful.
Parkinsons Disease And Sleep
Reviewed by David Rye, MD, and Mark Mahowald, MD. Published by the National Sleep Foundation
This web article offers a detailed description of Parkinsons disease and the challenges it presents to restorative rest and recuperation. Some suggestions are included for improving sleep and the environment around sleeping.
Parkinson’s Disease And Sleep
Approximately two thirds of people with Parkinsons Disease experience one or more sleep-related symptoms, with insomnia being the most common. The neurodegenerative process in the brain, disturbances of the sleep-wake cycle, the effect of symptoms of Parkinson’s Disease on sleep, and having another sleep disorder such as restless legs syndrome, all contribute to sleep disturbances in people with Parkinson’s Disease.
Sleep disorders often cause major discomfort in Parkinsons Disease. Not only is the persons health and quality of life affected, but so are their family members, especially if they are also carers. And we have little evidence to suggest that current practices work for long-term treatment of sleep-related problems in people with Parkinsons Disease. Despite the recognised impact of sleep disturbance in Parkinsons Disease, there have been few studies in this area.
Read Also: What Age Can You Get Parkinson’s Disease
The Importance Of Sleep
Proper sleep is essential to everyones good health, regardless of whether you have Parkinsons disease. Getting enough quality sleep is important for the body. In fact, poor sleep has been linked to the development of chronic diseases, including heart disease, high blood pressure, diabetes, obesity, and depression.
Although the whole body benefits from proper rest, the brain may benefit the most. During sleep, the brain can be very active. Sleep is an essential part of maintaining proper brain function, including forming long-term memories. Lack of sufficient, good quality sleep can impair memory and thinking when awake.
Parkinsons disease can disrupt normal sleep, leading to additional problems, such as worsening levodopa-induced dyskinesia.
How Can You Improve Your Sleep
While Parkinsons can have a dramatic impact on sleep, several things can improve your ability to fall asleep and stay asleep. Good sleep hygiene habits that help promote a good nights sleep can improve sleep quality. Improved sleep quality may reduce levodopa-induced dyskinesia and improve your quality of life.
Read Also: Restless Legs And Parkinson’s
Rapid Eye Movement Sleep Behavior Disorder
Rapid eye movement sleep behavior disorder is a parasomnia that arises out of REM sleep and leads to a loss of paralysis of skeletal muscles where patients may exhibit dream enactment behavior . These behaviors during sleep may range from mild muscle twitches to vocalizations to violent and complex motor behaviors. This can lead to falling out of bed, self-injury, or injury to bed partners . In fact, bed partners may be the first to note these types of complex behaviors during sleep, as patients themselves are unaware of most episodes . The prevalence of RBD is estimated to be 0.51% of the general population, but up to 50% in the PD population . A diagnosis of probable RBD can be made clinically based on the presence of nocturnal behaviors associated with vivid or violent dreams . A definitive diagnosis requires polysomnography confirmation of abnormal tonic elevation and/or bursts of muscle tone measured by electromyography , termed loss of REM atonia . The underlying mechanism leading to loss of REM atonia in PD is likely mediated by accumulation of alpha-synuclein in pontine nuclei such as the sublaterodorsal nucleus and ventral medial medulla, which send inhibitory projections to the spinal motor neurons during REM sleep . For a number of patients with PD, the symptoms of RBD precede motor manifestations and a formal diagnosis of PD by a median time of 10 years, providing an opportunity for early diagnosis and neuroprotective interventions .
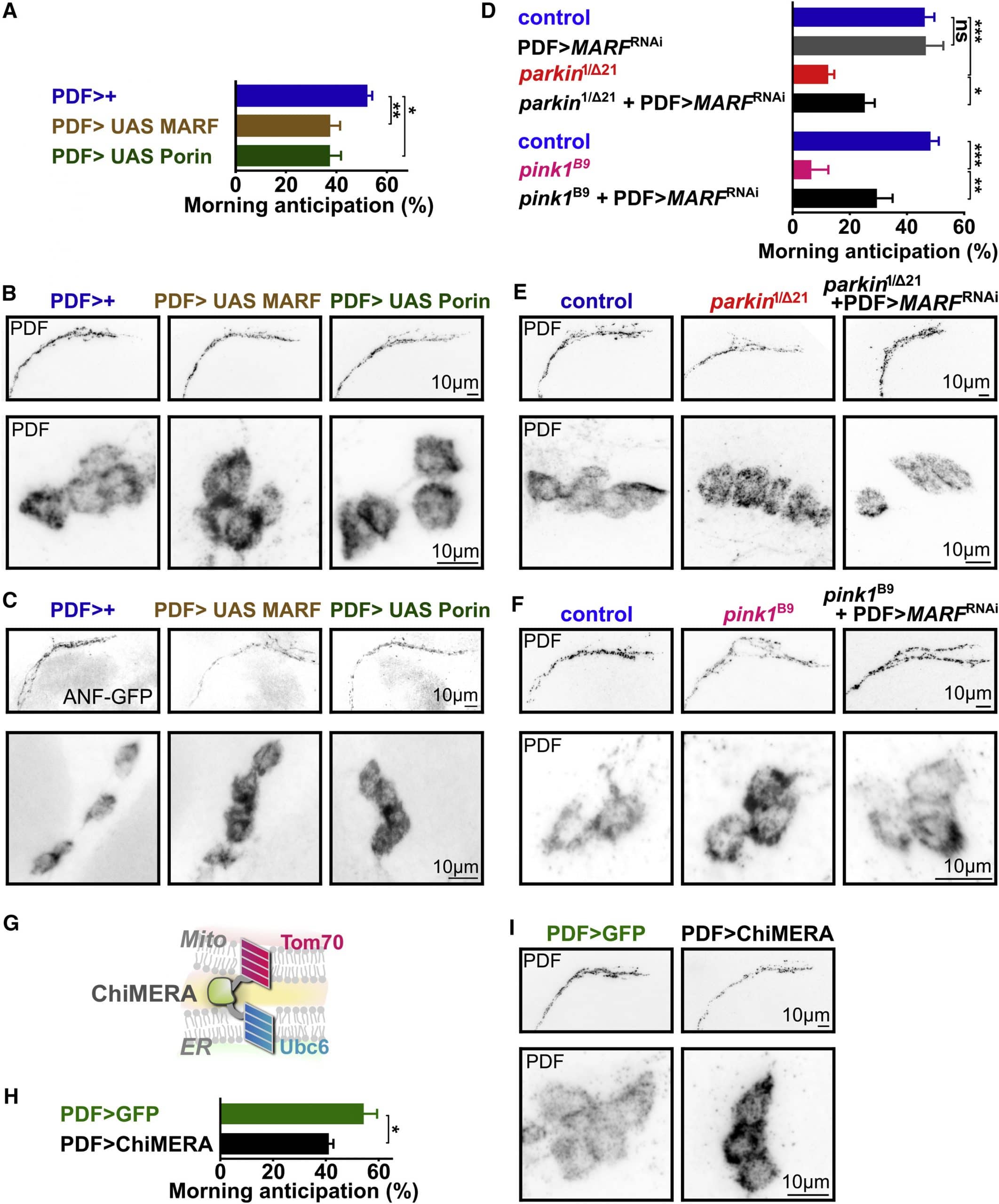
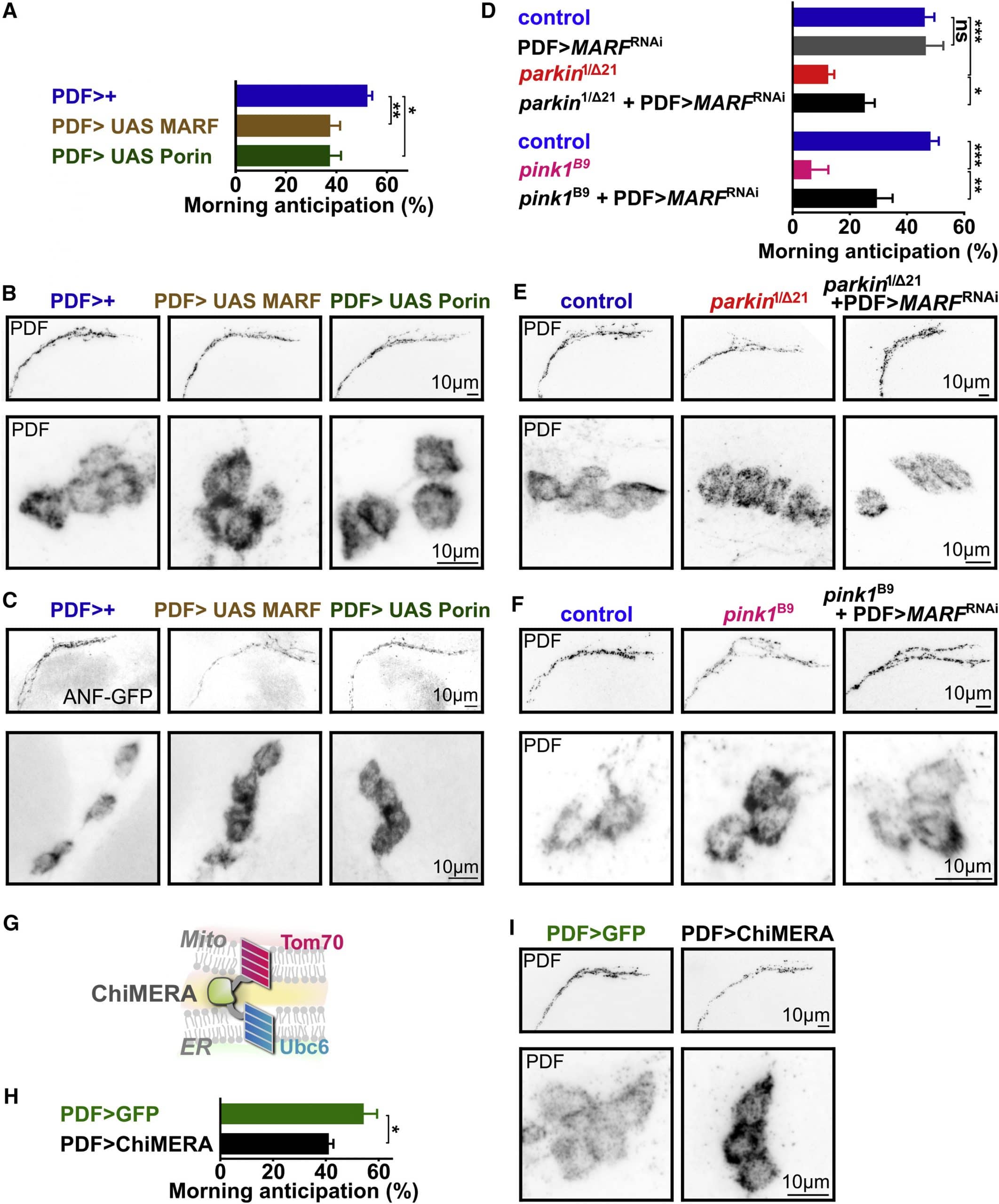
Fig. 2
Daytime Tips For Better Sleep
- Wake up at the same time every day, using an alarm if you have to.
- Get out of bed right after you wake up. Too much time spent in bed can lead to more waking at night.
- Eat regular, healthy meals, and eat at the same time every day. Three to four small meals are better than 1-2 large meals.
- Limit daytime napping to a 40-minute NASA nap . Too many or too-long naps can make sleep at night more difficult.
- Do not drink coffee, tea, sodas, or cocoa after noon. They contain caffeine and can interfere with normal sleep.
- Do not drink alcohol after dinner. It may help you fall asleep faster, but makes sleep shallower later in the night. Alcohol can also make snoring and sleep apnea worse.
- Use caution when taking headache and cold medicines. Some contain stimulants that can affect sleep.
- Stop smoking. Cigarette smoking stimulates the body and makes sleep difficult.
- Increase or start doing daily exercise. Regular exercise helps to deepen sleep. Avoid heavy exercise 2 hours before bedtime.
Also Check: Tardive Dyskinesia Parkinsons Disease
Don’t Miss: How Does A Doctor Diagnose Parkinson’s
Tips For Better Sleep
- Keep a regular sleep schedule go to bed at the same time and get up at the same time.
- Choose your bedtime based on when you want to get up. Plan to spend seven to eight hours a night in bed.
- Make a bedtime routine for example, snack, evening medication, tooth-brushing, using the restroom and follow it every evening.
- Spend time outdoors and exercise every day, in the morning if possible. Avoid exercise after 8:00 p.m.
- If you cant get outdoors, consider light therapy sitting or working near a light therapy box, available at drug stores and department stores.
- If you nap, try to do so at the same time every day, for no more than an hour, and not after 3:00 p.m.
- Sleep in a cool dark place and use the bed only for sleeping and sexual activity.
- Do not read, watch television, or use electronic devices in bed.
- If turning in bed is difficult: use a satin fitted sheet and pajamas use a light quilt instead of an easily tangled bedsheet.
- Minimize drinking liquids for three hours before bedtime to avoid frequent nighttime urination.
- Go to the bathroom immediately before retiring.
- Consider a soft, rather than bright, light to illuminate your path to the bathroom.
- Place a portable commode next to the bed to minimize effort, if needed.
Somnolence And Excessive Daytime Sleepiness
Somnolence and EDS occur commonly in PD. Etiologies of somnolence in PD include reversal of the sleepwake cycle, the disease process itself, disrupted sleep due to a variety of motor and nonmotor causes, and the use of dopamine agonists and other antiparkinsonian medications. Several studies have found that dopamine agonists are more likely to cause somnolence than levodopa. The soporific effects of the commonly used dopamine agonists appear to be similar as assessed by Epworth Sleepiness Scale scores.36
EDS occurs in PD patients, and is usually associated with dopamine agonist use. EDS may occur with use of other PD medications, including levodopa/carbidopa. However, EDS as measured by the ESS does not always correspond to shortened sleep latency as quantified by the Multiple Sleep Latency Test .10 In addition, nocturnal sleep disturbance as measured by polysomnogram may not account for the severity of daytime sleepiness in PD patients with EDS.10
Recommended Reading: How Does Parkinsons Disease Develop
Read Also: Support Groups For Parkinson’s
Getting Your Best Sleep With Parkinsons
This 1-hour webinar includes an interview of a person with Parkinsons disease, a movement disorders specialist, and a sleep sciences specialist. They discuss sleep disorders associated with Parkinsons disease, the difference between those that are a symptom the disease or a side-effect of medication, and how to treat them and live your best life with a sleep disorder.
How Are Sleep Problems Diagnosed In People With Parkinsons Disease
If youre having problems sleeping, sit down with your healthcare provider to discuss the issue in detail. Your provider will ask you questions to better understand your symptoms.
Be prepared to explain when sleep disruptions happen and how they affect your life. Keeping a sleep journal for a few weeks can help you remember the details.
If your provider suspects you may have a sleep disorder, they may recommend you have a sleep study. This overnight test uses electrodes attached to your skin to track how your body functions when youre sleeping.
Don’t Miss: Can You Diagnose Parkinson’s With An Mri
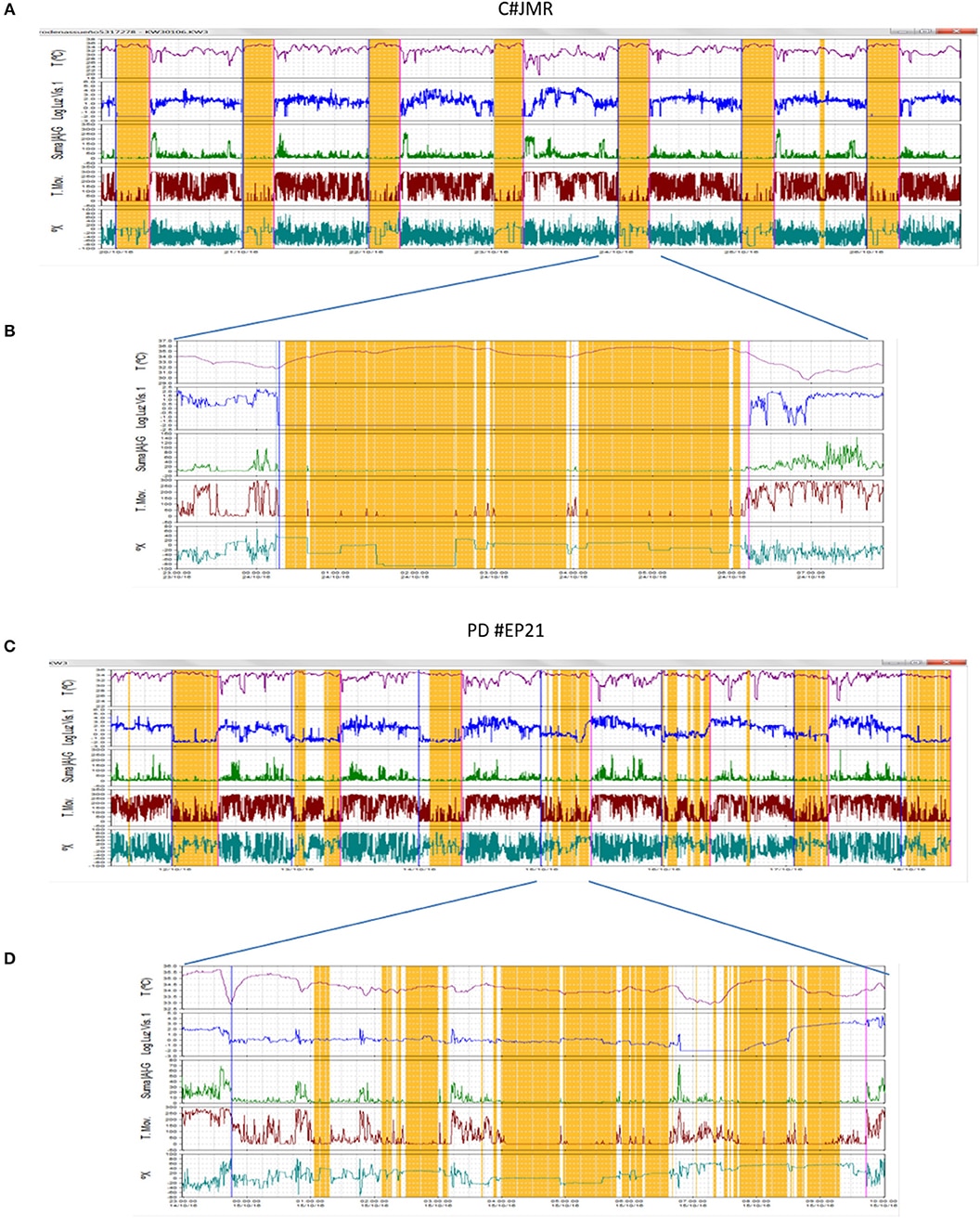
Impact Of Conventional Dbs On Sleep
Figure 3. Potential DBS targets for treatment of sleep dysfunction in PD. STN DBS may increase total sleep time and sleep efficiency, reduce wakefulness after sleep onset, and in some studies, increase REM duration. GPi DBS may improve sleep quality and daytime sleepiness. A single study in five PD patients with GPi DBS demonstrated a non-statistically significant increase sleep quality and efficiency, with decreased WASO, sleep onset latency, and REM latency. GPe DBS may improve insomnia and improve sleep efficiency. PPN DBS may improve sleep efficiency, REM duration, and daytime sleepiness, and decrease WASO. The ascending arousal system sends projections from the brainstem and posterior hypothalamus throughout the forebrain . Neurons of the laterodorsal tegmental nuclei and PPN send cholinergic fibers to many forebrain targets, including the thalamus, which then regulate cortical activity. Aminergic nuclei diffusely project throughout much of the forebrain, regulating the activity of cortical and hypothalamic targets directly. These include neurons of the tuberomammillary nucleus containing histamine, neurons of the dorsal raphe nuclei containing 5-HT, and neurons of the locus coeruleus containing noradrenaline. TMN, tuberomammillary nucleus DRN, dorsal raphe nucleus LC, locus coeruleus .
What Types Of Sleep Problems Do People With Parkinsons Disease Have
Parkinsons disease affects every person differently. It also impacts sleep in different ways. People with Parkinsons may have:
- Insomnia, finding it hard to fall asleep.
- Fragmented sleep, waking up many times over the night.
- Excessive daytime sleepiness, finding it hard to stay awake during the day.
- Very vivid dreams, which may cause hallucinations or confusion after waking up.
- Emotional dreams or nightmares, which may make you feel emotionally drained after waking up.
Also Check: How Do They Test For Parkinson’s
The Relationship Between Parkinsons Disease And Sleep
Its unclear whether poor sleep causes parkinsonian symptoms to worsen or whether worsening parkinsonian symptoms cause poor sleep. In many cases its likely a case of bidirectionality, with each one exacerbating the other.
Fragmented sleep and sleep deprivation appear to leave the brain more vulnerable to oxidative stress, which has been tied to the development of Parkinsons disease. Parkinsons disease is not usually diagnosed until individuals have developed sufficient motor symptoms, by which time a significant portion of brain cells have already been damaged. If poor sleep quality or having sleep disorders foreshadows the development of parkinsonian symptoms, these could be useful in early diagnosis of the disease.
More research is needed to clarify the multifaceted relationship between Parkinsons disease and sleep. A better understanding of this connection may offer medical experts the unique opportunity to screen at-risk individuals and perhaps delay the onset of the disease.
Poor Sleep Seems To Worsen Parkinsons Symptoms
Parkinsons disease and DLB are often considered to lie on the same continuum of disorders marked by toxic buildup of the alpha-synuclein protein in the brain. While they share common symptoms, including movement and cognitive impairments, cognitive problems tend to develop more quickly in DLB.
Both conditions are marked by sleep disruptions, including REM sleep behavior disorder .
Read Also: Zhittya Genesis Medicine Parkinson’s Disease
Sleep And Depression In Parkinsons Disease
Depression is seen in approximately 40% of PD patients in the course of their disease. Most persons with depression, including PD patients, also will experience problems with sleep. In depression, sleep does not refresh you like it used to, or you wake up too early in the morning. Dreams for depressed people are different, toothey are rare and often depict a single image.
Hallucinations And Rem Sleep Disorders In Parkinsons Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
You May Like: Cardinal Symptoms Of Parkinson’s Disease
Brain Changes Can Disrupt Sleep In Pd Patients
The exact cause of sleep disturbances in PD is not completely understood.
The pathophysiological changes begin in the back of the brain and spread to the front.
Hence, the brainstem gets involved earlier in the disease than other areas.
The brainstem has the reticular activating system which controls the sleep-wake cycle.
The RAS also communicates with other areas of the brain using many different neurotransmitters.
Brainstem involvement can change the neurotransmitter balance and modulate the activity of other areas.
This imbalance may manifest as sleep disturbances.
The use of dopamine agonists can produce sleep disturbances by altering neurotransmitter function.
You May Like: What Is Parkinsons Disease And What Causes It
Insomnia And Parkinsons Disease
Parkinsons disease comes with its fair share of challenges. Among the most frustrating symptoms of Parkinsons is insomnia, or difficulty sleeping. Research has found that the majority of people with PD experience trouble sleeping, and more than 3,000 members of MyParkinsonsTeam report difficulty sleeping as a symptom. Lack of regular sleep can have tremendous impacts on a persons quality of life. In fact, dealing with a sleep deficit can cause anyone to experience problems with memory and thinking.
Good, restful sleep is vital for people with Parkinsons, but it isnt always easy to get quality sleep. Luckily, there are some ways you can work toward combating insomnia with Parkinsons.
Dont Miss: Nuevos Tratamientos Para El Mal De Parkinson
Read Also: Are Shaky Hands A Sign Of Parkinson’s
Valerian Root And Other Herbal Supplements
A quick tour in the supplement aisle at a grocery store can give you a dizzying array of herbal supplements advertised to improve sleep. Valerian root is one of the most widely recognized. Although it has the potential for significantly enhancing sleep, people often experience residual sleepiness the next day.
Typically, you will find products combining several different compounds. The ability of these different compounds to induce sleep has not necessarily been studied, particularly in people living with Parkinsons. If youre interested in trying one of these products, consult your doctor with a list of the ingredients before attempting to incorporate them into your sleep routine.
Why Is It So Hard To Sleep Now That I Have Parkinsons
Parkinsons can impact sleep in a number of ways, ranging from trouble falling or staying asleep at night to excessive sleepiness during the day. A good sleep boosts everything from your mood to your ability to think and process to your physical movement. Understanding sleep problems and Parkinsons is often the first step you can take to enhance your sleep.
In this post, we help you learn more about sleep problems in Parkinsons and how you can improve your quality of sleep.
Parkinsons can affect sleep in many different ways, including trouble falling or staying asleep, vivid dreams, waking up frequently during the night and excessive sleepiness during the day. Like other non-motor symptoms, sleep problems can appear before the more recognized motor symptoms, like tremor or stiffness.
People with Parkinsons typically experience some combination of insomnia and sleep fragmentation . Studies have shown people with Parkinsons have different sleep patterns and that their deepest periods of sleep during the night are shorter and interrupted more often than people without Parkinsons. Often this is made worse by medications that may wear off during the night, causing painful stiffness, difficulty moving in bed or other symptoms to return and disrupt sleep.
Recommended Reading: Can Parkinson’s Affect The Eyes
Medication Changes For Dyskinesia
Dyskinesia can be improved in some cases by carefully adjusting ones levodopa dosage. can improve dyskinesia, but doctors must take care to find a dosage that adequately controls symptoms while limiting side effects.
Changing the timing of levodopa administration or using an extended-release formulation may also improve dyskinesia. Amantadine can be added to levodopa to help control dyskinesia.
Additionally, it may be necessary to discontinue certain Parkinsons drugs that can worsen dyskinesia, including monoamine oxidase B inhibitors and catechol-O-methyltransferase inhibitors.
If drug treatments are not helpful, your doctor may consider recommending more invasive options, like deep brain stimulation. These approaches can improve dyskinesia and other symptoms of Parkinsons as well.
