What Are Movement Disorders
Movement disorders are a group of neurological disorders that cause abnormal movements. These movements may be voluntary or involuntary, and they may faster or slower than typical movements.
Epilepsy is one of the more well-known movement disorders. Epilepsy is a neurological disorder that causes seizures due to abnormal brain activity. Other movement disorders include Tourette syndrome, Parkinson’s disease, restless leg syndrome, and many others.
Have You Come Across Advice That Those With Parkinsons Should Avoid Too Much Refined Sugar Or Perhaps Youre Aware Of New Research Linking Diabetes And The Condition We Go Behind The Headlines To Find Out What Is Actually Going On
Over the last decade, a war on sugar has started. In March 2016 the government announced that a tax on sugary soft drinks would be introduced in the UK from 2018. At the same time, weve seen a gradual increase in messaging that healthy eating, particularly limiting your intake of sugar, is essential for a healthy body.
The main aim of this war is to curb a growing obesity pandemic. And while its too early to draw any conclusions about these initiatives on the patterns of obesity in the UK, studies have suggested that simply reducing the sugar content of sweetened beverages by 40% over five years could result in roughly half a million fewer obese adults. As our collective national waistline shrinks, the hope is we will also see a reduction in a range of health conditions from heart problems to cancer, diabetes to osteoarthritis.
Tips For Living With Hallucinations
It is important for people with PD to talk about hallucinations with their family and care team, because they are manageable and can be troublesome if not treated. Discuss all possible symptoms with your doctor, no matter how minor, rare or bizarre you may think they are.
- Good lighting and stimulating activities in the evening can help keep hallucinations at bay.
- While a hallucination is occurring, caregivers can help their loved one by reassuring them that they will be safe and validating their partners experience. For example, say, Ill take the cat outside instead of arguing that there is no cat.
What Is The Link Between Paraquat And Parkinsons Disease
What Is the Link Between Paraquat and Parkinsons Disease? Diseases affect a living beings structure and function. For example, macular degeneration causes your retina to degenerate or causes blood vessel growth beneath the retina. These developments cause blurred vision and may result in loss of vision. The structural impact of the disease alters the affected body parts ability to function typically.
Infectious diseases can spread from person to person or animal to person. COVID-19 is an infectious disease. Dietary deficiencies cause deficiency diseases. Beriberi is a disease caused by a lack of vitamin B1. Hereditary diseases like cystic fibrosis are passed down from your ancestors or caused by mutated genes. Physiological diseases affect the way a person functions. Parkinsons disease is a physiological disease. People with Parkinsons disease may be curious about the connection between paraquat and Parkinsons. Read on to learn about Parkinsons, paraquat, and your legal options if you have Parkinsons.
Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed
In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half of the patients were described as unable to make any decisions in the last month of life. 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
The 5 Stages Of Parkinsons Disease
Getting older is underrated by most. Its a joyful experience to sit back, relax and watch the people in your life grow up, have kids of their own and flourish. Age can be a beautiful thing, even as our bodies begin to slow down. We spoke with David Shprecher, DO, movement disorders director at Banner Sun Health Research Instituteabout a well-known illness which afflicts as many as 2% of people older than 65, Parkinsons Disease.
The Use Of Levodopa And Peripheral Neuropathy
There are reports in the literature that levodopa use may increase the risk of peripheral neuropathy, although other studies suggest that this is not the case. There are studies that demonstrate for example, that cumulative Levodopa exposure correlates to prevalence of PN in people with PD. Other studies however, demonstrate no difference in the prevalence of PN whether the person was treated with Levodopa or not, suggesting that Levodopa treatment does not play a role in development of PN.
Another area of research that emerges from the literature is the potential role of Vitamin B12 deficiency in the development of PN in those with PD. Some studies suggest that Vitamin B12 deficiency is a more common cause of PN among those with PD than those with PN who do not have PD.
There is also research that suggests that levodopa treatment may contribute to PN through impairment of Vitamin B12 metabolism, leading to Vitamin B12 deficiency. Taking COMT inhibitors such as Entacapone may protect against this complication.
Regardless, if PN is diagnosed in anyone, whether they have PD or not, and whether they take Levodopa or not, Vitamin B12 and various other markers of Vitamin B12 metabolism should be tested. If Vitamin B12 levels are low or even low-normal, a person should take Vitamin B12 supplementation, which may help with the symptoms of PN. Other causes of PN, many of which can be checked with various blood tests, should be investigated as well.
No.
So, what is the controversy?
How Do You Die Of Parkinson’s Disease
Asked by Deb Nigra 431 votes
A
Parkinsons disease, a chronic, progressive movement disorder characterized by tremors and stiffness, is not considered a fatal disease in and of itself, though it may reduce life expectancy by a modest amount. It is often said that people die with Parkinsons rather than of the disease.
People who are healthy when diagnosed will generally live about as long as other people in their age cohort, said James Beck, the vice president for scientific affairs at the Parkinsons Disease Foundation, which is involved in research, education and advocacy. It is not a death sentence.
Since Parkinsons generally affects people later in life patients are typically given a diagnosis in their 60s patients often die of unrelated age-related diseases like cancer, heart disease or stroke. But the most common cause of death in those with Parkinsons is pneumonia, because the disease impairs patients ability to swallow, putting them at risk for inhaling or aspirating food or liquids into their lungs, leading to aspiration pneumonia.
Do you have a health question? Submit your question to Ask Well.
Should You Put Your Dog Down If Their Parkinsons Is Bad
I cannot answer that question for you. Your decision to euthanize a dog with Parkinsons disease is highly personal. If your dogs quality of life is truly poor, with no independence at all, the kinder thing may be to put them down.
Its a decision we never want to make, but sometimes it really is the best thing for them.
Consult your veterinarian for advice on how long your dog can expect to remain mobile and when euthanasia may be the sole solution.
Can Seizures Be Managed In People With Dementia
There is good news. There are medications that are effective at reducing, and hopefully stopping, epileptic seizures.
If you think that you, or someone you know with dementia may be having epileptic seizures you should tell a doctor. They might want to perform some extra tests, and may want to start some extra medications to treat this problem.
What we dont know yet is whether starting treatment for epilepsy might help to slow down dementia and whether it might help keep peoples memory function better for longer.
We have learned so much about the brain but there is still so much to discover.
Support dementia research
Alzheimers Society is working tirelessly to challenge perceptions, fund research and improve care and support. We rely on your donations. Lets take on dementia together.
The Use Of Levodopa And Peripheral Neuropathy
There are reports in the literature that levodopa use may increase the risk of peripheral neuropathy, although other studies suggest that this is not the case. There are studies that demonstrate for example, that cumulative Levodopa exposure correlates to prevalence of PN in people with PD. Other studies however, demonstrate no difference in the prevalence of PN whether the person was treated with Levodopa or not, suggesting that Levodopa treatment does not play a role in development of PN.
How Is Psp Different From Parkinsons Disease
Peripheral Neuropathy And Parkinsons Disease
Why Do People With Dementia Develop Seizures
Ultimately, anything that changes the structure of the brain can cause seizures.
This happens for some people after a stroke, a head injury, or with a brain infection like meningitis. A similar problem is happening in the brain in dementia. As cells in the brain die and the brain shrinks this can lead to epilepsy.
In addition, we know that two proteins that build up in the brain of people with Alzheimers disease amyloid and tau affect how the brains nerve cells communicate with each other.
Sometimes these nerve cells can become hyper-excitable, meaning they can behave uncontrollably, causing epileptic seizures.
What Symptoms Can Be Expected In Advanced Pd
- Pain 86%
- Shortness of breath 54%
- Problems in swallowing 40%14
In an analysis of 339 death certificates and medical notes in the UK, pneumonia was found to be a terminal event in 45%.13
Caregiver distress with choking and the risk of choking to death is also mentioned in a separate study in to experiences regarding all stages of PD.4
In a survey of symptoms and their association with quality of life, in those patients with advanced disease, uncontrolled pain, anxiety and hallucinations were significantly associated with poor quality of life.9
Seizures are also noted in a description of the last phase of Parkinsonian syndromes,15 and in retrospective studies of PD patients overall.16,17
Potential Therapeutic Implications For Non
What Are The Symptoms Of Parkinson Disease
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41It reduces the time in motor off periods in advanced PD and quality of life.42There is evidence of effective treatment up until death from within a case series.43
Relationship Between Disrupted Neuronal Connectivity And Epileptic Seizures
Epilepsy is considered a disease of network dysfunction.47,48 At a microscopic level, both simple and complex partial seizures involve disruptions in the excitatory interactions between cerebral cortex pyramidal cells.49 From a neurophysiology view, the EEG-graphic representation of an epileptic event is characterized by the paroxysmal onset of hyper-synchronized sharp waves disrupting the neuronal background activity. This activity is often multifocal, reflecting a broader network dysfunction.50,51 Moreover, TMS studies demonstrate similar neurophysiologic features between epilepsy and PD characterized by a state of increased cortical excitability as indicated by reduced intra-cortical inhibition and increased intra-cortical facilitation observed in both patient populations.25,5255 As mentioned before, in PD, cortical neurons innervating the basal ganglia become hyperexcitable, possibly as a compensatory mechanism following the incremental rise in the output threshold of striatal dopaminergic neurons. As such, it would not be surprising if this putatively maladaptive phenomenon may eventually lead to the generation of epileptiform activity. While epidemiologically, epilepsy-increased comorbidity in patients with PD remains questioned,13,56 our group published the largest case series of patients with PD with concomitant epilepsy57 raising the possibility that epileptic activity in these patients may indeed be under-diagnosed and under-recognized.
Parkinsonism Falls And Fracture Risk
All forms of parkinsonism, both PD and DIP, have implications for bone health. A 2014 meta-analysis on PD and fracture risk concludes that PD increases the risk of fracture.4
Given that the symptoms of parkinsonism affect balance, motor skills, gait, and the bodys ability to control movement, it is no surprise that people with PD are more likely to experience a fall than people without PD. Here is an excerpt from a 2016 study comparing the incidence of falls and fracture in PD patients:
It is estimated that 60.5% of patients with PD experience at least one fall and 39% have recurrent falls. The high frequency of falls consequently contributes to the increased risk for fractures in PD patients, which has been estimated to be approximately two times the risk in healthy controls. It has been estimated that 76% of falls in PD patients require health care services and 33% result in fractures. Falls and fractures may result in a series of unfavorable outcomes, such as disabilities and death. Furthermore, among PD patients with fractures, the mortality rate is approximately 10.6%.5
All too often, doctors prescribe these drugs without appropriate consideration of this risk. This excerpt from a study on DIP clarifies the danger of accepting a prescription of an unnecessary or inappropriate prescription drug:
Shockingly, the drugs that cause DIP are still being prescribed. This yet one more example further proving that the FDAs drug approval process is useless.
Synopsis
What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
The Relationship Between Parkinsons Disease And Sleep
Its unclear whether poor sleep causes parkinsonian symptoms to worsen or whether worsening parkinsonian symptoms cause poor sleep. In many cases its likely a case of bidirectionality, with each one exacerbating the other.
Fragmented sleep and sleep deprivation appear to leave the brain more vulnerable to oxidative stress, which has been tied to the development of Parkinsons disease. Parkinsons disease is not usually diagnosed until individuals have developed sufficient motor symptoms, by which time a significant portion of brain cells have already been damaged. If poor sleep quality or having sleep disorders foreshadows the development of parkinsonian symptoms, these could be useful in early diagnosis of the disease.
More research is needed to clarify the multifaceted relationship between Parkinsons disease and sleep. A better understanding of this connection may offer medical experts the unique opportunity to screen at-risk individuals and perhaps delay the onset of the disease.
Peripheral Neuropathy And Parkinsons Disease
A number of studies have tried to determine if PN is more common among people with PD as opposed to people without PD. PN is a relatively common condition in the general population, which makes it difficult to ascertain whether or not it is even more common among people with PD.
The available studies have varying results and are difficult to compare with each other as they:
- Include different types of populations of people with PD
- Assess peripheral neuropathy differently
- Assess for causes of peripheral neuropathy differently
A recent review looked at all the available data and determined that large fiber neuropathy was present in 16% of patients with PD, about double the prevalence of this condition in the general population. Skin biopsy-proven small fiber neuropathy was present in over 50% of people with PD, although this result was based on a small sample of patients.
How Could Cbd Oil Help With Parkinsons
While doctors havent been using CBD oil for Parkinsons disease long-term, and research into the benefits of CBD for this condition only began a few decades ago, current findings are very exciting. Studies suggest that CBD may have some positive effects on certain symptoms of Parkinsons disease, especially when it comes to anxiety, depression, and sleep difficulties.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
What Are Delusions
Delusions are illogical, irrational, dysfunctional views or persistent thoughts that are not based in reality. They are not deliberate and are very real to the person with PD. People with delusions who feel threatened may become argumentative, aggressive, agitated or unsafe.
- Delusions are less common in PD than visualhallucinations. They affect about eight percent of people with PD.
- Compared to hallucinations, delusions tend to be more complicated, present a greater risk for behavioral disturbances and safety concerns, are typically more difficult to treat and represent a more obvious deterioration or decline in ones condition.
- Delusions can begin as generalized confusion at night. Over time, confusion can develop into clear delusions and behavioral disturbances during the day.
- All forms of delusions can be seen with PD, although delusions of jealousy and persecution are most widely reported and represent a greater challenge for treatment. These delusions can lead to aggression, which can pose a serious safety risk to the person with PD, family members and caregivers.
- Paranoia can lead to medication noncompliance a person refusing to take medications, believing they are poisonous or deadly.
- Delusions can be associated with dementia. As a result, people with delusionsare often confused and extremely difficult to manage. In these cases, many caregivers require outside assistance.
How To Avoid Dip

The incidence rate of DIP has proved difficult to assess, due to the prevalence of misdiagnosis as PD. Older people and women are at higher risk of DIP, and genetic factors may also play a role.2
The only way to develop DIP is by taking a prescription drug that impacts the brains dopamine system. If you dont take those drugs, you cannot develop it.
Unfortunately, in some cases, DIP is misdiagnosed as PD. Researchers discovered that 6.8% of patients diagnosed with PD were later reclassified as having DIP.3 This mistake is particularly harmful since doctors may prescribe drugs to manage PD symptoms instead of stopping the drug thats causing DIP.
Discontinuing the responsible drug most often ends DIP. However, in some cases, the symptoms persist. In others, the parkinsonism continues to worsen along a track consistent with PD. Researchers have postulated that in these cases the drugs unmasked PD, which may have otherwise gone unexpressed.
Synopsis
If you dont take a prescription drug that causes DIP, then you cannot develop it. People experiencing DIP can usually end it by discontinuing the medication that caused it, but for some people, the symptoms persist or worsen.
Whats The Connection Between Paraquat And Parkinsons
Paraquat is a toxic herbicide, and people exposed to paraquat can develop multiple health issues, such as pain, vomiting, and diarrhea. Paraquat exposure can lower your blood pressure, and ingesting even small amounts can cause severe health problems, including kidney failure and heart failure.
Ingesting large quantities can trigger a coma, cause muscle weakness, produce respiratory issues, or cause seizures. The U.S. Centers for Disease Control and Prevention reports that ingesting large amounts of paraquat is typically fatal. Studies indicate paraquat exposure can cause Parkinsons. These studies provide legal grounds for lawsuits against paraquat producers when exposure to paraquats linked to Parkinsons disease.
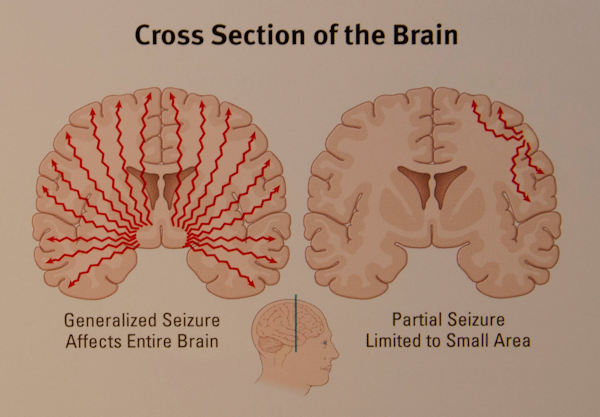
There Are Two Common Types Of Epileptic Seizures:
Generalised tonic-clonic seizures
Most of us are familiar with the kind of epileptic seizures we see on TV or in films. People become unresponsive, they fall to the ground, become stiff and their whole-body shakes in a convulsion.
Generalised tonic-clonic seizures are hard to miss. But this is not what most epileptic seizures look like.
Focal onset seizures
Most epileptic seizures in people with dementia are known as focal onset seizures. These can involve brief periods of increased amnesia or unresponsiveness. We see involuntary repeating movements, often of the hands and arms, or of the face .
Understandably, the latter are more easily missed, especially as the person affected will often quickly be back to normal afterwards..
What Is The Link Between Seizures And Dementiablog
There are some symptoms of dementia that are more commonly known, such as memory loss. Seizures are a less common symptom of dementia that are not as understood. Hear from one of our dementia researchers who has been studying seizures in people with the condition.
How common are epileptic seizures in dementia? Who is most at risk of having them? What do these seizures look like? What effect do they have on how someones memory changes over time?
These are the questions that I have been researching since starting my PhD in 2016.I’m astudent funded by Alzheimers Society as part of the University of Exeter doctoral training centre.
When To See A Doctor
Seek immediate medical help if any of the following occurs:
- The seizure lasts more than five minutes
- Breathing or consciousness doesn’t return after the seizure stops
- A second seizure follows immediately
- You have a high fever
- You’re experiencing heat exhaustion
- You’ve injured yourself during the seizure
- If you experience a seizure for the first time, seek medical advice.
Can Dogs Get Parkinsons Disease
In some ways, dogs and people are similar.
Both express love, have a playful side, and remain fiercely loyal to their families.
Unfortunately, just like people, dogs also get Parkinsons disease.
Parkinsons is a neurological condition that attacks the motor system and typically leads to mental incapacity in the form of dementia.
If your dog has it, its important to get a diagnosis as soon as possible so that you can slow down the progress of the disease.
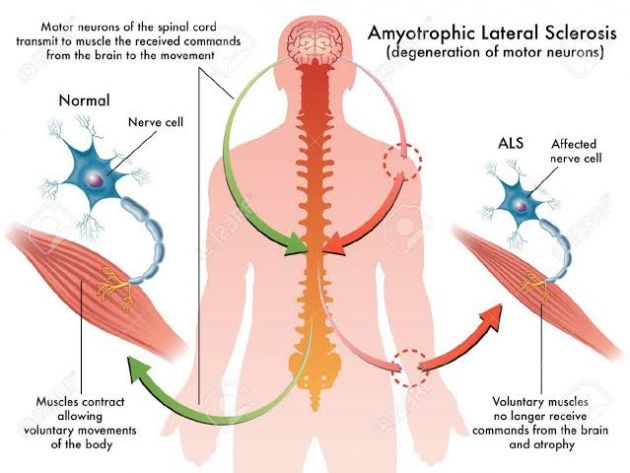
What Causes Parkinson Disease
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts don’t know what triggers the development of Parkinson disease most of the time. Early onset Parkinson disease is often inherited and is the result of certain gene defects.
A Search For Sharpness
But it is the angles and sharpness of brain waves that could hold the key to detecting Parkinsons, according to the new studys findings, which appear in the journal
While working on his doctorate at the University of California, San Diego, fellow study author Scott Cole, Ph.D., realized a potential link between the disease and sharp brain waves.
Using EEG readings taken from 15 Parkinsons patients and 16 healthy individuals, the team honed in on the unfiltered waves.
The raw signals go up and down like sine waves but with more asymmetry, explains Swann, adding, The steepness the slant turns out to be important in Parkinsons patients.
Indeed, the team noticed that Parkinsons patients who were not taking medication had a sharper peak at the top of their brain wave, compared with the bottom.
Finding that a noninvasive method such as an EEG could be a promising diagnostic tool may have important consequences for the future of the disease. The team is hoping that doctors and researchers can use the test to track changes related to Parkinsons in the brain over the years.
We dont know yet whether this approach will be better, but it could provide easily obtained brain measurements that would be helpful and possibly used in tandem with clinical observations and other EEG measurements, notes Swann.
