What Is Congestive Heart Failure
Congestive heart failure is a condition in which the heart becomes enlarged, often due to high blood pressure or narrowing of the coronary arteries.
It leads to an increase in blood volume being pumped out of the left ventricle with each contraction. This leads to fluids backing up in the lungs and body, leading to various symptoms. These include breathlessness, weakness, fatigue and coughing. The most serious complication of congestive heart failure is fluid accumulating around the lungs, known as pulmonary oedema or water on the lung.
1. Congestive heart failure is the most common cardiovascular condition in people over 65 years of age.
2. Heart failure has two major causes: cardiovascular disease or acute myocardial infarction.
3. About one third of heart failure cases are due to dilated cardiomyopathy, in which the heart muscle is damaged by abnormal heart muscle cells .
4. About one third of cases are due to left ventricular hypertrophy .
5. About 15% of cases in males and about 75% in females are idiopathic .
The term congestive heart failure refers to a condition in which the heart becomes enlarged, often due to high blood pressure or narrowing of the coronary arteries.
If untreated, congestive heart failure may progress to decreased exercise tolerance and acute deterioration.
The link between coffee and congestive heart failure
The link between coffee and congestive heart failure
Dont Miss: What Is Drug Induced Parkinsons Disease
Limitations And Future Directions
All PD patients in our study were maintained on regular doses of dopaminergic medication. Furthermore, the MDD group received no medications. There was no way to examine whether the PD-associated deficit predated the MDD-associated deficit, or the opposite, in the PD-MDD group. Future studies ought to focus on the effects of dopaminergic medications on cognitive function in PD-MDD. Furthermore, MDD should be studied longitudinally in medication-naïve patients with PD to investigate the chronological order of cognitive deficits associated with PD-MDD.
Types Of Anxiety Disorders Found In Parkinson’s Disease
Generalised anxiety disorder, panic disorder, social phobia, phobic disorder, agoraphobia, obsessive-compulsive disorder, and anxiety disorder not otherwise specified have all been identified in patients with Parkinson’s disease . The diagnoses in the patients with Parkinson’s disease appear to be clustered in the panic disorder, phobic disorder, and generalised anxiety disorder areas.
Box 1: Anxiety disorders found in Parkinson’s disease
-
Generalised anxiety disorder
You May Like: Can Parkinsons Be Diagnosed With An Mri
Anxiety And Antiparkinsonian Medications
There is no consensus on whether antiparkinsonian medications are responsible for symptoms of anxiety in Parkinson’s disease.
Stein et al found that the levodopa dose was similar in anxious and non-anxious patients. Hendersonet al noted that 44% of patients with Parkinson’s disease noticed anxiety symptoms before starting levodopa. Menza et al found that the levodopa dose did not significantly correlate with anxiety levels: they suggested that anxiety in patients with Parkinson’s disease is unlikely to be a side effect of levodopa treatment. In contrast, Vasquez et al found that panic attacks were related to levodopa therapy but not to other agonist drugs.
Lang reported anxiety in five of 26 patients when pergolide was added to their treatment regimen. Menza et al found no differences in measures of anxiety in patients receiving or not receiving pergolide. Menzaet al found no differences in measures of anxiety in patients receiving or not receiving selegeline.
The temporal relationship between panic attacks and off periods have led some authors to suggest that panic attacks may be related to falling brain levodopa levels. Anxiety fluctuations may be an important component of levodopa induced fluctuations. In a double blind placebo controlled trial, Maricle et al found that anxiety levels fell and motor performance improved during a levodopa infusion.
Depression Reduces Accuracy While Parkinsonism Slows Response Time For Processing Positive Feedback In Patients With Parkinsons Disease With Comorbid Major Depressive Disorder Tested On A Probabilistic Category
- 1Palestinian Neuroscience Initiative, Al-Quds University, Abu Dis, Palestine
- 2Center for Molecular and Behavioral Neuroscience, Rutgers University, Newark, NJ, United States
- 3School of Social Sciences and Psychology, Marcs Institute for Brain and Behavior, Western Sydney University, Sydney, NSW, Australia
- 4Department of Veterans Affairs, VA New Jersey Health Care System, East Orange, NJ, United States
- 5Department of Physiology, Pharmacology and Neuroscience, New Jersey Medical School, Rutgers University, Newark, NJ, United States
You May Like: What Vitamins Should Not Be Taken With Parkinson’s
Role Of Imaging In Diagnosis
For a patient presenting with symptoms of typical idiopathic Parkinsons disease and no other abnormal exam findings, imaging is usually not necessary.
Dr. Hung notes that he will typically order an MRI in the following situations:
- Atypical symptoms some atypical parkinsonian syndromes can have particular MRI correlates that mary be useful
- Lower-body predominant parkinsonism For patients with significant lower-body parkinsonism without significant tremor or upper-body bradykinesia, an MRI is important to obtain to rule out the following causes of lower-body parkinsonism : 1) Vascular disease significant frontal white matter disease can cause symptoms of lower-body parkinsonism, and 2) Normal pressure hydrocephalus can cause parkinsonian symptoms involving the gait.
Features Of Parkinsons Disease Psychosis
PDP typically arises later in the course of the disease, approximately 10 years after initial diagnosis of PD. Symptoms typically arise in the context of retained insight and clear sensorium . Over time, symptoms such as visual hallucinations or delusions tend to recur and progress and insight is lost. Prominent hallucinations early in the course of the disease may suggest Lewy body dementia, Alzheimerâs disease, or a preexisting psychiatric disorder .
Recommended Reading: Early Parkinsonâs Symptoms Mayo Clinic
Recommended Reading: Japan Parkinson’s Stem Cell Breakthrough
Depression In Genetic Pd
Whether genetic forms of PD predispose to depression remains an open question, although monogenic forms of PD resembling idiopathic PD with Lewy-body synucleinopathy represent critical etiopathogenic models.
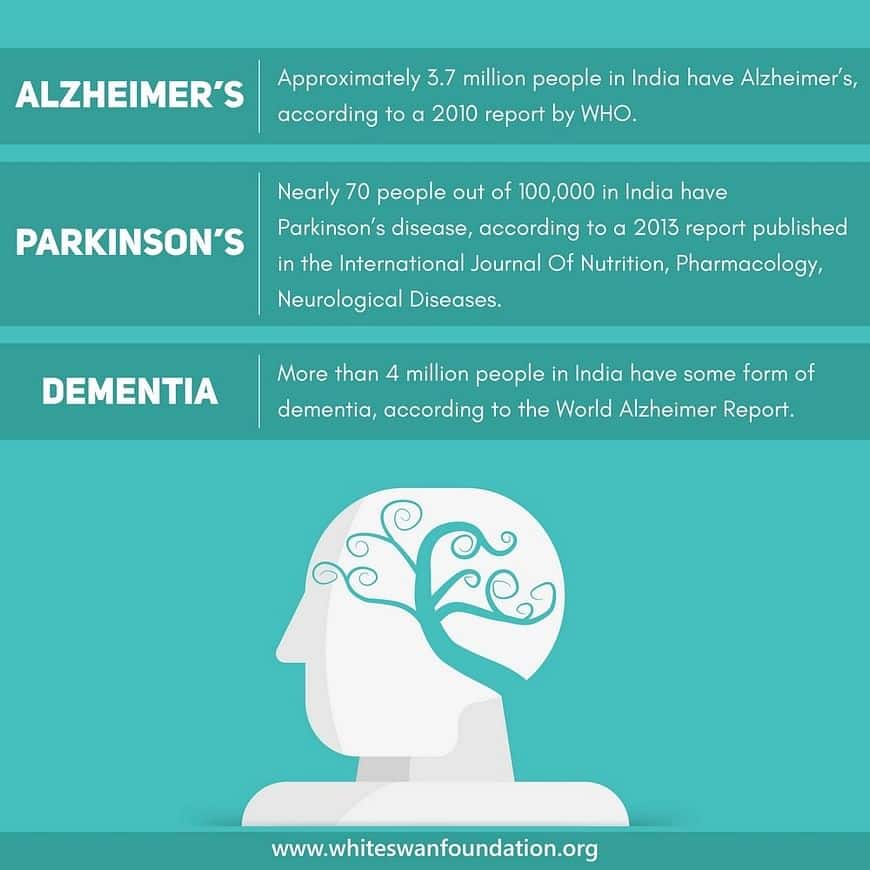
Depression is frequent in patients with genetic PD , although depression was not related to mutations of parkin, leucine-rich repeat kinase 2 and apolipoprotein E status in a large study gathering 632 families . In addition, a recent study showed that depression severity was similar to healthy controls in both LRRK2 and glucocerebrosidase mutation carriers at risk of PD as well as RBD and impulse control disorders . Nevertheless, prevalence of depression is close to 30% in LRRK2 patients with manifest PD and may predate motor symptoms, similar to patients with idiopathic PD , whereas prevalence of dementia might be lower . Moreover, depression severity increased over 2 years in heterozygous carriers of GBA mutations, who are at high risk of PD, also associated with greater olfactory and cognitive impairment , and depending on the alleles .
Overall, these robust statistical associations and temporal precedence suggest that depression and PD may share common pathophysiological mechanisms , and that association with specific comorbidities and risks factors may reflect different pathological routes .
Table 1 Summary of epidemiological findings for depression in patients with Parkinsons disease
Treatment Of Advanced Motor Symptoms
In more advanced Parkinsons disease, patients will often experience a shorter window of time in which levodopa / carbidopa is effective, and tend to develop on / off fluctuations in which they experience wearing off of the medication towards the end of the dose . This is because levodopa has a short half life in the blood while in earlier stages of Parkinsons disease the body can accommodate this, in later stages the accommodation is less robust, and wearing off will occur. Additionally, when patients do take enough medication to achieve an on state, they may exhibit too much movement, known as levodopa-induced dyskinesias , which can include writhing, swaying, and bobbing. Thus, the challenge in managing motor symptoms in advanced Parkinsons disease is trying to strike a balance between wearing off and levodopa-induced dyskinesias When patients reach this point, a movement disorder specialist should be involved in management.
In thinking about management of advanced motor symptoms, Dr. Hung notes that thinking about pharmacokinetics is key: essentially, considering how to stretch out the duration of action of levodopa to prevent so many highs and lows. There are several strategies in treating motor symptoms in advanced Parkinsons disease:
You May Like: Patrick Losasso Parkinson’s Exercises
Why Check Heart Rate Variability
- It can identify ANS imbalances. When your system is in fight-or-flight mode, the difference between heartbeats is low as compared to when you are in a relaxed mode where the difference between the heartbeats is high.
- HRV can detect stress levels. People with low HRV can easily experience acute stress while people with high HRV rarely experience stress and their cardiovascular system is in great shape. Checking your HRV can help you understand how to respond to stress in a healthier way.
- May increase awareness of your lifestyle habits. Checking your HRV is one way you can know if your lifestyle habits are healthy or unhealthy for your heart and a great tool to motivate behavioral change.
- It can detect your reaction to the environment, and emotions. Your nervous system can tell you how you are reacting to your environment, feelings, and emotions when you track your HRV.
- Can increase your self-awareness. HRV measurements can help increase your awareness of how you live and think, and how your behavior affects your nervous system and bodily functions.
You May Like: Parkinsons Disease Urinary Incontinence
Phenomenology And Diagnostic Issues
There is no general consensus about the most valid methods to assess and diagnose depression in PD. One of the most important nosological limitations is the overlap between symptoms of depression and symptoms of PD . A workgroup established by the National Institutes of Neurological Disorders and Stroke, and the National Institutes of Mental Health proposed provisional criteria for depression in PD . The workgroup stressed the need to validate the DSM-IV categories of major depression, minor depression and dysthymia, as well as the concept of subsyndromal depression in patients with PD. They recommended the use of the inclusive approach to symptom assessment , to distinguish loss of interest/anhedonia from apathy, to consider whether putative depressive symptoms may be the expression of motor fluctuations, to assess depression at consistent times and during the on and off states, and to obtain additional information about mood changes from a next of kin or caregiver. Other investigators reported a relatively low frequency of guilt, self-blame and worthlessness in depressed patients with PD .
Read Also: Does Parkinson’s Affect Memory
Is It Bradycardia Or Something Else Causing Symptoms
- Brian OlshanskyCorrespondenceAddress reprint requests and correspondence: Dr Brian Olshansky, University of Iowa Hospitals, 200 Hawkins Drive, 4426a JCP, Iowa City, IA 52242.Cardiovascular Division, University of Iowa Hospitals, Iowa City, IowaCardiovascular Division, Mercy Medical Center North Iowa, Mason City, Iowa
- Cardiovascular Division, Hospital of the Good Samaritan, Los Angeles, CaliforniaCardiovascular Division, Cedars Sinai Medical Center, Los Angeles, California
Key Teaching Points
The Hallucinations Of Parkinsons Disease
People living with Parkinsons disease frequently experience visual hallucinations. These symptoms can occur in between 8% and 20% of patients during their illness. It is possible to have hallucinations that are visual, such as seeing animals or people, or that are auditory, such as hearing voices. While hallucinations are uncommon in the majority of patients, they can be persistent in others. Parkinsons disease patients may also exhibit increased hallucinations as the disease progresses as a marker of how severe it is. Although hallucinations do not always indicate a more serious condition, they can be a source of distress for those who have them. hallucinations can be caused by other non-motor symptoms like incontinence or insomnia. Although hallucinations are not the end of Parkinsons disease, they are one of the first symptoms that patients will experience. Affirming that hallucinations are a significant challenge for those with the disorder.
Donât Miss: Stage 4 Parkinsonâs Disease
Read Also: Life Expectancy Parkinson’s Dementia
Association Between Depression And Motor Symptoms
Greater motor and global impairment, closely related to worse quality of life, is a constant finding in depressed patients , although the impact of depression on motor impairment is modest . In addition, depression in early PD is regarded as a risk factor for worse motor and global prognosis . This is also the case in patients with advanced PD and persistent depression . This is consistent with previous studies confirming the association between depression and PD severity scores, motor complications, duration of treatment) such as the DEPAR and DoPaMiP surveys in older and more advanced patients, including those with mild cognitive impairment . Furthermore, worse motor prognosis was found in mid-stage patients with greater depression, apathy and anxiety as well as greater cognitive impairment . Importantly, comorbid depression over time is not related to worse motor prognosis in prospective studies but may accelerate the initiation of dopaminergic replacement therapy in early PD .
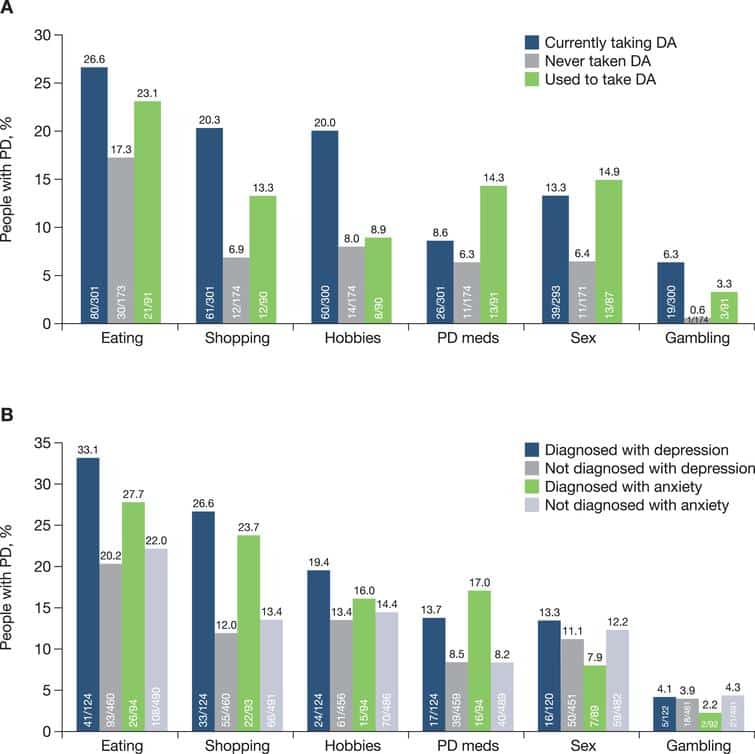
Higher depression scores were found in patients with motor fluctuations and/or dyskinesia , also in comparison with drug-naïve patients . Greater dyskinesia, levodopa equivalent dose and impulse control disorders were also associated with depression . In addition, greater severity of depression was the strongest predictor of impulse control disorders of all types, independently of treatment with dopamine agonists .
Mood Changes In Parkinson’s
When faced with a diagnosis of Parkinson’s disease , it is understandable to feel depressed or anxious. But mood disorders such as depression and anxiety are clinical symptoms of Parkinson’s, just as are slowness of movement and tremor. In fact, up to half of all people with Parkinson’s may suffer from depression and/or anxiety at some point during the course of their disease. Like all symptoms of PD, mood changes are different for different people. Some people with depression feel sad and lose interest in things they used to enjoy, while others feel irritable and have difficulty sleeping. People with anxiety often feel overly worried or concerned, or say they are “on edge.”
The good news: Over the past decade, researchers have placed increasing focus on these aspects of PD, and today we have a better understanding of how to treat mood disorders in Parkinson’s.
You May Like: Masked Facies Parkinson’s Disease
Frequency And Clinical Correlates Of Anxiety Disorders
Several recent studies examined the frequency of anxiety disorders in PD. Negre-Pages et al. assessed 422 ambulatory patients with PD and 98 age- and gender-comparable non-PD individuals using the HADS. The authors reported clinically relevant anxiety symptoms in 50% of non-demented PD patients, while the frequency in the control group was 29%. Of note, there was a strong comorbidity between anxiety and depression.
A recent study assessed 79 PD patients using the Mini International Neuropsychiatric Interview and the Spielberger State-Trait Anxiety Inventory. Twenty-five percent of the sample met DSM-IV diagnostic criteria for a current anxiety disorder, 8% met criteria for panic disorder, 13% for social phobia, and 3% for generalized anxiety disorder. There was a significant association between the presence of anxiety disorders and motor complications , worse quality of life, and older age. Finally, the comorbidity between anxiety and depression was 14%.
Bringing Light To Darker Side Of Parkinsons
Often the hardest part of Parkinsons disease psychosis is the fear of the unknown. As a person with Parkinsons, you may worry about having hallucinations and/or delusions and not being able to do anything about it. As a care partner, you may worry that you wont be able to help your person with Parkinsons feel safe if something does happen.
The good news is you now have information on what Parkinsons disease psychosis is the risk factors to look out for biological and environmental triggers that can bring them on and how to manage them if they show up.
But what about the emotional toll these types of symptoms can place on you over the long-term as the person with Parkinsons or as a care partner?
The diagnosis of a chronic illness in and of itself requires a lot of adjustments. When you add something like Parkinsons disease psychosis into the mix, its important that you also add another level of self-care to your everyday life.
Don’t Miss: Dbs Programming For Parkinson’s
Parkinson’s Disease And Anxiety: Comorbidity With Depression
@article, author=, journal=, year=, volume=, pages=}
- Movement disorders : official journal of the Movement Disorder Society
- View 2 excerpts, cites results
- View 1 excerpt, cites background
- Movement disorders : official journal of the Movement Disorder Society
- View 6 excerpts, cites background and results
Conflict Of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer, DJ, and handling editor declared their shared affiliation, and the handling editor states that the process nevertheless met the standards of a fair and objective review.
Read Also: Antipsychotic For Parkinson’s Psychosis
Management Of Autonomic Symptoms
Autonomic symptoms, including constipation, urinary symptoms, and orthostatic hypotension, are very common in Parkinsons disease. Collaboration between multiple specialties, including urology, GI, neurology, and primary care, is crucial. Notably, dopamine replacement can exacerbate autonomic symptoms, and in more advanced Parkinsons disease the dose of dopaminergic agents may need to be decreased if autonomic symptoms are an issue. Constipation can be severe, and often require harnessing the full arsenal of bowel medications. Orthostatic hypotension is also a concern, and physicians should have a low threshold to check orthostatics in the office and encourage fluid / salt intake if there are hints of issues with dizziness on standing. More severe orthostatic hypotension may require agents like fludrocortisone or midodrine.
Caring For A Loved One With Parkinsons Psychosis
When a loved one is experiencing psychosis, it is important to be patient and avoid arguing with them.
In some cases, your loved one may still have the insight to recognize that these thoughts and feelings are not real. If so, you can explain the reality to them. If they do not have this insight, it is not productive to try to convince them otherwise instead, you should try to remain reassuring and calm.
Be sure that your loved one cannot access anything dangerous when experiencing psychosis and keep the home free of clutter to prevent triggers, falls, and injuries.
Work closely with your loved ones doctors to adjust medications as needed. It can also be helpful to check if eyeglasses or hearing aids are needed and to keep the home well-lit at night. Difficulty in vision and hearing can sometimes trigger hallucinations.
Palliative care can provide added support to family caregivers caring for a loved one with Parkinsons disease. To learn more about how Crossroads Hospice & Palliative Care supports patients with Parkinsons disease, please call 1-888-564-3405.
You May Like: Parkinsonâs Voice Project Live
Don’t Miss: How Hereditary Is Parkinson’s Disease
