Nursing Assessment And Interventions
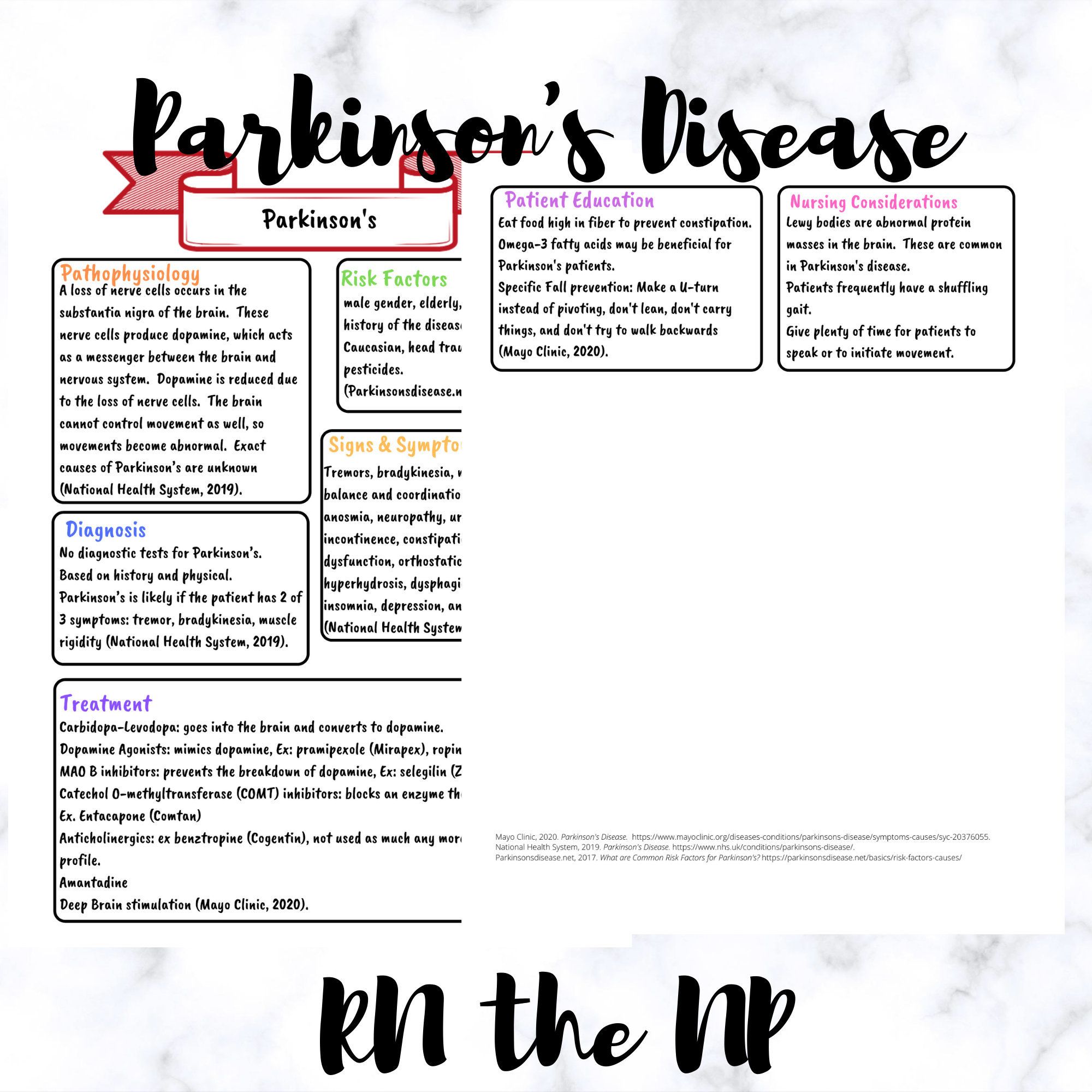
Managing Parkinsons disease is a collaborative effort involving the patient, the patients family or caregiver, and the health care team. On the health care team, the role of the nurse is to provide education about PD, to help monitor medication management, and to help the patient maintain optimal functioning with as much independence as possible. PD is a complex multisystem disease. Symptoms vary from one person to the next. For each individual, symptoms change over time as the disease progresses. The nursing assessment is an ongoing process to monitor the symptoms of the disease and the effectiveness of treatment in managing these symptoms. Assessment includes: history of symptoms physical assessment and specific review of medication effectiveness or side effects.
History ofsymptoms : mobility problems, fatigue, sleep problems, eating/swallowing problems, weight gain or loss, falls, episodes of fainting or feeling light-headed, pain, muscle cramps, constipation, urinary problems, sexual dysfunction, excessive sweating, skin problems, restless leg syndrome, depression or other mood changes, hallucination or delusions, and behavior changes.
A nursing physical assessment includes: evaluation of overall appearance, weight, affect, facial expression, drooling, tremor , muscle rigidity, posture, gait, coordination, speech, skin, scalp, mental status.
Also Check: Does Sam Waterston Have Parkinsons
Nursing Care Plan For Parkinsons Disease 4
Nursing Diagnosis: Disturbed Thought Process related to psychological causes, parkinsonian medications, chronic illness, and depression, secondary to Parkinsons disease as evidenced by memory impairment, distractibility, inability to perform activities, abnormal lab studies, and insomnia.
Desired Outcomes:
- The patient will be able to express understanding of the factors that may produce depressive reactions.
- The patient will use different techniques that will effectively decrease the amount and frequency of depressive reactions.
- The patient will show compliance to the different therapeutic regimens.
Nursing Care Plan For Parkinsons Disease 1
Ineffective Airway Clearance related to Parkinsons disease as evidenced by shortness of breath, SpO2 level of 89%, cough, use of accessory muscles, increased mucus production, difficulty to expectorate phlegm
Desired Outcome: The patient will be able to maintain airway patency and improved airway clearance as evidenced by being able to expectorate phlegm effectively, respiratory rates between 12 to 20 breaths per minutes, oxygen saturation within target range , and verbalize ease of breathing.
Recommended Reading: Is Parkinson’s Disease Neurological
Heterogeneity Instead Of A Clear Line: What Do The Studies Tell Us
Personalized PD care describes a comparatively new approach and has therefore not yet been finally and uniformly established throughout literature. In the included studies, it remained at times unclear whether concepts of personalized care were actively pursued, not only as care models differed significantly, but also due to the applied terminology. These discrepancies are paralleled beyond the scope of this review, insofar as that some aspects of personalized PD care can be met in patient-centered or integrated care models with somehow differing nomenclature . In agreement with this blurred definition, we could identify tasks corresponding to but not matching exactly one of van Halterens five elements of personalized PD care which might nonetheless be attributable to their idea of care according to the individuals needs and preferences . On the one hand, divergency of services may reflect strengths of care models incorporating specific, e.g., regional elements. It is hard to imagine anyone assuming personalized care approaches being a universal concept in the sense of a one-fits-all approach. Otherwise, great heterogeneity in implementation or nomenclature hinders scientific assessment and the development of binding and specific descriptions of professions like PN. In the future theoretical work, a balance between precision and reflection of theories and concepts in the international comparisons is desirable.
Nursing Care Plan For Parkinsons Disease 2
Impaired physical mobility related to disease process of Parkinsons disease as evidenced by bradykinesia, cognitive impairment, inability to bear weight, rigidity, tremors, generalized weakness, inability to do activities of daily living as normal, and verbalization of overwhelming tiredness
Desired Outcome: The patient will be able to perform activities of daily living within the limits of the disease.
Don’t Miss: Nyu Langone Parkinson’s Center
Risk Of Bias Assessment
The articles included in the meta-analysis were independently examined for internal validity utilizing the Cochrane risk-of-bias tool . To ensure interrater reliability, the tool was applied independently by the two researchers . Subsequently, the results were compared and discrepancies were discussed with a third researcher until a consensus was reached.
Nursing Care Plan For Parkinsons Disease 6
Nursing Diagnosis: Deficient Knowledge related to lack of knowledge about Parkinsons disease, difficulty understanding the disease process, lack of coping skills, and cognitive impairment secondary to Parkinsons disease as evidenced by verbalization of questions and incorrect information from the patient and family, presence of preventable complications, and inappropriate behavior.
Desired Outcomes:
- The patient and the patients family will be able to express an accurate understanding of the disease process, medication regimen, and treatment plan of care for Parkinsons disease.
- The patient will be able to fulfill the medication regimen and will notify the physician if the patient experiences unusual side effects.
- The patient will be able to prevent injury by demonstrating safety precautions.
- The patient and the family members will identify the need for long-term goals and the potential for end-of-life decisions to be done.
Recommended Reading: Effects Of Missing Parkinson’s Medication
Nursing Care Plan For Parkinsons Disease 5
Nursing Diagnosis: Impaired Verbal Communication related to the rigidity of facial muscles, lack of stimuli, decreased circulation to the brain, and psychological barriers secondary to Parkinsons disease as evidenced by stuttering, inability to name words, inability to identify objects, inappropriate verbalization, and facial muscle rigidity.
Desired Outcomes:
- The patient will be able to use other methods to communicate and make his or her needs known.
- The patient will be able to use techniques and other assistive devices that will help him or her to improve the patients ability to communicate.
- The patient will be capable of speaking in an understandable way as much as possible.
- The patient will be able to comprehend communication and will be able to exhibit minimal frustration and anxiety with speech attempts.
Read This Article To Learn More About:
- assessing mental health in Parkinsons disease
- the overlap between Parkinsons disease non-motor symptoms and depression
- the role of the Parkinsons disease nurse specialist in supporting people with Parkinsons disease.
Parkinsons disease is a progressive neurological condition that is characterised by tremor, stiffness, and slowness. These overt physical signs are commonly referred to as motor symptoms. However, signs unrelated to movement can manifest along the way, or even before the disease is formally diagnosed these non-motor symptoms can include autonomic, memory, mental health, and mood problems.
When a person is diagnosed with PD, a multi-disciplinary health and social care team often supports them. The team can include neurologists, occupational therapists, and Parkinsons disease nurse specialists . PDNSs are often central in coordinating care, conducting regular monitoring of the person with PD, managing medication, and generally being an accessible source of information and advice for patients, families, and other healthcare professionals. This framework for the role of the PDNS is supported by the 2017 NICE Guideline 71 on Parkinsons disease in adults.1
Recommended Reading: What Happens In Late Stages Of Parkinson’s Disease
Characteristics Of Studies Included
The review consisted of 44 publications published between 1971 and 2021. A total of 43 studies were unicentric, most of them from the United States of America , followed by the United Kingdom , South Korea , Brazil , and Spain . Canada, Italy, Germany, Denmark, Sweden, Netherlands, Turkey, Singapore, Hong Kong had one study each. Only one study was multicenter, with a partnership between the centers of Japan, Thailand, Canada, Denmark, the United Kingdom and the Netherlands.
There is growing interest and research in the area with emphasis on 2019 and 2020. Chronologically, the first three studies analyzed in this review were conducted in the United States. The first was a case report of a patient with PD dating from 1971, then, only after 16 years, another study related to the theme was carried out, being an experimental study.
Regarding the method used, thirteen were quantitative studies, twelve narrative reviews, seven qualitative, seven case reports, three systematic literature reviews, and one study of mixed methods. The included studies targeted people diagnosed with PD and/or their relatives/spouses/caregivers however, few considered the clinical stage of PD when detailing the sample recruitment. Details can be found in Chart 2.
Chart 2.
Impaired Walking/risk For Falls Care Plan
Impaired walking/risk for falls associated with Parkinsons disease can be caused by impaired neuromuscular and musculoskeletal changes. It is also caused by damage to the part of the brain that regulates movement.
Nursing Diagnosis: Impaired Walking/Risk for Falls
Related to:
- Patient will be able to walk around the facility independently with minimum assistance
- Patient will be able to use an assistive device while walking
- Patient will be able to participate actively in physical therapy and rehabilitation
- Patient will not experience falls
Impaired walking/Risk for falls Assessment
1. Assess the neurological status.Parkinsons disease is a chronic condition that progressively affects both the neurological system and musculoskeletal system affecting balance and muscle control. Neurological effects can be tested through grip strength and coordination tests.
2. Assess the patients Parkinsons movement symptoms.Symptoms may include stiff muscles, rigidity, and delayed movement. Patients with mid-stage to advanced PD experience freezing or the feeling of the feet being glued to the floor, as well as short, shuffling steps.
3. Determine the patients ability to move independently.Parkinsons symptoms can be reduced with continuous movement, which can also boost confidence and independence while preventing falls.
Impaired walking/Risk for falls Interventions
You May Like: What Is The Difference Between Alzheimer’s Dementia And Parkinson’s
The Role Of Nurses In Parkinson’s Disease
Research has shown increasing specialization among nurses who care for patients with PD thus, knowledge of the pathophysiology of this disease is arguably an important starting point for vocational training . Based on this, we sought to hierarchically organize the major motor and nonmotor symptoms of PD using evidence gathered from the literature .
Figure 1.
Classification of the main motor and nonmotor symptoms in Parkinson’s disease.
The symptoms of PD are divided into motor and nonmotor each of these classifications contains various other signs and symptoms related to both the neurodegenerative disease process itself as well as multifactorial causes. Thus, hierarchical organization of symptoms is not an easy task, and various descriptions have been proposed to facilitate understanding of the pathophysiology of the disease however, none of them have structured the symptoms into an organizational chart.
Our research on nursing diagnoses, outcomes, and interventions was based on this chart.
Considerations For Future Research In The Field Of Parkinsons Care
Notwithstanding the heterogeneity and diversity of the study results to date, some recommendations for the future are possible. First, scientists should consider the complexity of care research when designing studies and critically appraise which elements should be addressed. Focusing on single theoretical concepts may be helpful in planning studies, but limit the evaluation of results. Care models may be multidisciplinary, patient-centered, integrated, and personalized.
The planning of problem-orientated research is of central importance. From a methodological perspective, we follow previously made recommendations advocating for a head-to-head design, comparing the standard of care with a complex, personalized care intervention or and for implementing cluster-randomized designs, as blinding participants may be hardly achievable. While randomized controlled study designs are considered the gold standard, more pragmatic research approaches also appear as relevant research approaches . Finally, explicit descriptions of the settings, the objectives, the mechanisms of cooperation, the responsibilities and the preliminary theoretical considerations might promote a universal definition of the roles of PN.
You May Like: What Causes Pain In Parkinson’s Patients
Box : Further Assessment Of Depression In Patients With A Chronic Physical Health Problem6
If a patient with a chronic physical health problem answers yes to either of the depression identification questions , a practitioner who is competent to perform a mental health assessment should:
- ask three further questions to improve the accuracy of the assessment of depression, specifically:
- during the last month, have you often been bothered by feelings of worthlessness?
- during the last month, have you often been bothered by poor concentration?
- during the last month, have you often been bothered by thoughts of death?
© NICE 2009. Depression in adults with a chronic physical health problem: recognition and management. Available from www.nice.org.uk/cg91 All rights reserved. Subject to Notice of rights. NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/publication.
Recommended Reading: Cleveland Clinic Parkinsons Bicycle Study 2017
Nursing Care Plan For Parkinsons Disease 3
Nursing Diagnosis: Fatigue related to disease process of Parkinsons disease as evidenced by generalized weakness, tremors, muscular rigidity, and verbalization of overwhelming tiredness
Desired Outcome: The patient will demonstration active participation in necessary and desired activities and demonstrate increase in activity levels.
Also Check: Dbs Treatment For Parkinson’s
Parkinsons Disease: Symptoms Treatment Options And Nursing Care
Phil Cotterell Parkinsons disease nurse specialist, Community Neurological Rehabilitation Team, Sussex Community NHS Foundation Trust, Worthing, England
Why you should read this article:
-
» To understand your role in supporting and improving the quality of life of patients with Parkinsons disease and their family and carers
-
» To recognise motor and non-motor symptoms of Parkinsons disease and potential treatment options
-
» To ensure the care you provide to patients is holistic and considers not only the physical effect of Parkinsons disease, but also the psychological and emotional effects that individuals may experience
Idiopathic Parkinsons disease is a progressive neurodegenerative condition that causes various motor and non-motor symptoms and will often have life-changing effects for those with the condition, as well as for their family and carers. Nurses can make a significant difference to the lives of those affected by Parkinsons disease, whether in the acute setting, community setting or in care homes. This article explores the causes and progressive clinical pathway of IPD using an evidence-based approach. It emphasises the valuable role of the multidisciplinary team and of the nurse, in particular, in monitoring and improving the quality of life of those with the condition and their family and carers.
Nursing Standard. doi: 10.7748/ns.2018.e11207
Impaired Swallowing Care Plan
Impaired swallowing associated with Parkinsons disease is caused by the inability to control throat and mouth muscles resulting in difficulty chewing and swallowing food. This can lead to aspiration pneumonia, which is the leading cause of death in PD.
Nursing Diagnosis: Impaired Swallowing
- Inability to control throat and mouth muscles
- Degeneration of nerve cells
- Blank facial expression
- Coughing while eating or drinking
- Clearing of the throat while eating or drinking
- A feeling of food stuck in the throat during feeding
Expected outcomes:
- Patient will demonstrate appropriate swallowing without coughing/gagging, drooling, or pocketing food
- Patient will be able to maintain an acceptable weight for their height and gender
- Patient will not develop aspiration pneumonia
Impaired Swallowing Assessment
1. Assess the patients ability to swallow and chew.The muscles in the throat that regulate food passage can stiffen or become slow-moving, which may leave residue in the throat. The patient may complain of food stuck in the throat. The nurse can perform a bedside swallow assessment by giving the patient a teaspoon of water and ensuring the patient can swallow without gagging or coughing.
2. Monitor the patients weight.Weight and nutritional status must be consistently monitored. Impaired swallowing is associated with weight loss in PD.
3. Assess for signs of aspiration pneumonia.Fever, dyspnea, chest pain, coughing, and lethargy are signs of possible aspiration pneumonia.
Recommended Reading: How To Help With Parkinson Disease
Diagnosis Of Parkinsons Disease
There is no specific diagnostic procedure to diagnose PD. However, the following are helpful to come up with the diagnosis:
- Medical History Taking
- Physical Examination
- Single Photon Emission CT scan -this form of imaging shows the blood flow to tissues and organs
- Dopamine transporter scan this imaging is often used to confirm the diagnosis of PD. It is not typically requested as medical history and physical examination are often conclusive.
Caring For Patients With Parkinsons Disease In General Hospital Settings
Vicky Queen Parkinsons disease nurse specialist, Torbay Hospital, Torbay and South Devon NHS Foundation Trust, Torquay, England
Parkinsons disease is a common progressive neurological condition. There are 127,000 people with the disease in the UK, that is, one in every 500 of the population. In 2014-15 there were 14,000 hospital admissions of people with PD in England. However, PD is often not the primary cause of admission. Urinary tract infections and pneumonia, for example, are frequent causes of hospital admission for people with PD. Therefore, nurses on general medical and surgical wards will often care for people with PD. This article aims to provide an update on PD and explore the nurses role in assessment and provision of safe and effective care for patients with PD in acute hospital settings.
Nursing Older People.29, 5, 30-37. doi: 10.7748/nop.2017.e861
Correspondence
Recommended Reading: Parkinsons Phase 3 Trials
Also Check: Parkinson’s Support Group Nyc
Impaired Verbal Communication Care Plan
Impaired verbal communication associated with Parkinsons disease can be caused by the inability to control the muscles on the face, throat, mouth, and vocal cords resulting in difficulty to speak and communicate. It is also caused by damage to the part of the brain that regulates speech and comprehension.
Differences In Home Health Nursing Care For Patients With Parkinsons Disease By Stage Of Progress: Patients In Hoehn And Yahr Stages Iii Iv And V
Yumi Iwasa
1Department of Nursing, Graduate School of Health Sciences, Kobe University, Tomogaoka, Suma-ku, Kobe, Hyogo 654-0142, Japan
2Akebi Home-Visit Nursing Station, Hosoe, Shikama-ku, Himeji, Hyogo 672-8064, Japan
Abstract
1. Introduction
Parkinsons disease is a neurodegenerative disease with no radical cure. In Japan, patients above stage III on the Hoehn and Yahr scale are eligible for public medical expense subsidies. When calculated using the Japanese population, the adjusted prevalence of the disease is 166.8 per 100,000 individuals .
It is important for patients with PD in long-term medical treatment to receive physical therapy to maintain bodily functions and pharmacotherapy, centering primarily on L-Dopa, to achieve symptomatic relief both of these efforts require effective care protocols. When provided by nurses, programs that involve counseling, medication information, and collaboration with local organizations during hospitalization and discharge are known to be effective for supporting patients with PD. In the West, PD nurse specialists perform these roles and, in recent years, efforts to improve these nursing activities have resulted in studies and surveys leading to the creation of nursing practice guidelines . Due to the need to enhance the effectiveness of nursing care provided to patients with PD, the movement to maintain and further improve the quality of care is increasing globally.
2. Methods
2.1. Participants and Collected Data
3. Results
Also Check: Does Parkinson’s Disease Affect The Brain
