Whats The Relationship Between Parkinsons And Sleep
Parkinsons disease and sleep are connected in complex ways that not even scientists completely understand quite yet.
Sometimes, Parkinsons disease directly causes sleep problems. According to one study, sleep-related symptoms may be one of the earliest signs of Parkinsons disease. These signs may include things like thrashing while youre asleep.
Other factors can also play a role. One thing is clear: For many people with Parkinsons disease, a restful nights sleep can be hard to find.
How Are Sleep Problems Diagnosed In People With Parkinsons Disease
If youre having problems sleeping, sit down with your healthcare provider to discuss the issue in detail. Your provider will ask you questions to better understand your symptoms.
Be prepared to explain when sleep disruptions happen and how they affect your life. Keeping a sleep journal for a few weeks can help you remember the details.
If your provider suspects you may have a sleep disorder, they may recommend you have a sleep study. This overnight test uses electrodes attached to your skin to track how your body functions when youre sleeping.
Additional Disorders And Related Symptoms Impacting Sleep
Restless Leg Syndrome
Q: My wife has restless leg syndrome but not Parkinsons. She is not getting enough relief. Are there doctors who specialize in RLS?
A: Both Sleep specialists and Movement disorders specialists see patients with RLS.
Age-Related Sleep Problems
Q: Could occasional sleep problems just be age related?
A: Not every symptom that someone with PD experiences is caused by PD. Many people in the general population experience sleep problems and many of the strategies that were discussed by Dr. Ospina can be relevant for a wider audience. Also keep in mind that if the problems are not persistent and only occasional, no treatment may be necessary at all.
Progressive Supranuclear Palsy
Q: Do people with Progressive supranuclear palsy also have problems with their sleep?
A: Yes, people with PSP can also have difficulties with their sleep, with much overlap with the problems seen by people with PD. Many of the same approaches would be used for people with PSP.
Deep Brain Stimulation
Q: Can deep brain stimulation make sleep worse?
A: This is not a common complaint. In fact, several studies have shown that subthalamic nucleus DBS improves subjective and objective measures of sleep, including sleep efficiency, nocturnal mobility, and wake after sleep onset. However, every person is different, and your reaction to DBS might be different than others.
Read Also: Why Do Parkinson’s Patients Hallucinate
How Can I Reduce The Consequences Of This Sleep Disorder
Treatment usually involves a combination of medication and a change in sleeping habits.
Before you see a doctor, you can use strategies to reduce the impact of these dreams on you and your partners safety. Here are some of these strategies:
- Make sure there are no sharp objects near the bed
- Place the bed against the wall or put pillows to prevent falls
- Consider installing safety rails on the bed
- Place sharp objects and furniture away from the bed
- Move the bed away from windows
- Sleep in separate rooms if your behaviour becomes too much of an inconvenience
An occupational therapists advice can also provide you with several concrete solutions to make your sleep environment safer and prevent injuries.
Recommended Reading: On-off Phenomenon
How Does Parkinsons Disease Cause Sleep Problems

Researchers have yet to uncover every nuance of the Parkinsons and sleep connection. So far, medical experts believe several causes may contribute:
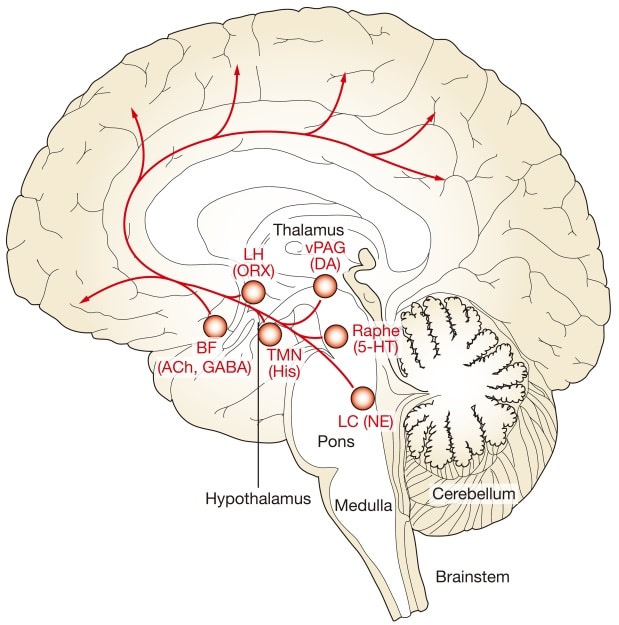
- Chemical changes in the brain: Ongoing research shows that Parkinsons disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinsons to get less sleep.
- Medication: Some drugs that treat Parkinsons disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinsons commonly deal with mood disorders, such as anxiety or depression. Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinsons symptoms: Pain, waking up at night to pee or other Parkinsons symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Don’t Miss: Can You Be Tested For The Parkinson’s Gene
Parkinsons Disease And Sleep
Reviewed by David Rye, MD, and Mark Mahowald, MD. Published by the National Sleep Foundation
This web article offers a detailed description of Parkinsons disease and the challenges it presents to restorative rest and recuperation. Some suggestions are included for improving sleep and the environment around sleeping.
Clinical Features Of Insomnia
Insomnia is defined as difficulties initiating sleep , sleep maintenance problem or early awakening . In studies, it has been reported that the frequency of insomnia in patients with PD varies from 27 to 80% . It has been reported that the most common types of insomnia in PD patients are sleep fragmentation , and early awakenings . It has been reported that insomnia may occur alone or accompany comorbid mental or systemic illnesses, and it is associated with disease duration and female gender . Sleep fragmentation is defined as a deterioration of sleep integrity , and it leads to a lighter sleep or wakefulness . In studies, it has been reported that sleep fragmentation is the most common sleep disorder in patients with PD .
Read Also: Does Black Seed Oil Help Parkinson’s Disease
Classification Of Sleep Disorders In Parkinsons Disease
Sleep disorders in PD may occur during the day or at night. In PD, sleep disorders can be classified into three major categories such as abnormal behaviors and events during or around sleep , inability to sleep , and EDS . These three categories of sleep disorders can be seen separately or together .
| Categories |
|---|
Spend Time Outside During The Day
Take advantage of the sunlight when its out in the daytime. Consider spending time outdoors for exercise. Simple walking or running can contribute to your daily exercise quota, but avoid heavy exercises and activities after 8:00 PM.
Your goal for spending time outdoors is to get enough light. You could invest in a light therapy box for artificial light if you have trouble going outdoors. Such tools are available at drug stores.
Read Also: Is Parkinson’s Related To Dementia
Modifying The Accumulation Of Abnormal Proteins And Disturbed Sleep: The Glymphatic System
Abnormal build-up of proteins, such as -synuclein, amyloid-, TDP-43, or phosphorylated tau may occur in PD. The glymphatic system is a paravascular pathway that promotes clearance of waste products from the brain . The glymphatic system has been implicated in clearing soluble species of amyloid- in patients with AD allowing potentially toxic proteins to clear the brain and prevent the build-up of pathological deposits.
Nonetheless, glymphatic clearance promoting intervention still may be of benefit in the early motor symptomatic phase of PD as -synuclein spreading may extend beyond mesencephalic and limbic regions. Furthermore, subsequent development of dementia in PD is also associated with co-occurring AD pathology. Therefore, sleep or glymphatic clearance enhancing strategies may also lower the build-up of non--synuclein protein deposits in advancing PD at risk of dementia. Sleep enhancing interventions that promote glymphatic clearance may therefore have the potential to serve important disease-modifying goals in PD.
Fig.2
Treatment Of Excessive Daytime Sleepiness In Pd
The first step in the treatment of EDS should be the correction of underlying conditions . For example, it may be useful to treat the conditions that disturb sleep quality at night or to arrange medications that cause daytime sleep episodes. After that, pharmacological treatment options for EDS should be considered. Nonpharmacological treatment approaches can be performed in the treatment of mild to moderate EDS cases . Modafinil is widely used for the symptomatic treatment of EDS, which appears to stimulate catecholamine production . Common side effects of modafinil are insomnia, headache, dry mouth, dizziness, nausea, nervousness, and depression . A review has reported that sodium oxybate and methylphenidate have inadequate evidence that they are effective in the treatment of EDS in PD . Amantadine and selegiline are reported to have an alerting effect . Thus, amantadine and selegiline may be preferentially used in PD patients with EDS.
Don’t Miss: How Long Can Someone Live With Stage 5 Parkinson’s
Recurrent Falls In Parkinsons Disease: A Systematic Review
Natalie E. Allen
1Clinical and Rehabilitation Sciences Research Group, Faculty of Health Sciences, The University of Sydney, P.O. Box 170, Lidcombe, NSW 1825, Australia
Abstract
Most people with Parkinsons disease fall and many experience recurrent falls. The aim of this review was to examine the scope of recurrent falls and to identify factors associated with recurrent fallers. A database search for journal articles which reported prospectively collected information concerning recurrent falls in people with PD identified 22 studies. In these studies, 60.5% of participants reported at least one fall, with 39% reporting recurrent falls. Recurrent fallers reported an average of 4.7 to 67.6 falls per person per year . Factors associated with recurrent falls include: a positive fall history, increased disease severity and duration, increased motor impairment, treatment with dopamine agonists, increased levodopa dosage, cognitive impairment, fear of falling, freezing of gait, impaired mobility and reduced physical activity. The wide range in the frequency of recurrent falls experienced by people with PD suggests that it would be beneficial to classify recurrent fallers into sub-groups based on fall frequency. Given that there are several factors particularly associated with recurrent falls, fall management and prevention strategies specifically targeting recurrent fallers require urgent evaluation in order to inform clinical practice.
1. Introduction
Support For People Living With Parkinsons Disease
While the progression of Parkinsons is usually slow, eventually a persons daily routines may be affected. Activities such as working, taking care of a home, and participating in social activities with friends may become challenging. Experiencing these changes can be difficult, but support groups can help people cope. These groups can provide information, advice, and connections to resources for those living with Parkinsons disease, their families, and caregivers. The organizations listed below can help people find local support groups and other resources in their communities.
Also Check: Toxic Causes Of Parkinson Disease
Recommended Reading: What Is The Medication For Parkinson Disease
Sleep Disorders In Parkinsons Disease
In this 17-minute lecture Dr Gary Leo discuses sleep challenges caused by the neurochemical changes, medications and mood disturbances of Parkinsons disease, and normal changes of aging. He discusses possible causes and treatment options of sleep maintenance insomnia, REM Sleep Behavior Disorder, daytime sleepiness, sleep apnea, and restless leg syndrome, ending with some tips for good sleep.
Good Night: Sleep And Parkinsons Disease
Lack of good sleep can worsen Parkinsons symptoms. In this 45-minute lecture, Dr. Rafael Zuzuárregui addresses causes of sleep loss and the latest treatments for: insomnia, restless leg syndrome, REM sleep behavior disorder, nocturnal urination, hallucinations, wearing off of medication, dystonia and sleep apnea.
Recommended Reading: Does Parkinson’s Cause Depression
Sleep And Parkinsons Disease
The Palo Alto Parkinsons Disease support group February 2020 meeting featured Dr. Emmanuel During, a Stanford sleep medicine neurologist. During the meeting, Dr. During discusses sleep disturbances that can occur in PD, such as insomnia, restles legs syndrome, sleep apnea, and REM sleep behavior disorder , along with available treatments. There’s a question and answer session.
Diagnostic Assessment Of Sleep Disorders In Pd
The history taken from the patient and its neighbors is very important in assessing sleep disorders in PD. The type of sleep disorder should be identified in the history, and information about possible related factors should be obtained from the history. In PD, general and specific scales can be used to investigate the subtype of sleep disorder and to determine its severity. Objective methods can be used to further investigate the diagnosis of these disorders. Further investigative techniques include sleep recording methods such as actigraphy or PSG. Polysomnographic findings of each sleep disorder have been explained in the relevant section. In addition, information about screening scales used in each sleep disorder has been described in the relevant section.
Actigraphy is an electrophysiological device that measures the movements of the patient during sleep by recording from wrist or ankle for many days. Actigraphy evaluates indirectly the circadian sleepwake patterns . It is especially used in circadian rhythm disorders or insomnia and prolonged daytime sleepiness .
Read Also: Can Spinal Stenosis Mimic Parkinson’s
What Are The Causes And Symptoms Of Parkinsons Disease
As a neurodegenerative disorder, Parkinsons Disease leads to the progressive deterioration of motor function due to loss of dopamine-producing brain cells. While the cause of Parkinsons Disease is unknown, researchers speculate that both genetic and environmental factors are involved. Studies also show that men are 50% more likely to develop the disorder than women.
Primary symptoms of Parkinsons Disease:
Dont Miss: Prayers For Parkinsons Disease
Ways To Reduce The Risk Of Falling
There are several steps people living with PD can take to reduce their risk of falling, including:
- Talk to your doctor about your risks. Your doctor can assess your personal risk and can help you manage your medications and any side effects. Medications may need to be adjusted or switched up.
- Exercising regularly helps maintain strength, improve stamina, improve balance, and reduce the risk of falls. Exercises that challenge your balance are especially beneficial, and research has shown that exercise that requires your attention, concentration and focus on activity and movement may also be neuroprotective protecting the nerve cells from damage and possibly slowing the progression of PD.
- Make modifications to your home. There are several adaptations that can be made in your home to make falls less likely, such as removing throw rugs, ensuring wide pathways through furniture, and adding non-skid mats and grab bars to showers and bathtubs.
- Use a walking aid.Canes or four-wheeled walkers offer stability for people with PD.
- Learn ways to overcome freezing episodes, such as walking in beat to music or a metronome. Some people also find it helpful to move from side to side before stepping forward.
- Work with a physical therapist or occupational therapist.Physical and occupational therapists can provide exercises to help keep you mobile. Occupational therapists also can suggest adaptations and modifications to the persons environment.1,3-5
Also Check: How Do You Find Out If You Have Parkinson Disease
Beating The Lockdown Blues
Did you knowBodily functions are heavily influenced by biological clocks which are distributed throughout your body . Your clocks primary role is timing and orchestrating your bodys everyday vital functions and aligning these to geophysical and social schedules. Disruptions to your daily routine derail your clock which reflects negatively on your mood, energy, sleep, digestion, heart and immune system, just to name a few!
With COVID-19-related lockdowns causing unanticipated disruptions to our routine, Researchers at the University of Queensland have developed some guidelines to stay on a schedule to improve sleep and support your health and wellbeing.
Sleep: A Mind Guide To Parkinsons Disease

This 36-page booklet explains normal sleep patterns, the body clock, how much sleep we should get, challenges to sleeping well, tips for good sleep hygiene, and sleep in normal aging before discussing symptoms, diagnosis and treatment of sleep disorders, including insomnia, REM sleep behavior disorder, sleep apnea, restless leg syndrome, and daytime sleepiness.
Read Also: What To Expect With Parkinson’s
The Relationship Between Parkinsons Disease And Sleep
Its unclear whether poor sleep causes parkinsonian symptoms to worsen or whether worsening parkinsonian symptoms cause poor sleep. In many cases its likely a case of bidirectionality, with each one exacerbating the other.
Fragmented sleep and sleep deprivation appear to leave the brain more vulnerable to oxidative stress, which has been tied to the development of Parkinsons disease. Parkinsons disease is not usually diagnosed until individuals have developed sufficient motor symptoms, by which time a significant portion of brain cells have already been damaged. If poor sleep quality or having sleep disorders foreshadows the development of parkinsonian symptoms, these could be useful in early diagnosis of the disease.
More research is needed to clarify the multifaceted relationship between Parkinsons disease and sleep. A better understanding of this connection may offer medical experts the unique opportunity to screen at-risk individuals and perhaps delay the onset of the disease.
Circadian Rhythm Sleep Disorders
Circadian rhythm sleep disorders potentially influence daytime and nocturnal dysfunctions. It is common to find that PD patients go to bed and wake up very early therefore, a phase advance may occur . Advanced sleep phase is usually associated with older age and characterized by involuntary sleep and waking times that are generally more than 3 h earlier than usual sleep times. For patients with PD, both age-related changes and brain damage can provoke circadian rhythm sleep abnormalities. This relationship deserves more careful clarification, although it is complex. For instance, a slower absorption rate of levodopa during nighttime, possibly related to delayed gastric emptying, has been reported in PD patients . In agreement with this example, it has been documented that phase advance in PD is possibly influenced not only by age but also by dopaminergic therapy and disease severity . Given the complexity of this issue, an abnormal pattern of daily activities and associated comorbidities, such as depressive symptoms and daytime sleepiness, could also influence circadian rhythms . Thus, the analysis of this complex issue must take all of these variables into careful consideration.
Don’t Miss: What Helps With Parkinson’s Disease
Highlights From The Episode
In case you missed it, the August broadcast of Dr. Gilbert Hosts was a very informative conversation, and we encourage you to watch the full episode. For your convenience, weve listed the topics and questions from the episode below with timestamps, so you can skip to what may interest you most:
00:48 Introduction of Dr. Ospina
01:27 Dr. Ospinas presentation about sleep issues
23:37 My husband sleeps fairly well at night but sleeps a lot during the day. How do we get him to not sleep so much during the day?
25:19 My father has had much improvement in his sleep by taking CBD. What is your opinion on this?
27:20 Discussion of OFF time
31:23 Will Prozac affect my sleep? Is it better to take it in the morning or at lunch rather than at night?
32:48 Does deep brain stimulation help insomnia and sleep issues?
35:13 I wake up frequently with leg and foot cramps/dystonia. How should I treat this?
36:51 Is it OK to take Nyquil for insomnia? Melatonin? If so, how much melatonin should I take?
38:05 Could numbness in the feet be associated with restless leg syndrome?
39:36 Can you get accustomed to sleep medications whereby the medication is no longer effective?
40:40 What should I do if Im wide awake in the middle of the night? Should I try to be active and get something done, or should I try to stay in bed?
