Causes Of Parkinson’s Disease
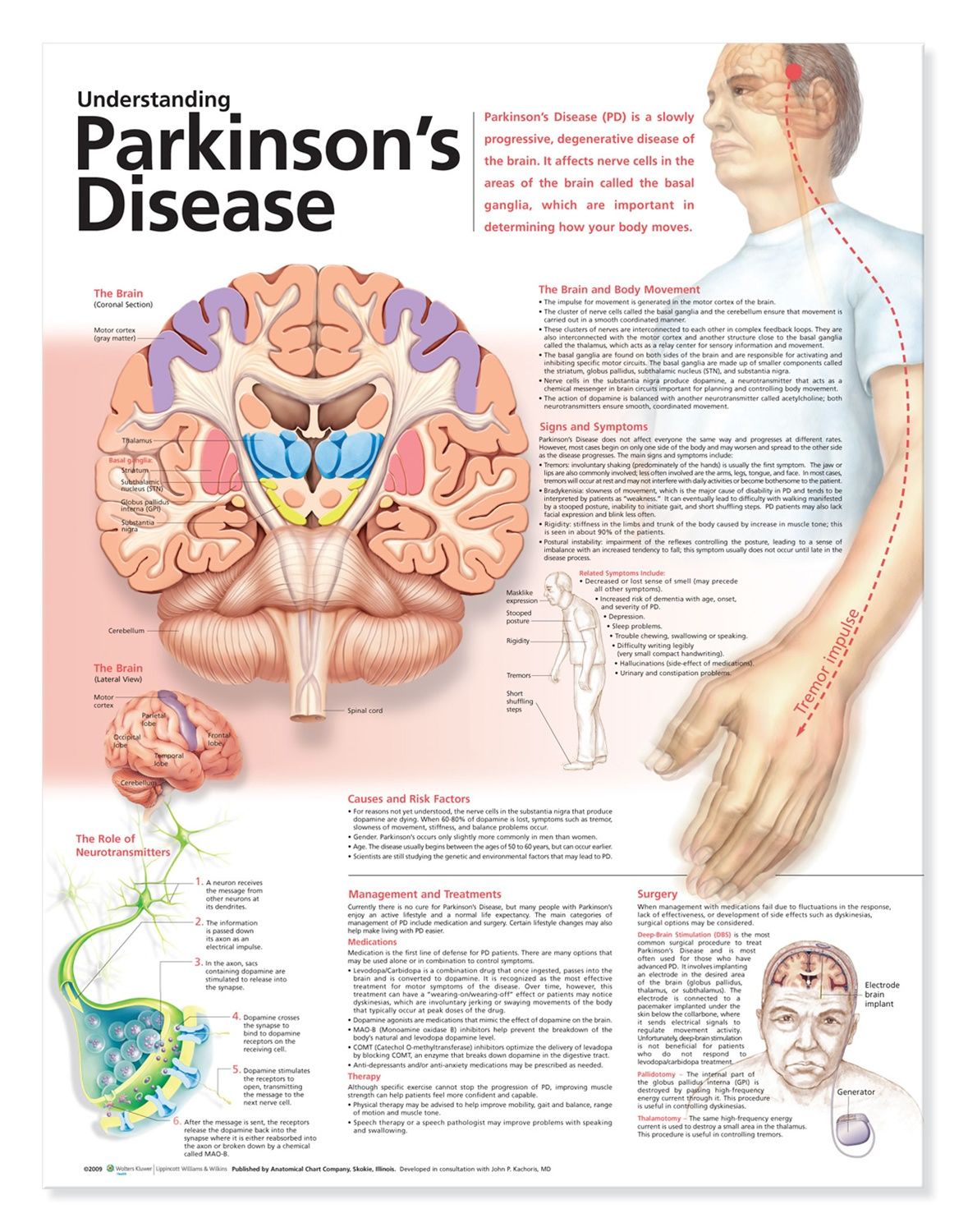
Parkinson’s disease is caused by a loss of nerve cells in part of the brain called the substantia nigra. This leads to a reduction in a chemical called dopamine in the brain.
Dopamine plays a vital role in regulating the movement of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinson’s disease.
Exactly what causes the loss of nerve cells is unclear. Most experts think that a combination of genetic and environmental factors is responsible.
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinsons disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinsons disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Approaches To Pain Assessment
When assessing pain in patients with PD, using a validated pain scale that targets symptoms specific to PD whenever possible will more accurately categorize pain type. The first pain tool designed specifically for patients with PD is the Kings PD Pain Scale .4,12 This scale has 14 questions that measure severity and frequency of different types of pain specific to PD. A complementary patient screening tool, the Kings College PD Pain Questionnaire , is designed for assessing whether or not specific pain types are present. All questions on the KPPQ correspond with a specific question on the KPPS. Screening patients with the KPPQ can facilitate identifying pain types that correspond to the KPPS assessment tool.
If unable to assess pain with scales specific to PD, validated general pain scales, such as the Likert scale, can be utilized to determine quality and severity of any type of pain.18 Using PD-specific pain scales may better characterize a patients pain symptoms, however, which may lead to more targeted treatment options.
Read Also: What Essential Oils Are Good For Parkinson’s Disease
Lower Back Pain And Parkinsons Disease
Lower back pain is an extremely common problem in the general population, as well as for people with Parkinsons disease . It tends to make moving more difficult, adding to the challenges of PD. Tim Nordahl, PT, DPT, a physical therapist at Boston University gave an excellent presentation as part of APDAs Lets Keep Moving Webinar Series. Because this is such a prevalent issue, and because there are things you can do to help alleviate your back pain, I wanted to summarize and highlight this important topic.
Natural Remedies And Treatments For Parkinsons Disease That Get Powerful Results
To successfully treat the symptoms of Parkinsons, andeven reverse this disorder, there are 4 things you must do
a) Increase your natural dopamine levels
b) Detox your body of all heavy metals andpollutants
c) Reduce all inflammation in the body,especially the brain
d) Repair the neuro pathways
These 10 natural treatments and remedies do all four. Solets not waste any more time then. Here they are in order of importance
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Q Which Pharmacotherapies Are Best For Treating Pain In Pd
Dr. Fleisher: The first step is to make sure that Parkinsons medications are optimized. For example, dystonic or musculoskeletal pain may be caused by Parkinsons motor symptoms when dopamine levels are too low. If the patient is able to keep a pain diary, it may show a clear pattern of pain occurring the hour before each dose or before specific doses, suggesting the need to either increase the dosage preceding the pain episode, increase the frequency of medication dosing, or use adjunctive dopaminergic therapies to achieve more steady dopamine levels throughout the day.
In addition, optimal management of comorbidities that may contribute to pain is needed. The choice of pain medication depends on the pain type.
The first lines of treatment for musculoskeletal pain can be heat and cold packs and nonsteroidal anti-inflammatory drugs alone or in combination with acetaminophen.
For dystonic pain, adjustment of dopaminergic medications is particularly critical however, if dystonia consistently occurs in 1 particular body part, botulinum toxin injections also can be helpful. The goal of botulinum toxin injection is to weaken the muscle enough to stop the abnormal contractions and twisting, but the patient may lose function in the body part as a result . Thus, patient counseling is important to manage expectations.
Pathophysiological Pathways Of Pain In Pd
The origin of pain in PD remains poorly understood. At times, it appears as dystonia when the dopaminergic effects wear off. The pathophysiological mechanisms behind this phenomenon are most probable by which dopamine, in the network with other monoamines such as noradrenaline and 5-hydroxytryptamine , interacts through inhibitory and excitatory pathways. Abnormalities in descending pathways affect central pain processing. In addition, clinically registered neuropathic pain and other muscular pain sensations are described by PD patients. This has led to the exploration of pathways other than those secondary to rigidity, tremor, or any other motor manifestations of the disease, with abnormal nociception processing in PD patients suffering from pain as the most likely suspect. The basal ganglia process somatosensory information in different ways, and increased subjective pain sensitivity with lower electrical and heat pain thresholds has been reported in PD patients. This abnormal processing also comprises PD-related disorders such as multiple system atrophy, which exhibits almost the same prevalence of pain as PD.
The pathophysiological basis of sensory disturbances in PD, the so-called pain matrix with information from different loci, processed in the BG.
Abbreviations: PD, Parkinsons disease BG, basal ganglia GPe, globus pallidus externa, GPi, globus pallidus interna STN, subthalamic nucleus.
You May Like: Is Parkinson’s Disease Fatal
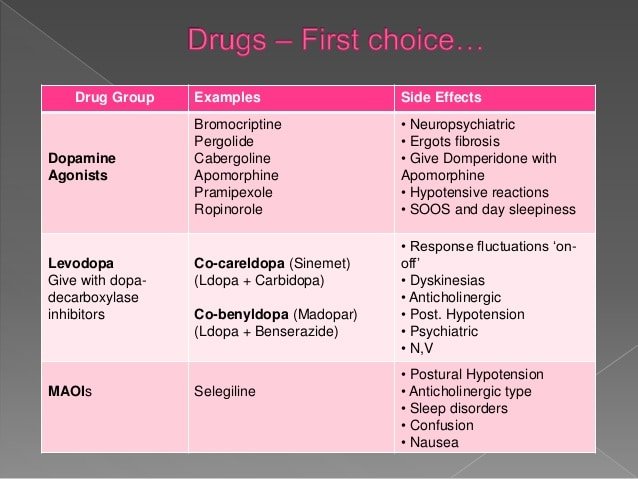
Medical Treatment For Parkinson’s Disease
Parkinson’s disease cannot be cured, though taking the medicines timely as prescribed by the doctor can control your symptoms, often dramatically. The doctor may suggest lifestyle changes, and exercises and physical therapy that focuses on balance and stretching.
Based on the severity of the patients condition the doctor may also suggest surgery.
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
You May Like: What Color Is The Ribbon For Parkinson’s
Q What Role Does Exercise Play In Pain Management In Pd
Dr. Fleisher: Exercise and physical therapy can be tremendously helpful in managing pain in PD, in addition to being important for overall disease management.4,8 Evidence suggests that exercise is the best option we have to alter the course of PD, and it has been shown to promote neuroplasticity and neurorestoration in PD.9,10 In addition, research suggests that exercise can activate both dopaminergic and non-dopaminergic inhibitory pain pathways, which may help to modulate the experience of pain in PD.10
Good exercise options include walking, swimming, dancing, and using a recumbent bike. In particular, forms of dance with smooth movements and those that encourage bigger steps appear to be especially beneficial in helping retrain the brain that the shuffling gait of PD is not the norm. Incredible work has come out of the Mark Morris Dance Company, in New York City, which has started a Dance for PD class that has spread throughout the country. In addition, yoga and tai chi can help with balance and core strength, which are critical for people with PD.
Importantly, there doesnt appear to be an upper limit for the benefits of exercise on the disease. I encourage patients to aim for at least 30 to 45 minutes a day at least 3 to 4 days a week. Patients who are sedentary should start with 5 minutes per day for a week, and then increase the duration each week.
Pain Presentation And Assessment In Pd
Most epidemiological data are based on questionnaires which were not specifically validated for PD patients so that results have to be interpreted with caution. The Kings Parkinsons disease pain scale is to date the only questionnaire that is specifically calibrated and validated for PD and is highly recommended to qualitatively and quantitatively assess pain and to ascribe the pain pathophysiologically. The scale contains seven different pain domains comprising musculoskeletal pain, chronic pain , fluctuation-related pain, nocturnal pain, oro-facial pain, discolouration or oedema/swelling and radicular pain as well as 14 sub-categories . This assessment tool is based on the pain classification according to Ford but also considers pain types of other classifications such as motor fluctuations or visceral pain .
In addition, there are some specific pain syndromes in PD which have to be kept in mind, including the so-called coat-hanger pain that occurs in cases of pronounced orthostatic dysregulation and although it is more frequent in multisystem atrophy it can occur also in PD and is often associated with strong headache and neck pain . Furthermore, pain due to constipation which is frequent in PD can cause abdominal pain.
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinsons disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
Q What Is The Role Of Depression In The Pain Experience In Pd
Dr. Fleisher: Depression is one of the most overlooked symptoms of PD, and it can affect over 30% of people with the disease at some point in their illness.5 I think there is a misconception that depression results from an adjustment disorder following diagnosis. While that may be partially true, patients with PD have alterations in various neurotransmittersincluding serotonin and norepinephrine in addition to dopaminethat predispose them to depression.6,7
Depression is the primary factor related to quality of life in PD and is an independent risk factor for medication nonadherence. A physician could prescribe the most comprehensive regimen to control Parkinsons symptoms, including pain, but if depression symptoms are not being addressed simultaneously, the likelihood that that person is going to take that regimen is pretty minimal.
Given the link between depression and chronic pain, patients who are depressed should be screened for chronic pain and vice versa. In my practice, we screen every patient with the Unified Parkinsons Disease rating scale , which has both a patient-reported subjective component that includes questions about depression, pain, and altered sensation, as well as an objective component that includes a physical examination and questions about potential medication adverse effects . The patient fills out the subjective component every single time they come to the office.
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Sensory Profiling And The Potential For Mechanism
Since psychophysical testing offers the opportunity to explore the functionality of an individuals pain system under controlled settings, a comprehensive assessment of various pain processing and modulatory pathways for use as a surrogate measure of the mechanisms driving the development of persistent pain in a given population/patient cohort is possible. For example CPM deficiencies in patients with neuropathic pain can be targeted by manipulation of central noradrenergic and serotonergic transmission, where the pain-inhibiting impact of Tapentadol potentiates impaired CPM in persistent pain patients in a manner that back translates to animal studies,,. Psychophysical testing can also be used to predict analgesic treatment efficacy.
In people with PD, sensory profiling through psychophysical testing has been applied in order to provide insight of the underlying mechanisms of persistent pain. Thereafter, guidance for personalised pain medicine through mechanism-based treatments is a key goal for many chronic pain types,,,. However, a frustratingly disparate range of psychophysical trials exists in the literature for the PD patient cohort, where significant differences in the type of pain considered and methodologies employed leads to incomplete conclusions, as discussed below.
Who Is Prone To Parkinson’s Disease
Some people are more to Parkinsons disease than others. They include:
- People who are of advanced age
- Males are more likely to get Parkinsons disease than females
- People with a family history of Parkinsons disease
- Postmenopausal women who have very low levels of oestrogen
- Women who have undergone hysterectomies
- People who suffer from vitamin B deficiency
- People who have suffered from head trauma
- People who are frequently exposed to environmental toxins such as a pesticide or herbicide
Don’t Miss: Life Expectancy With Parkinson’s
Naturalremedy For Parkinsons #7 Omega
Animal based omega-3 fatty acids are a powerful weapon inthe fight against Parkinsons disease. One of the main fatty acids, DHA, is oneof the essential building blocks for the human brain. Half of your brain andeyes are made up of fat and a large proportion of this is DHA fat.
Omega-3 fatty acids have the unique ability to cross theblood-brain barrier, something most conventional drugs cannot do. They helpincrease dopamine levels and reduce neuroinflammation in the brain, while atthe same time, stimulating neuron growth. So basically, EPA and DHA help preventbrain cell damage and keep the nervous system in tip top working order! 4
Best sources of animal based omega-3s are either fishoil, cod liver oil or krill oil. High strength krill oil is the preferred option as thiscontains a substance called Astaxanthin. Astaxanthin is a potent brain food nutrientthat has been shown to prevent neurodegeneration and inflammation of the brain.For dosages, take AT LEAST the highest recommended amount listed on the bottle the same goes with fish oil or cod liver oil. You cant overdose on thesesupplements so theres nothing to be concerned about. In fact, the more omega-3syou can get into you the better the results!
In addition to this, try and eat some cold water fattyfish such as salmon, tuna, mackerel, sardines or herring 3-4 times a week foran extra supply of DHA and EPA.
What Is Parkinson’s Disease
Parkinson’s disease is a neurodegenerative disorder that affects the way you move. It occurs when there is a problem with the nerve cells in the brain that produce an important chemical called dopamine, which is responsible for motor function. As dopamine levels drop it leads to progressive deterioration of motor function in the person. Early signs of Parkinsons disease include tremors in the hands, rigidity or stiffness in the body, difficulty while walking. The muscles of the person suffering from Parkinsons disease gradually become weaker with time.
Don’t Miss: Is Parkinson’s Terminal
How Is Pain Diagnosed Assessed And Treated
Diagnosing and treating pain in people with Parkinsons can be difficult and often, common ways of reducing pain, such taking painkillers or doing regular, gentle exercise may not help.
Usually, your doctor or Parkinsons nurse specialist will be able to help you to manage the more common types of pain, such as shoulder pain and headaches. Certain other types of pain, however, such as pain caused by involuntary movements or burning mouth, may need the help of your Parkinsons specialist.
Completing a Kings Parkinsons Disease Pain Questionnaire and showing it to your heath-care professional will help them to understand the pain you are suffering from1. Completing the 24-hour Hauser2 diary, a home diary designed to assess your motor symptoms, over the same period of time, would further help your doctor or Parkinsons nurse to better understand the pain you are experiencing and to treat it more quickly.
To ensure Parkinsons pain is assessed and diagnosed efficiently, a specific scale has been designed. Kings Parkinsons Pain Scale 1 is a validated scale which covers the common types of Parkinsons related pain. Your Parkinsons specialist might use this scale to help understand the type of Parkinsons pain you have even better and assess what needs to be done to help you further.
References:
Complementary And Alternative Medicine
In addition to pharmacologic and interventional treatments, several complementary and alternative therapies have also been investigated for alleviating PD pain. The designation of alternative medicine is a bit of a misnomer as these treatments are typically used alongside traditional pharmacologic and surgical interventions. A number of studies have examined the benefits of complementary therapies, but there is a lack of large-scale, high-level research and results are mixed regarding their effectiveness. Fortunately, most complementary therapies are safe and well-tolerated, and current literature, though limited, does suggest a role for including these therapies as a component of a multimodal approach to pain treatment.
Finally, there has been some research into the use of cannabis for pain treatment in the setting of PD. In two small, open-label, observational trials in PD patients, cannabis was found to improve pain scores as well as significantly decrease heat and cold pain tolerance . The authors postulated that cannabis acts on PD pain via modulation of the peripheral and central pathways . While no adverse effects were found in these trials, unlike with other complimentary therapies, cannabis use carries the risk of unpleasant side effects. Patients must be aware of the potential for paranoia, delusions, breathing problems, increased heart rate, and nausea. These side effects are typically dose related with incidence increasing with higher doses.
Read Also: Cardinal Features Of Parkinson’s
