What Is The Meaning Of Shuffling Gait
Let us think about a fictional person, Sue. Sue has a normal gait.
Sue starts walking.
Sue first lifts one foot up. Then he moves that foot forward. After the foot is adequately in front, Sue stops moving it forward. She then places the foot down on the ground.
Sue can do this very rapidly, and walk very fast.
Usually, we walk like Sue. We do not shuffle.
==
Shuffling gait means a peculiar way of walking, in which the foot is still moving when it hits the ground.
Let us look at another person, Mary.
Mary does not lift the foot high off the ground. She moves it forward slowly. Even before he/she moves it forward adequately, it is time to put the foot down! And so she does so.
This causes Mary to shuffle while walking. This is the meaning of a shuffling gait.
See this sample video of bradykinesia posted by a Russian doctor on youtube:
Why Do People With Parkinsons Shuffle
4.4/5FallsFalls
Parkinsonian gait is a defining feature of Parkinsons disease, especially in later stages. People with Parkinsonian gait usually take small, shuffling steps. They might have difficulty picking up their feet. Parkinsonian gait changes can be episodic or continuous.
Subsequently, question is, what helps Parkinsons patients walk? To lower your risk of falling:
Besides, what is the cause of a shuffling gait?
An unsteady gait or shuffling walk could be caused by something as simple as slippery floors or as serious as dementia or Parkinsons disease. So if your older adult has started shuffling their feet when walking, its important to schedule an appointment with their doctor to find out whats causing it.
How does Parkinsons affect movement?
Parkinsons disease is a type of central nervous system disorder that affects your movement, causing symptoms such as tremors, slowness, stiffness, and more. These involuntary movements begin, in part, in the brain, where the production of dopamine is impaired.
Maintaining Your Normal Pd Medication Schedule
Maintaining your PD medication schedule is crucial for anyone with PD. The correct timing and dosage are essential to your comfort and well-being. However, oftentimes when undergoing surgery, there may be restrictions regarding when you can and cannot take medications. Here are a few tips to navigate this issue:
What Does Lewy Body Dementia Look Like
Lewy body dementia affects a persons ability to think and process information and it can negatively impact memory and alter personality. Though it shares aspects of other forms of dementia, there are distinct hallmarks of LBD. Lewy body dementia symptoms include:
- Fluctuating attention/alertness: These shifts can last hours or go on for days. The person may stare into space, appear lethargic or drowsy, and have hard-to-understand speech, appearing a lot like delirium. At other times, the person may have much more clarity of thought.
- Visual hallucinations: Often, these are very detailed hallucinations and visions of people or animals, and they can recur.
- Movement disorders: Parkinsons-like movement issues, such as muscle rigidity, tremors, falls, or a shuffling gait or way of walking, may occur.
Medications Used For Treating Psychosis
Antipsychotic agents are designed to balance abnormal chemical levels in the brain. Up until the 1990s, the use of antipsychotics in PD was controversial because the drugs used until that time work by reducing excess dopamine. This alleviated psychosis but caused dramatic worsening of PD motor symptoms.
Fortunately, medications that are better tolerated by people with PD are now available. Today, there are threeantipsychotic medications considered relatively safe for people with PD: quetiapine , clozapine and the newest agent, pimavanserin . They cause limited worsening of PD while treating hallucinations and delusions.
Demystifying Hallucinations Night Terrors And Dementia In Parkinsons
This two-hour webinar includes extensive discussion about hallucinations, delusions, illusions and other examples of Parkinsons psychosis in Parkinson’s. Presenters: Rohit Dhall, MD, MSPH and Vergilio Gerald H. Evidente, Director, Movement Disorders Center of Arizona in Scottsdale. Pay particular attention to Dr. Rohit Dhalls description of the causes of PD psychosis as well as treatment options and what to discuss with your movement disorder specialist. Dr. Evidente gives a clear description on differences in PD dementia, Alzheimer’s and other dementias.
How Are They Treated
Your medical team should be aware of non-motor issues, just like your physical symptoms. Internists, neurologists, and psychiatrists together can help determine the right course for each person.
There are antipsychotic medications that are safe and can help to reduce the symptoms of Parkinson’s disease psychosis, but there are even more antipsychotics that are contraindicated for PD.
Let a medical provider know you have Parkinson’s when seeking emergency care or treatment for something by doctors who are not a part of your regular medical team.
There is only one drug, pimavanserin, approved in 2016 by the FDA specifically for PD. It has a mechanism of action that doesn’t block dopamine. This has made it a safer drug for people with Parkinson’s.2
Two other , quetiapine and clozapine, that have been used for a longer time, are also considered safe for treating hallucinations and delusions in people with PD.2
Hallucinations And Delusions In Pd
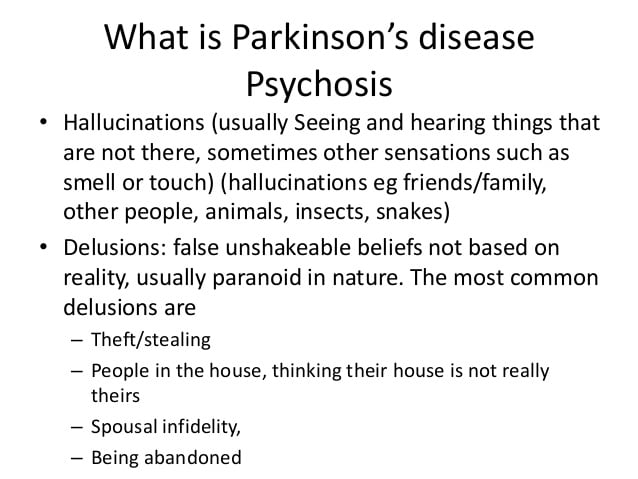
Hallucinations and delusions are collectively referred to as psychosis.
Visual hallucinations are the most common type of hallucination. In a visual hallucination, someone sees things that are not actually there. There can also be auditory and olfactory hallucinations. Often hallucinations are not alarming to the person experiencing them.
Delusions are when there is an alternative view of reality: an entire irrational story is created. Paranoia is a common type of delusion. Capgras delusions are a specific type of delusion where the person believes that a spouse, adult child, or other family member has been replaced by an imposter.
Lewy Body Dementia: A Common Yet Underdiagnosed Dementia
While its not a household word yet, Lewy body dementia is not a rare disease. It affects an estimated 1.4 million individuals and their families in the United States. Because LBD symptoms can closely resemble other more commonly known disorders like Alzheimers disease and , it is often underdiagnosed or misdiagnosed. In fact, many doctors or other medical professionals still are not familiar with LBD.
Why Do Seniors Develop A Shuffling Gait
As seniors reach the golden years, they sometimes develop a shuffling gait. While family caregivers may view this development as normal, any changes in your aging loved ones gait shouldnt be ignored. Your loved ones tendency to drag his or her feet could be linked to one of the following issues that needs to be addressed right away.
How Can You Reduce Shuffling Gait
has long been hailed and proven to be an effective way of slowing down the effects of Parkinsons. Dr Horak says the same applies for improving balance and Parkinsons gait. Therapy and exercise can improve balance and gait but the specific type of exercise will depend on each persons abilities.
Dr Horak recently co-authored a study on the effects of a group exercise class on gait and brain connectivity in people with Parkinsons for whom the major form of disability is impaired mobility.
She explains: We studied 85 people with mild to moderate Parkinsons who took part in a six-week agility bootcamp with cognitive challenges. We found that the ability to walk quickly with less shuffling improved particularly in those with the strongest shuffle to begin with.
As well as exercising, Dr Horak suggests people with Parkinsons try and improve gait by taking part in gait rehabilitation with a physical therapist, using walking aids such as hiking sticks or a rolling walker, or monitoring the change in movements over time using wearable technology.
Similarly, there is evidence to suggest walking to the beat of a metronome or music may reduce shuffling, improve walking speed and limit freezing of gait.
For more information about Parkinsons and gait please visit the EPDA website.
Read more:
Predictive Factors And Pathophysiology
Minor hallucinations/illusions
Patients with isolated minor hallucinations/illusions differed from patients without hallucinations only by the presence of more depressive symptoms on the CES-D rating scale, suggesting that depressive symptoms are a facilitating factor. Indeed, depression may sometimes trigger or aggravate hallucinations associated with deafness or ocular pathology . However, when we analysed depression according to CES-D cut-off scores, the difference between the Parkinson’s disease patients with minor hallucinations/illusions and those with no hallucinations was not significant. Interestingly, hallucinations involving the deceased spouse have been reported in up to half of widowed persons, with a higher frequency in the elderly . In the present study, the `presence’ was that of a deceased relative in only three cases ; bereavement cannot therefore explain the bulk of the cases.
Dopaminergic agents and other treatments
In the present study, non-hallucinators were more likely to be on anticholinergics or selegiline than patients with hallucinations. A similar paradoxical, negative association between anticholinergics and hallucinations was found by Sanchez-Ramos and colleagues . This reflects the recommendation whereby the use of these drugs in patients with cognitive impairment is avoided because of the well-known risk of cognitive worsening and/or hallucinations in this population.
Cognitive impairment
Sleepwake disturbances
Motor status
Depression
What Should I Do Once The Hallucination Passes
After the hallucination passes, you can try to talk through the experience together. If the person has insight, it may be easier for them to understand and talk about what just happened.
Write down what happened during the hallucination. Note the time of day and what the person was doing when it started.
Taking notes each time it happens can help you identify the triggers. It could be related to the timing of medication, and your loved one might feel a sense of relief and control in knowing that pattern.
Ask what you can do to stop it from happening again. This might include adjusting their medication dosage or adding an atypical antipsychotic drug to their medication regimen.
What Can I Expect If I Or My Loved One Have A Diagnosis Of Lewy Body Dementia
Each persons experience with Lewy body dementia is unique to them. How slowly or quickly the disease progresses is impossible to know, but may be influenced by your general health and any existing diseases you may have. Because LBD is a progressive disease, difficulties with mind and body functions get worse over time. Currently, there is no known way to stop the progression of the disease. After diagnosis, most people with LBD live between five and seven years. Some people with LBD live up to 20 years after their diagnosis.
However, theres always hope. Research on LBD, dementia with lewy bodies, Alzheimers disease, Parkinsons disease with dementia are ongoing. New medications are being developed and new approaches to treatment are being investigated.
Join The Parkinsons News Today Forums And Share Your Experience With Hallucinations And Other Pd Symptoms
Most patients reported having hallucinations for at least one year, the researchers wrote. A difference noted: Parkinsons patients tended tosee images of people and animals not actually present, while dementia patients tended to experience people or presence hallucinations.
Patients were asked about their experiences and interpretations of such hallucinations, their impact on relationships and daily life, and information or support they had asked for or received regarding them.
Caregivers were asked to reflect upon their own reactions and any support they might have received.
All patients were assessed for vision, cognition, and motor function skills.
Differences in the VH experience between persons with dementia and PD were less striking than the overall similarities across conditions at equivalent stages of cognitive and insight impairment, the researchers wrote.
Patients reported disease aspects such as loss of independence and depression as more concerning and difficult than hallucinations, while those with poorer cognitive abilities voiced greater distress with visual hallucinations.
Three overall themes emerged in the study:
An ability to understand and distinguish a visual hallucination from reality called insight by the research team influenced how the threat of such hallucinations was perceived and whether acceptance occurred over time.Reactions to visual hallucinations and coping strategies varied as insights changed with disease progression.
How To Care For Someone Who Experiences Delusions
If the person youre caring for experiences confusion or delusions, heres what you can do in the moment:
- Stay as calm and patient as you can and remember that this belief has nothing to do with you and only with what is going on in their mind
- Remove any objects in the room that could pose a danger to them or to anyone else
- Clear space so there are no tripping hazards and its easy for the person to move around
- Do not try to reason with the person or convince them why their belief is false
- Reassure them that everything is going to be okay
- If the person becomes aggressive, minimize your movements and remain calm
- Ask the person to talk to you about what they are feeling and really listen to them so they dont feel threatened
- If you feel like you or they are in danger, call 911
Here are a few actions you can take once the delusion has passed:
- Inform their doctor immediately
- Educate others who may care for the person how to handle the situation if it happens
- If the person is open to it, discuss it with them and ask them to explain what the experience is like for them and if theres anything different you could do next time
- Seek expert advice if you feel like you need support in managing these episodes
Age And Duration Of Illness
Increased age has been associated with the presence of hallucinations. This might be explained by accerelated sensory loss or age related side effects of medication. One of the main confounders with age is duration of illness; when the non-independence of these variables was controlled, Fnelon et alfound that duration of illness was the crucial factor. Grahamet al identified two subgroups of patients with Parkinson’s disease experiencing hallucinosis: in those with disease duration of 5 years or less, visual hallucinations were associated with rapid progression of the motor but not the cognitive component of the disease. In the remainder with longer histories, visual hallucinations were associated with postural instability, global cognitive impairment, and the lack of depression. Goetz et al contrasted patients with Parkinson’s disease who experienced hallucinations within 3 months of levodopa therapy with those who experienced hallucinations after 1 year of treatment. Diagnoses in the early onset group more often changed to Lewy body or Alzheimer’s disease. Lewy bodies are present to a greater or lesser degree in all cases of Parkinson’s disease and are known to be associated with visual hallucinations.
Outlook For Dementia With Lewy Bodies
How quickly dementia with Lewy bodies gets worse varies from person to person.
Home-based help will usually be needed, and some people will eventually need care in a nursing home.
The average survival time after diagnosis is similar to that of Alzheimers disease around 6 to 12 years. But this is highly variable and some people live much longer than this.
If you or a loved one has been diagnosed with dementia, remember that youre not alone. The NHS and social services, as well as voluntary organisations, can provide advice and support for you and your family.
Hallucinations And Delusions In Parkinsons Disease
It might be surprising to learn that 20 to 30 percent of people with Parkinsons disease will experience visual hallucinations. While typically not a symptom of PD itself, they can develop as a result to a change in PD medication or as a symptom of an unrelated infection or illness. It is important to know the signs of hallucinations and how to manage them.
Hallucinations and other more severe perceptual changes can be distressing to family often more so than to the person experiencing them. For the well-being of people with PD and caregivers, it is important to identify hallucinations as early as possible and take steps to reduce them.
The following article is based on the latest research and a Parkinsons Foundation Expert Briefingsabout hallucinations and delusions in Parkinsons hosted by Christopher G. Goetz, MD, Professor of Neurological Sciences, Professor of Pharmacology at Rush University Medical Center, a Parkinsons FoundationCenter of Excellence.
What Is Lewy Body Disease
Lewy body disease is caused by the degeneration and death of nerve cells in the brain. The name comes from the presence of abnormal spherical structures, called Lewy bodies, which develop inside nerve cells. It is thought that these may contribute to the death of the brain cells. They are named after the doctor who first wrote about them. It is sometimes referred to as Diffuse Lewy body disease.
Parkinsons Disease Psychosis: A Little

One of the lesser-known symptoms of Parkinsons Disease is Parkinsons psychosis. This webpage explains the prevalence, causes and symptoms, treatment options of PD psychosis. More useful to caregivers are sections on potential triggers of psychotic episodes and what caregivers can do about PD psychosis.
Medications To Help Treat Parkinsons Disease Psychosis
Your doctor might consider prescribing an antipsychotic drug if reducing your PD medication doesnt help manage this side effect.
Antipsychotic drugs should be used with extreme caution in people with PD. They may cause serious side effects and can even make hallucinations and delusions worse.
Common antipsychotic drugs like olanzapine might improve hallucinations, but they often result in worsening PD motor symptoms.
Clozapine and quetiapine are two other antipsychotic drugs that doctors often prescribe at low doses to treat PD psychosis. However, there are concerns about their safety and effectiveness.
In 2016, the approved the first medication specifically for use in PD psychosis: pimavanserin .
In clinical studies , pimavanserin was shown to decrease the frequency and severity of hallucinations and delusions without worsening the primary motor symptoms of PD.
The medication shouldnt be used in people with dementia-related psychosis due to an increased risk of death.
Psychosis symptoms caused by delirium may improve once the underlying condition is treated.
There are several reasons someone with PD might experience delusions or hallucinations.
What Is Lewy Body Dementia
Lewy body dementia , is a common form of dementia combining Alzheimers-like cognitive symptoms and Parkinsons-like motor issues. A neurodegenerative disease, it is the second most prevalent type of dementia after Alzheimers disease. Combining cognitive symptoms similar to Alzheimers with the motor features of Parkinsons, LBD is estimated to affect 1.3 million people in the United States.
The diseases name refers to abnormal protein deposits that occur in the brain discovered by neurologist Dr. Frederic Lewy. These Lewy body inclusions are present in both Parkinsons disease and LBD. Lewy body dementia refers to both Dementia with Lewy Bodies and Parkinsons disease Dementia, which are pathologically similar.
Abnormal Posture And Gait
Patients with Parkinsons disease have a characteristic flexed posture. A slow shuffling gait is combined with reduced or absent arm swing and the hands are held in front of the body. Crossing boundaries such as doorways may be difficult and turning is often slow and awkward. Excessive trunk flexion brings the centre of gravity forward and the walking pace tends to accelerate as the feet try to keep up, termed a festinating gait . This increases the risk of falling, particularly since impairment of postural reflexes is another common feature.
Abu A. Qutubuddin, William Carne, in, 2021
Hallucinations According To The Duration Of The Disease
We found that the prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of the disease. Moreover, the duration of Parkinson’s disease was an independent predictor of visual hallucinations in the multivariate analysis. Other studies gave conflicting results on the relationship between hallucinations and disease duration. In a retrospective study of 100 patients, logistic regression analysis also showed an association between `psychosis’ and an increased duration of the disease . An association between the duration of the disease and the occurrence of hallucinations was also found by some investigators but not by others .
Table 1
Neurological And Ophthalmological Assessments
All participants were examined by a neurologist specialized in movement disorders to establish the clinical diagnosis of PD in PD patients and to exclude the presence of a neurodegenerative disorder in controls. To evaluate cognitive function, The Montreal Cognitive Assessment and CLOX1 were used. Furthermore, the neurologist interviewed each participant for the presence of VH using standardized questions on minor hallucinations and complex visual hallucinations, within the last six months. Questions on minor hallucinations included questions on visual illusions , presence hallucinations and passage hallucinations . In addition, questions on complex visual hallucinations included questions on hallucinations of objects, animals or persons and on the retainment or loss of insight. Furthermore, participants were asked to categorize the frequency in which they experienced VH into daily, weekly, monthly or never. While questioning the participants, the neurologist was also informed by the patients medical files. Presence of VH was defined as minor or complex visual hallucinations, occurring monthly or more frequently, in the last six months before inclusion.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
What Is Parkinsons Disease
Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
Delusions From Parkinsons Disease

Delusions affect only about 8 percent of people living with PD. Delusions can be more complex than hallucinations. They may be more difficult to treat.
Delusions often start as confusion that develops into clear ideas that arent based on reality. Examples of the types of delusions people with PD experience include:
- Jealousy or possessiveness. The person believes someone in their life is being unfaithful or disloyal.
- Persecutory. They believe that someone is out to get them or harm them in some way.
- Somatic. They believe they have an injury or other medical problem.
- Guilt. The person with PD has feelings of guilt not based in real behaviors or actions.
- Mixed delusions. They experience multiple types of delusions.
Paranoia, jealousy, and persecution are the most commonly reported delusions. They can pose a safety risk to caregivers and to the person with PD themselves.
PD isnt fatal, though complications from the disease can contribute to a shorter expected life span.
Dementia and other psychosis symptoms like hallucinations and delusions do contribute to increased hospitalizations and increased rates of death .
One study from 2010 found that people with PD who experienced delusions, hallucinations, or other psychosis symptoms were about 50 percent more likely to die early than those without these symptoms.
But early prevention of the development of psychosis symptoms may help increase life expectancy in people with PD.
