Ethnic Variation In Cognition In Pd
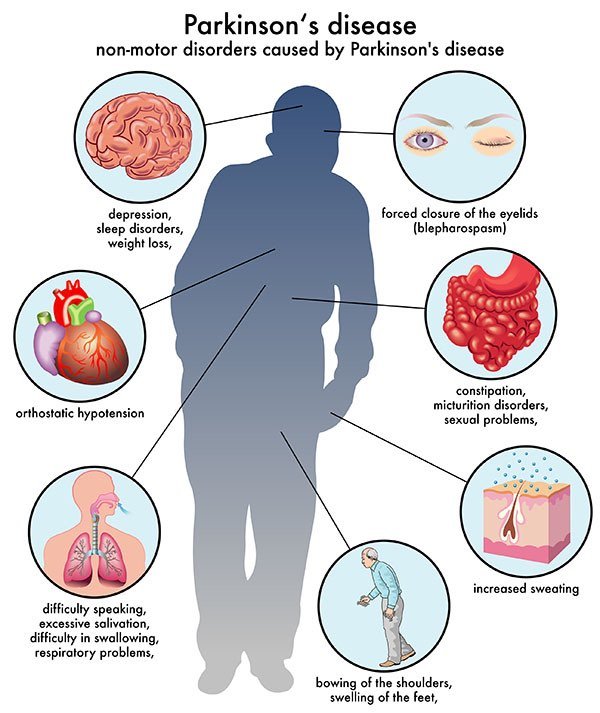
Cognitive impairment is one of the most frequent and disabling non-motor symptoms of PD . The typical cognitive domains affected by PD dementia are visuospatial, executive and attention, but there can be global deficits, particularly in advanced disease. Cognitive dysfunction frequently occurs in combination with neuropsychiatric features including depression, anxiety, hallucinations and apathy, which are major determinants of morbidity . The presence of cognitive impairment with a diagnosis of PD is established as a significant indicator of increased mortality .
Similar findings have been observed for Hispanic patients in some settings . Hispanic patients may have a more severe form of PD dementia and/or an increased severity of behavioural and psychological symptoms in dementia . The evidence regarding Asian PD patients and cognitive dysfunction is more conflicting. Willis et al. found in their 6-year retrospective cohort study that Asian patients had the lowest odds of being diagnosed with dementia during the study period . But Asian PD patients report higher levels of subjective cognitive impairment than White patients . It remains to be determined whether Asian patients suffer from different rates of cognitive dysfunction compared to other ethnicities. This is particularly true for South Asian populations that have largely been unstudied.
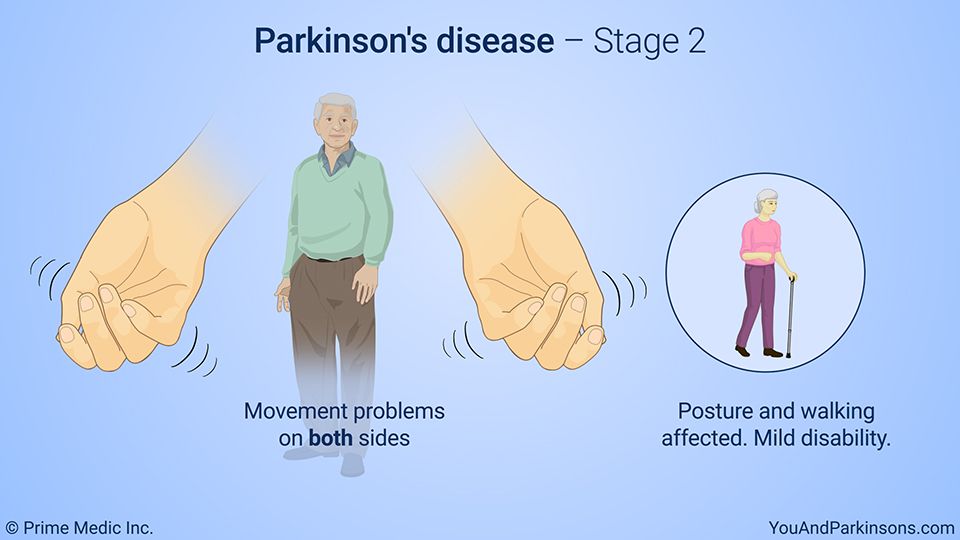
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinsons disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinsons.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinsons disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinsons disease has a tremor, nor is a tremor proof of Parkinsons. If you suspect Parkinsons, see a neurologist or movement disorders specialist.
Tremors
Rigidity
Bradykinesia
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
Diagnosis Of Parkinsons Disease
A number of disorders can cause symptoms similar to those of Parkinson’s disease. People with Parkinson’s-like symptoms that result from other causes are sometimes said to have parkinsonism. While these disorders initially may be misdiagnosed as Parkinson’s, certain medical tests, as well as response to drug treatment, may help to distinguish them from Parkinson’s. Since many other diseases have similar features but require different treatments, it is important to make an exact diagnosis as soon as possible.
There are currently no blood or laboratory tests to diagnose nongenetic cases of Parkinson’s disease. Diagnosis is based on a person’s medical history and a neurological examination. Improvement after initiating medication is another important hallmark of Parkinson’s disease.
You May Like: Effects Of Sugar On Parkinson’s Disease
Other Studies Of Interest
Three high-quality papers were found but not included in the meta-analysis as they did not report age- and gender-specific incidence rates or proportions. These studies provided information on Asian and Eastern European populations that were not well represented in the meta-analysis.
Das et al. was the only study that examined PD in a south Asian Indian population, reporting average annual incidence rates for males and females in different age categories. AAIRs peaked earlier for males, than females. Male AAIRs peaked at 60-69 years female AAIRs continued to rise in 70-79 years before dropping off in the 80+ age group. Hristova et al. and Kyrozis et al. both provided incidence rates not stratified by gender and age and therefore could not be included in the meta-analysis. Both represented unique European populations and found peak incidence between 70 and 80 years.
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
Read Also: Is Parkinson’s Disease Fatal
Ethnic Variation In The Manifestation Of Parkinsons Disease: A Narrative Review
Article type: Review Article
Authors: Ben-Joseph, Aarona | a | Lees, Andrew J.b | Noyce, Alastair J.a b *
Affiliations: Preventive Neurology Unit, Wolfson Institute of Preventive Medicine, Queen Mary University of London, London, UK | Reta Lila Weston Institute of Neurological Studies and Department of Clinical and Movement Neurosciences, University College London, London, UK
Correspondence: Correspondence to: Dr. Alastair Noyce, MRCP, PhD, Preventive Neurology Unit, Wolfson Institute of Preventive Medicine, Barts and the London School of Medicine and Dentistry, Queen Mary University of London, London, EC1M 6BQ, UK. Tel.: +44 207 882 3527 E-mail: .
Keywords: Parkinsons disease, ethnic groups, epidemiology, tremor, dementia, atypical parkinsonism
DOI: 10.3233/JPD-191763
Journal: Journal of Parkinson’s Disease, vol. 10, no. 1, pp. 31-45, 2020
Abstract
Ethnic Variation In Non
In the past two decades, there has been significant progress in the understanding of the non-motor manifestations of PD . However, there remains relatively few studies that compare non-motor symptom prevalence in ethnically diverse samples. The Non-Motor Symptom Questionnaire was designed and validated in 2006 and has been used in different populations to enable comparison . All patients, regardless of ethnicity, appear to suffer from a high burden of non-motor symptoms. It is notable in Table 2 that the prevalence of gastrointestinal non-motor symptoms appear to be highest in the East Asian studies . The prevalence of depression was above 60% in the Chinese, Korean, Mexican and Peruvian studies , but in the studies from the UK and the USA the rate was less than 40% . A study comparing mood and anxiety symptoms in a multi-ethnic sample found no clear differences .
Table 2
Non-motor symptoms questionnaire results by country
| Study | |
| 14 | 8 |
N& V, nausea and vomiting OH, orthostatic hypotension EDS, excessive daytime sleepiness RBD, REM sleep behaviour disorder. Any data that was not available is replaced with a dash.
Excessive daytime sleepiness may be more common in PD patients from Europe and North America. Studies in Asian countries suggest a prevalence in the range of 1532% of patients. Whereas studies in North America and Europe suggest a prevalence of EDS between 4157% .
Table 3
Impulse control behaviours by country
| Study | |
Don’t Miss: Can Parkinson’s Run In The Family
Whats Different About Young
The age of diagnosis matters for a variety of reasons, from probable causes of early cases to symptoms and treatment:
- Genetics. As with any case of Parkinsons disease, the exact cause is usually unknown. That said, The young-onset cases of Parkinsons disease are, on average, a bit more likely to be familial or genetic, says Gregory Pontone, M.D., director of the Johns Hopkins Movement Disorders Psychiatry Clinic.
- Symptoms. In many patients with YOPD, dystonia is an early symptom. People with YOPD also report more dyskinesia . They also tend to exhibit cognitive problems, such as dementia and memory issues, less frequently.
- Progression. Patients with young-onset Parkinsons appear to have a slower progression of the disease over time, says Pontone. They tend to have a milder course, staying functional and cognitively intact for much longer.
- Treatment. Most patients with Parkinsons take the medication levodopa. However, other drugs, such as MAO-B inhibitors, anticholinergics, amantadine, and dopamine receptor agonists, may be used before levodopa.
Parkinsons Disease Is A Global Pandemic
PD is an age-related disorder symptoms typically begin to first appear at varying stages in patients in their mid-60s.
PD had been a rare disorder, however, demography and the by-products of industrialisation are now contributing to an impending PD pandemic. It is currently understood to affect 12% of individuals aged 65 years and older worldwide.
The increase in prevalent cases of PD worldwide is a major reason for researchers to increase efforts in understanding the disease.
Also Check: Life Expectancy Of Someone With Parkinson’s
This Chemical Is Banned In Europe But Common In The Us
Doctors have a difficult time tracing cases of Parkinsons Disease back to their root cause, in no small part because the degenerative neurological condition can be triggered by exposure to chemicals years before any symptoms emerge.
But case numbers have increased drastically in the US over the course of the last decade, University of Rochester Medical Center neurologist Ray Dorsey warned The Guardian, and a carcinogen called TCE thats commonly used in household and industrial cleaning products might be to blame.
Scientists first linked TCE to Parkinsons back in 2012, but the compound is often overlooked in studies on the disease because whole decades can pass in between exposure and the onset of symptoms in some cases, according to The Guardian. In the meantime, other causes including gut hormones have been linked to the disease, but an increasing body of evidence continues to point toward chemical exposure. TCE is banned in Europe, but there are no federal restrictions on it in the US, and only Minnesota and New York have banned the compound.
Numerous studies have linked well water to Parkinsons disease, and its not just TCE in those cases, it can be pesticides like paraquat, too, Dorsey told The Guardian.
Care about supporting clean energy adoption? Find out how much money you could save by switching to solar power at UnderstandSolar.com. By signing up through this link, Futurism.com may receive a small commission.
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Environmental And Genetic Factors
Scientists are also working to learn more about environmental factors and genetic factors that might contribute to the risk of developing Parkinsons. One recent genetic research breakthrough is the development of a DNA chip called NeuroX, which could potentially determine a persons risk, but more research is needed.
Parkinsons disease is the result of complicated combination of interconnected events, as described it. Since aging is the most common risk factor, future treatments may need to take degeneration of certain neurons into account.
Sidebar: Advances In Circuitry Research
The brain contains numerous connections among neurons known as neural circuits.
Research on such connections and networks within the brain have advanced rapidly in the past few years. A wide spectrum of tools and techniques can now map connections between neural circuits. Using animal models, scientists have shown how circuits in the brain can be turned on and off. For example, researchers can see correlations between the firing patterns of neurons in a zebrafishs brain and precise behavioral responses such as seeking and capturing food.
Potential opportunities to influence the brains circuitry are starting to emerge. Optogenetics is an experimental technique that involves the delivery of light-sensitive proteins to specific populations of brain cells. Once in place, these light-sensitive proteins can be inhibited or stimulated by exposure to light delivered via fiber optics. Optogenetics has never been used in people, however the success of the approach in animal models demonstrates a proof of principal: A neural network can be precisely targeted.
Thanks in part to the BRAIN Initiative, research on neural circuitry is gaining momentum. The Brain Research through Advancing Innovative Neurotechnologies Initiative is accelerating the development and application of new technologies that enable researchers to produce dynamic pictures of the brain that show how individual brain cells and complex neural circuits interact at the speed of thought.
NIH Publication No. 15-5595
Read Also: Stages Of Parkinson’s Disease Life Expectancy
Exploring The Clinical Burden Of Off Periods In Parkinson Disease
Supplements and Featured Publications
ABSTRACT
Parkinson disease, the second-most-common neurodegenerative disorder, affects approximately 1 million individuals in the United States, and this number is projected to increase to 1.2 million by 2030. Characterized pathologically by degeneration of dopaminergic neurons, with widespread pathology in nondopaminergic systems, Parkinson disease leads to an array of motor and nonmotor symptoms that can significantly impact an affected individuals quality of life. Treatments for Parkinson disease typically focus on controlling the motor symptoms of the disease, including treating OFF periods when motor symptoms return. OFF periods can occur for many individuals with Parkinson disease, especially as the disease progresses, and can pose a substantial burden to those with the disease and their caregivers. Available treatments for OFF periods may help alleviate this burden.
Am J Manag Care. 2020 26:S255-S264.
For author information and disclosures, see end of text.
Introduction
Diagnosis of PD usually occurs after age 50 years, and incidence rises with increasing age.1 In most populations, incidence of PD is twice as common in men as in women.1 In a population-based study conducted in Olmsted County, Minnesota, incidence was observed to increase over a 30-year period, particularly in men 70 years or older .4
Etiology
Diagnosis of Parkinson Disease
Symptoms of Parkinson Disease
Nonmotor Symptoms
Tips For Daily Living
If you are already living with Parkinsons disease, here are some tips to manage it:
- Exercise your brain. Read, work on crossword puzzle, do Sudoku, or engage in other activities that use your brain.
- Get moving. If you feel comfortable walking, swimming, or riding an exercise bike, go for itand try to do it on a regular basis.
- Try tai chi. We think of tai chi as a mind-body exercise, and it is, but it also has roots as a martial art in China. A 2012 study found that practicing tai chi helped people with moderate Parkinsons disease maintain stability and balance. And a 2014 study found that tai chi can help people reduce their risk of falling. It incorporates a flowing series of coordinated movements to help you maintain flexibility, strength and balance, and it can be easily adapted to meet your abilities.
- Practice yoga. You dont have to perform headstands or other physically challenging poses to get significant benefits from practicing yoga. You can improve your balance, mobility, flexibility, and strength with a form thats adapted for you.
- Find a support group. Whether you prefer an online support group or a group that meets in person, a support group can be an invaluable resource for helping you live with Parkinsons disease.
You May Like: Is Parkinson’s Disease Fatal
How Many Canadians Live With Parkinsonism And How Many Are Newly Diagnosed Each Year
Based on the latest estimates available , in 20132014, approximately 84,000 Canadians aged 40 years and older were living with diagnosed parkinsonism and 10,000 Canadians were newly diagnosed with this condition . The age-standardized prevalence was 1.5Footnote i times higher among males than among females , and similarly the age-standardized incidence was 1.7Footnote i times higher among males than females . The epidemiological burden of parkinsonism increases with age. In 20132014, when comparing estimates among Canadians aged 85 years and older vs. those aged 40-44 years, the prevalence of the condition was 169Footnote i times higher in the older age group , while the incidence was 48Footnote i times higher in the older age group .
Figure 1: Prevalence of diagnosed parkinsonism, including Parkinsons disease, by sex and age group, Canada, 20132014
| Age group |
|---|
| 44.7 | 55.1 |
Note: The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20. Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, July 2017.
Common Treatments For Parkinsons Disease
Parkinsons disease is a long-term degenerative disease which affects the central nervous system. To date, there is no cure for the condition, but there are medications and therapies available to address some of the symptoms and improve quality of life for patients.
Here are eight of the main drugs and therapies used in the treatment of Parkinsons disease according to the Mayo Clinic:
1. Carbidopa-levodopa
Levodopa is a naturally occurring chemical which can enter the brain and be converted to dopamine. When combined with carbidopa, the levodopa is prevented from converting into dopamine before it enters the brain. The is one of the most effective treatments for Parkinsons although, after long-term use, the effects start to fluctuate.
Some people may experience side effects such as nausea, feeling lightheaded, and making sudden involuntary movements.
2. Carbidopa-levodopa infusion
In 2015, the FDA approved Duopa, which is a combination of carbidopa and levodopa in a gel form which is administered via a feeding tube into the small intestine. Duopa is generally given to patients with advanced Parkinsons disease whose response to carbidopa-levodopa fluctuates. The drug is infused continuously so the levels remain constant.
The risks associated with Duopa are infections at the site of the feeding tube and the tube falling out.
MORE: Read about the five stages of Parkinsons disease
3. Dopamine agonists
4. MAO-B inhibitors
5. Catechol-O-methyltransferase inhibitors
Recommended Reading: Is Parkinson’s Terminal
Causes Of Parkinson’s Disease
Parkinson’s disease is caused by a loss of nerve cells in part of the brain called the substantia nigra. This leads to a reduction in a chemical called dopamine in the brain.
Dopamine plays a vital role in regulating the movement of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinson’s disease.
Exactly what causes the loss of nerve cells is unclear. Most experts think that a combination of genetic and environmental factors is responsible.
