Study Design In Brief
We retrospectively identified all patients with coexisting PD and CSM who underwent cervical decompression at Cleveland Clinic between June 2009 and December 2014 and then matched them to controls with CSM alone who underwent cervical decompression over the same period by the same team of spine surgeons . Matching was done on the basis of age, gender, American Society of Anesthesiologists classification, preoperative modified Japanese Orthopaedic Association score and operative parameters.
The primary outcome measure was postoperative improvement in mJOA score at patients last follow-up visit. The mJOA scale ranges from 0 to 18, with lower scores indicating greater neurologic disability. Two points was considered the minimum clinically important difference. Additionally, scores on the Nurick scale were collected to measure ambulatory status, with greater scores indicating greater impairment.
In a secondary QOL analysis, outcomes included QOL improvement as measured by the EuroQol 5 dimensions questionnaire , the Pain Disability Questionnaire and the Patient Health Questionnaire 9 . These measures were prospectively collected before and after surgery.
Simple and multivariable linear and logistic regression analyses were used to assess the impact of PD on primary and secondary outcomes.
Outcomes And Radiological Measurements
Data for age, gender, body mass index , disease duration from diagnosis of compression fracture to that of burst fracture and/or appearance of neurological symptoms, surgical procedures, and postoperative complications were acquired from medical charts. In patients with PD, the Hoehn & Yahr stage before surgery and at follow-up was assessed by senior neurologists. Clinical symptoms, low back pain, radicular leg pain, and cauda equine sign were also stratified based on cleft formation. Radicular leg pain was defined as lower extremity pain consistent with a neurological dominant region. Cauda equina syndrome was diagnosed based on symptoms of neurogenic intermittent claudication or motor and/or sensory disturbance, including bladder dysfunction. The Japanese Orthopaedic Association score for neurological status was obtained before surgery and at follow-up, with all neurological evaluations performed by senior spine surgeons. Neurological improvement rate at follow-up was calculated using the following formula: ×100/. Plain standing radiographs were used to identify other vertebral collapses, the type of vertebral collapse, lumbar lordosis and local lumbar lordosis before surgery and at follow-up.
Figure 3
How Is Psp Different From Parkinsons Disease
PSP is often misdiagnosed as Parkinsons disease, especially early in the disorder, as they share many symptoms, including stiffness, movement difficulties, clumsiness, bradykinesia , and rigidity of muscles. The onset of both diseases is in late middle age. However, PSP progresses more rapidly than Parkinsons disease.
- People with PSP usually stand exceptionally straight or occasionally tilt their heads backward . This is termed axial rigidity. Those with Parkinsons disease usually bend forward.
- Problems with speech and swallowing are much more common and severe in PSP than in Parkinsons disease and tend to show up earlier in the disease.
- Eye movements are abnormal in PSP but close to normal in Parkinsons disease.
- Tremor is rare in PSP but very common in individuals with Parkinsons disease.
Although individuals with Parkinsons disease markedly benefit from the drug levodopa, people with PSP respond minimally and only briefly to this drug.
People with PSP show accumulation of the protein tau in affected brain cells, whereas people with Parkinsons disease show accumulation of a different protein called alpha-synuclein.
Also Check: Patch For Parkinsons Disease
You May Like: Did Katharine Hepburn Have Parkinson’s Disease
Operative Procedure & Postoperative Course
Considering the patientâs degree of deformity and pain, we elected to perform revision surgery. Pedicle screws and rods were reinserted from the L1to S1 levels with iliac screws after performing a partial pedicle subtraction osteotomy at the L4 level with removal of the intervertebral discs at the level of L34 . The patientâs intraoperative and postoperative periods were uneventful, and she was able to walk with a straight back without any support a few days postoperatively. Follow-up X-rays obtainedapproximately 18 months after surgery showed significant improvement in her spinal parameters and kyphoscoliosis. Pre and postoperative surgical outcomes were measured with Modified Scoliosis Research Society-23 Outcome Instrument scoring system . A mean postoperative score of 20 out of 25 indicated a satisfactory outcome.
Lateral thoracolumbar X-ray showing PPSO & discectomy performed at the L4 and L34 level, respectively, and lateral thoracolumbar X-ray showing the correction angle of approximately 30 degrees at the same level postoperatively. PPSO : partial pedicle subtraction osteotomy.Follow-up anteroposterior and lateral whole spine X-rays showing satisfactory correction of coronal and sagittal imbalance. *Indicates the lumbar lordosis, **Indicates sagittal vertical axis. PI : pelvic incidence, LL : lumbar lordosis, SVA : sagittal vertical axis.
Is Early Diagnosis Possible
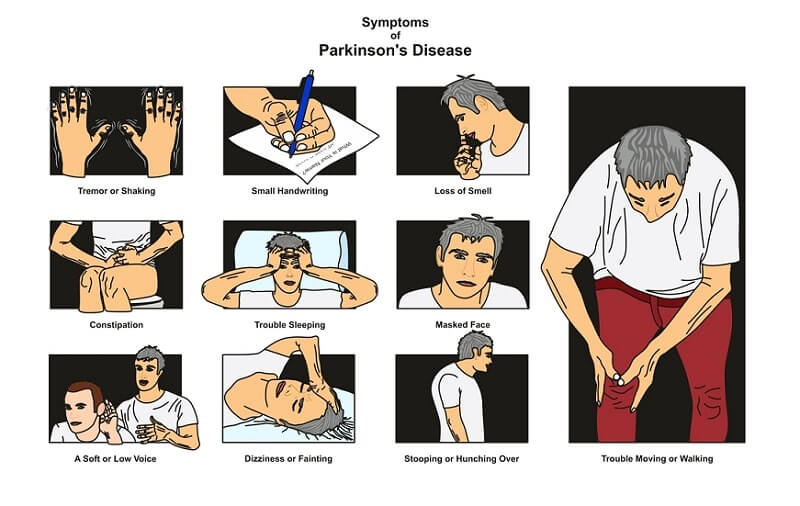
Experts are becoming more aware of symptoms of Parkinsons that precede physical manifestations. Clues to the disease that sometimes show up before motor symptoms and before a formal diagnosis are called prodromal symptoms. These include the loss of sense of smell, a sleep disturbance called REM behavior disorder, ongoing constipation thats not otherwise explained and mood disorders, such as anxiety and depression.
Research into these and other early symptoms holds promise for even more sensitive testing and diagnosis.
For example, biomarker research is trying to answer the question of who gets Parkinsons disease. Researchers hope that once doctors can predict that a person with very early symptoms will eventually get Parkinsons disease, those patients can be appropriately treated. At the very least, these advances could greatly delay progression.
Parkinsons Disease and Movement Disorders Center
Our center provides compassionate and timely treatment to patients with movement disorders, such as dystonia, ataxia, essential tremor and similar conditions. But our mission goes beyond patient care excellence. By offering educational events and support groups, we empower patients and caregivers to become better partners in their health.
You May Like: How Can I Tell If I Have Parkinson’s
A Dilemma Of Symptom Overlap
Patients with Parkinsons disease may exhibit symptoms similar to those observed in cervical spondylotic myelopathy , including ataxia, weakness, and bowel or bladder dysfunction. These similarities present diagnostic and therapeutic challenges when PD and CSM coexist. While CSM is typically treated with surgical decompression , PD requires pharmacologic therapies and is expected to derive little benefit from decompression. This poses a dilemma for both neurologists and spine surgeons treating patients with PD who may have evidence of cervical spondylosis and myelopathy.
Clinical and quality-of-life outcomes following cervical decompression in the PD population remain undefined. Defining these outcomes may improve patient management and help avoid unnecessary surgical intervention. To that end, Cleveland Clinic Center for Spine Health clinicians and researchers recently sought to investigate clinical and QOL outcomes following cervical decompression among patients with CSM with and without coexisting PD. We hypothesized that both groups would benefit from surgery but that patients with concomitant PD would experience inferior outcomes.
Figure. Preoperative sagittal T2 MRI of a patient with coexistent cervical spondylotic myelopathy and Parkinson disease. Note the severe cervical stenosis and cord compression at C3-4and C4-5 . Postoperative X-ray after the patient underwent laminectomies at C3 through C5 and extension of her fusion to C3 via a dorsal approach.
Complications Related To Parkinsons Can Affect Survival
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology. She is an associate professor of neurology at Tufts Medical School and medical director of the Lahey Clinic Multiple Sclerosis Center in Lexington, Massachusetts.
Parkinsons is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinsons disease in the United States. During the six-year period, 64% of the participants with Parkinsons disease passed away.
The risk of death of those with Parkinsons was then compared to Medicare beneficiaries who did not have Parkinsons or any other common diseases, including:
When controlling for variables like age, race, and gender, the six-year risk of death among people with Parkinsons was found to be nearly four times greater than those Medicare beneficiaries without the disease or other common diseases.
At the same time, the rate of death among those with Parkinsons disease was similar to those with hip fracture, Alzheimers dementia, or a recent heart attackalthough it was higher than those who had been newly diagnosed with either colorectal cancer, stroke, ischemic heart disease, or chronic obstructive pulmonary disease.
Also Check: 1st Sign Of Parkinsons
Don’t Miss: Is There A Disease That Mimics Parkinson’s
Points To Remember About Spinal Stenosis
- Spinal stenosis happens when the spaces in the spine narrow and create pressure on the spinal cord and nerve roots. The narrowing usually occurs over time.
- Depending on the location of the spinal stenosis, symptoms can include pain, numbness, and weakness in your legs, feet, arms, and hands.
- Treatments for spinal stenosis can include nonsurgical treatments such as physical therapy, medications to help manage pain, and, in some cases, surgery.
- To help you live with spinal stenosis, get regular exercise, change activities in your routine that cause pain, maintain a healthy weight, and dont smoke.
New Jersey Spine Treatment Center
Our team of board-certified spinal specialists at theBrain, Spine & Neuromuscular Care Center of The Department of Neurosurgery at Rutgers Health and RWJBarnabas Health treat a variety of all types of spinal stenosis affecting all areas of the spine, including lumbarspinal stenosis. We treat thousands of patients every year who suffer from neurological conditions, and offer a multidisciplinary approach from a dedicated, board-certified team of physicians who specialize in neuroscience, from neurology to neurosurgery and beyond.
Recommended Reading: How Does Parkinson’s Disease Kill You
What Are The Symptoms Of Spinal Stenosis
Symptoms of spinal stenosis happen when the spaces within the spine narrow and put pressure on the spine. This occurs most often in the lower back and neck. For most people, symptoms develop slowly, and some people may not have any symptoms.
Symptoms of spinal stenosis in the lower back can include:
- Pain in the lower back.
- Burning pain or ache that spreads down the buttocks and into the legs, that typically worsens with standing or walking and gets better with leaning forward.
- Numbness, tingling, or cramping in the legs and feet. These may get worse when you stand or walk.
- Weakness in the legs and feet.
Symptoms of spinal stenosis in the neck may include:
- Neck pain.
- Numbness or tingling that spreads down the arms into the hands.
- Weakness in a hand, arm, or fingers.
Recommended Reading: Serotonin Syndrome And Parkinsonâs
Interested In Parkinsons Disease Research Sign Up For Our Forums And Join The Conversation
A total of 97 Parkinsons patients at a mean age of 67.7 years, including 60 men, and 97 individuals used as controls at a mean age of 67.5 years, including six men, without the disorder or other neuromuscular diseases, filled out a questionnaire on the intensity of local lumbar back pain. The intensity of leg radicular pain caused by inflammation and/or injury to a spinal nerve root was quantified by the visual analogue scale a continuous scale used to measure pain intensity.
In addition, the participants permanent functional disability was assessed via the Oswestry Low Back Pain Disability Questionnaire a self-completed questionnaire that includes 10 different topics: intensity of pain, lifting, ability to care for oneself, ability to walk, ability to sit, sexual function, ability to stand, social life, sleep quality, and ability to travel.
Patients were further asked to describe the painful sensation they experience as pricking, tingling, burning, paresthesia often described as feelings of pins and needles, or numbness or other.
The team also assessed Parkinsons duration, medications being used, severity of motor symptoms as assessed by the Unified Parkinsons disease rating scale part III and the Hoehn and Yahr stage, which is a system used to assess symptom progression.
According to the ODI results, minimal disability was reported by 43.8% of Parkinsons patients, moderate disability by 27.5%, severe disability by 22.5%, and crippled by 6.3%.
Don’t Miss: When To Take Parkinson’s Medication
Treatment Of Lumbar Spinal Stenosis
For most patients, treatment begins with conservative, nonoperative therapies. Treatment may include anti-inflammatory medication, pain medication, and nerve pain medication such as gabapentin or pregabalin. Sometimes cortisone steroid injections are ordered for the lumbar spine, also known as epidural injections. This can reduce symptoms and is often repeated for maximum results. It is not a cure, but it can help manage the symptoms of lumbar spinal stenosis.
Surgery is often the best option for patients whose symptoms do not improve with non-operative treatments, or if they have severe symptoms such as progressive weakness or incontinence. Surgery is usually very successful in patients who need it to relieve leg pain, sciatica, and numbness. However, patients who have severe nerve compression for an extended length of time may have permanent loss of nerve function that cannot be recovered.
The Effect Of Parkinsons Disease On Patients Undergoing Lumbar Spine Surgery
Jeffrey Gilligan
1Department of Neurosurgery, Icahn School of Medicine at Mount Sinai, New York, NY, USA
2Department of Neurosurgery, North Jersey Spine Group, Wayne, NJ, USA
3Department of Orthopaedics, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Abstract
1. Introduction
Parkinsons disease is a neurodegenerative disorder characterized by resting tremors, rigidity, bradykinesia, postural instability, and gait disturbances . The prevalence of PD in industrialized countries is estimated at 0.3% of the entire population with approximately 7 million people affected worldwide . PD is an age-related disease which is rare before the age of 50, with a prevalence of about 1% in people over the age of 60 and up to 4% in people over the age of 80 .
PD is increasingly recognized as an important cause of spinal disorders requiring surgical intervention . However, spinal procedures can be complicated by underlying osteoporosis and severe musculoskeletal dysfunction in this population.
In this study, we investigate the effect of PD on patients undergoing lumbar spine surgery. The aim of this study is to identify the incidence, trend, risk factors, outcomes, and cost of lumbar spinal surgery for degenerative disease in PD patients.
2. Materials and Methods
2.1. Sample Selection
2.2. Outcome Measures
2.3. Data Analysis
No Institutional Board Review approval was required for this study.
3. Results
| Demographics |
4. Discussion
5. Conclusion
Data Availability
Disclosure
You May Like: What’s The Difference Between Parkinson’s And Dementia
What Causes Spinal Stenosis
Spinal stenosis can be both an inherited condition, like achondroplasia, a defective bone formation that narrows the spinal canal, said the National Institute of Arthritis and Musculoskeletal and Skin Diseases . It can also be acquired as the result of a condition like scoliosis, in which the curvature of the spine affects the surrounding nerves, tissue, and ligaments. Or, it can be the result of a degenerative condition. Everything from bone spurs to bulging discs to spondylolisthesis to osteoarthritis can cause the spinal cord to narrow.
This reinforces the importance of seeing a doctor for back pain. Its obviously important to continue treatment from a leading back doctor if you were born with a condition that needs to be controlled, both for pain management and so it wont worsen and turn into spinal stenosis. But, going to the doctor for back pain is not something everyone does at the first sign of symptoms knowing how dangerous conditions like spinal stenosis can be should help convince back pain sufferers to allow a professional to do a thorough examination and develop a plan to treat the issue so it does not degenerate.
Biography Of Charles J Malemud
Charles J. Malemud received the Ph.D. from George Washington University in 1973 and completed postdoctoral studies at the State University of New York at Stony Brook in 1977. Since 1977, Dr. Malemud has been a member of the faculty at Case Western Reserve University School of Medicine where he is presently Professor of Medicine & Anatomy in the Division of Rheumatic Diseases and Senior Investigator of the Arthritis Research Group. He has published over 230 papers, chapters and reviews primarily in the field of chondrocyte biology. Professor Malemud is on the editorial board of several rheumatology, immunology and musculoskeletal journals and is Editor-in-Chief of the Journal of Clinical and Cellular Immunology and Global Vaccines and Immunology.
You May Like: How To Use Hemp Oil For Parkinson’s
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Why Is Diagnosis Difficult
Unfortunately Parkinsons Syndrome Sufferers may present with rather confusing combinations of symptoms arising from the loss of nerve function and muscle stiffness or spasm as well as the symptoms arising from the Degenerative Disc Disease at more than one disc level.
In the light of the primary diagnosis of Parkinsons Syndrome, physicians tend to associate symptoms with the Parkinsons Syndrome rather than that of the underlying Degenerative Disc Disease. In addition the dangers of treating the Degenerative Disc Disease with open surgery for this particular group of patients makes physicians or surgeons reticent to offer the surgical solutions which would be offered to less challenged patents.
Until the advent of aware state surgical examination, the sources of Parkinsons Syndrome Sufferers were hard to define and surgeons engaged in pre-operative guesstimation based on the results of clinical examination, X-rays, MRI scans and CAT scans. The complexity of the spinal region means that a wide range of possible conditions exist to confound diagnosis. In the presence of Degenerative Disc Disease the surgeon will tend to focus upon and treat evident pathology on the scan. In our published studies the pain was found to be arising at an adjacent level in almost 20% of cases.
Also Check: How To Get Tested For Parkinson’s
