What Is Parkinsons Disease
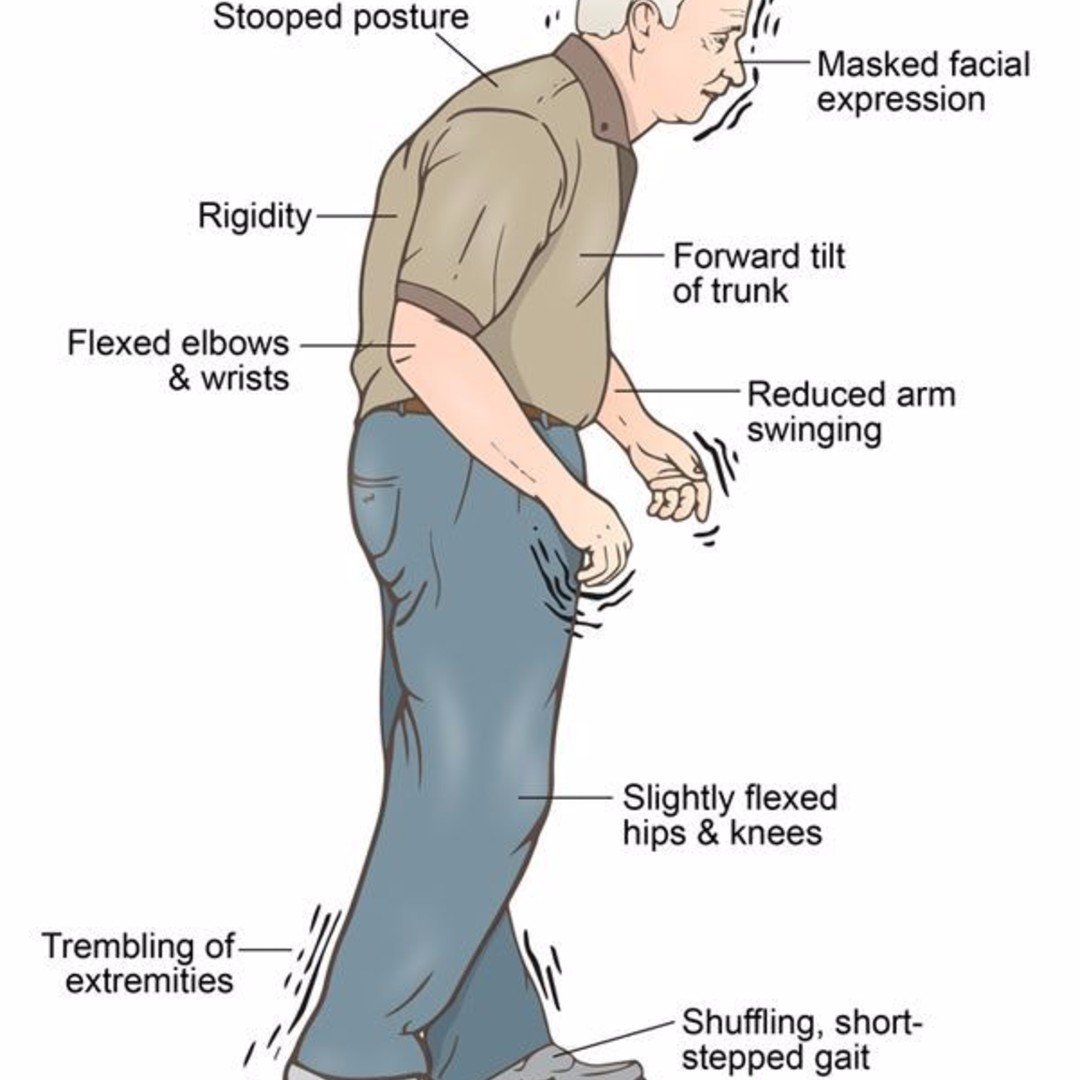
Parkinsons disease is a chronic, progressive and often disabling disease of the nervous system characterized by:
Medications are used to treat the symptoms the most commonly prescribed drug is a levodopa/carbidopa combination . One unfortunate side effect of levodopa is the development of dyskinesias abnormal, involuntary movements. Dyskinesias can become a significantly disabling feature of Parkinsons disease.
As Parkinsons disease progresses, the symptoms become less responsive to medical therapy. Patients often suffer from the on-off phenomenon, in which their mobility abruptly changes from good to severely impaired . For these patients who continue to be severely disabled in spite of optimal medical therapy, surgical intervention should be considered.
Who Is A Candidate
You may be a candidate for DBS if you have:
- a movement disorder with worsening symptoms and your medications have begun to lose effectiveness.
- troubling “off” periods when your medication wears off before the next dose can be taken.
- troubling “on” periods when you develop medication-induced dyskinesias .
DBS may not be an option if you have severe untreated depression, advanced dementia, or if you have symptoms that are not typical for Parkinson’s.
DBS can help treat symptoms caused by:
- Parkinson’s disease: tremor, rigidity, and slowness of movement caused by the death of dopamine-producing nerve cells responsible for relaying messages that control body movement.
- Essential tremor: involuntary rhythmic tremors of the hands and arms, occurring both at rest and during purposeful movement. Also may affect the head in a “no-no” motion.
- Dystonia: involuntary movements and prolonged muscle contraction, resulting in twisting or writhing body motions, tremor, and abnormal posture. May involve the entire body, or only an isolated area. Spasms can often be suppressed by “sensory tricks,” such as touching the face, eyebrows, or hands.
After your evaluation and videotaping is complete, your case will be discussed at a conference with multiple physicians, nurses, and surgeons. The team discusses the best treatment plan for each patient. If the team agrees that you are a good candidate for DBS, you will be contacted to schedule an appointment with a neurosurgeon.
Bwh: Comprehensive Treatment For Patients With Parkinson’s Disease
The Movement Disorder Program at BWH provides comprehensive evaluation and treatment for patients with movement disorders, including Parkinson’s disease, tremor, and dystonia . The Program’s team of physicians, nurses, and researchers is dedicated to advancing the understanding and treatment of Parkinson’s disease and related disorders. The Program is a collaboration between BWH and Massachusetts General Hospital working with the national Parkinson Study Group. In addition to Parkinson’s disease, the Program provides comprehensive care for patients with other movement disorders such as Tourette syndrome, tremor, and dystonia .
Don’t Miss: Does Essential Tremor Lead To Parkinson
How Deep Brain Stimulation Works
Exactly how DBS works is not completely understood, but many experts believe it regulates abnormal electrical signaling patterns in the brain. To control normal movement and other functions, brain cells communicate with each other using electrical signals. In Parkinson’s disease, these signals become irregular and uncoordinated, which leads to motor symptoms. DBS may interrupt the irregular signaling patterns so cells can communicate more smoothly and symptoms lessen.
Living With A Stimulator
Once the DBS has been programmed, you are sent home with instructions for adjusting your own stimulation. The handheld controller allows you turn the stimulator on and off, select programs, and adjust the strength of the stimulation. Most patients keep their DBS system turned on 24 hours day and night. Some patients with essential tremor can use it during the day and turn off the system before bedtime. Your doctor may alter the settings on follow-up visits if necessary.
If your DBS has a rechargeable battery, you will need to use a charging unit. On average charging time is 1 to 2 hours per week. You will have a choice of either a primary cell battery or a rechargeable unit and you should discuss this with you surgeon prior to surgery.
Just like a cardiac pacemaker, other devices such as cellular phones, pagers, microwaves, security doors, and anti theft sensors will not affect your stimulator. Be sure to carry your Implanted Device Identification card when flying, since the device is detected at airport security gates.
Don’t Miss: Home Exercise For Parkinson Disease
Are There Any Alternative Treatments
Some research suggests that a supplement called coenzyme Q10 may help in the early stages of Parkinsons when taken for 16 months or longer. For mild to moderate Parkinsons, the practice of tai chi may help improve balance more than resistance training or stretching.
Other complementary therapies may include:
- massage or meditation for relaxation
- acupuncture for pain reduction
- yoga to improve flexibility and balance
Some dietary or herbal supplements can react with medications, so talk to your doctor before starting any supplements.
The neurostimulator runs on batteries that last three to five years. They can be replaced in an outpatient procedure.
Your doctor will provide you with specific instructions on life with DBS, such as:
- Other screening devices and theft detectors in stores and other public venues can cause your neurostimulator to turn off or on. This may cause a mild, uncomfortable sensation. Show your ID card and ask for assistance in bypassing these devices, if possible.
- Places to avoid include those with large magnetic fields, such as power generators and automobile junkyards. You should also avoid high-voltage or radar machinery, including television and radio transmitters, high-tension wires, electric arc welders, radar installations, and smelting furnaces.
- Its safe to use cellphones,home appliances, and computers, as they wont cause interference.
Read Also: Rehabilitation Programs For Parkinsons Disease
Parkinsons Disease Treatment Options
Parkinsons is incurable, but the symptoms can be managed as the disease progresses. Initially, your doctor may recommend lifestyle changes, such as ongoing aerobic exercise, healthy diet, and advice for avoiding falls.
Medication
-
Carbidopa-levodopa : Sometimes simply called Levodopa, is the most effective Parkinsons disease medication and has been since its breakthrough in the late 1960s. It is an effective first-line treatment for Parkinsons and comes in many formulations, including slow- and extended-release pills, and infusions. It works by introducing a natural chemical to the body which converts into dopamine in the brain. This helps reduce symptoms of stiffness and tremors. The medication does not slow the progression of the disease.
-
Catechol O-methyltransferase inhibitors: These pills can boost the effectiveness of carbidopa-levodopa. It helps block the brains dopamine breakdown to help reduce some of the tremors and motor symptoms of Parkinsons.
-
Dopamine agonists: This medication mimics the effect of dopamine in the brain and may be used with carbidopa-levodopa. It can be prescribed in the early stages of Parkinsons, and it can lengthen the effectiveness of carbidopa-levodopa.
Innovative surgical options
Clinical Trials
You May Like: How Young Can You Get Parkinson’s Disease
What Happens During Surgery
For stage 1, implanting the electrodes in the brain, the entire process lasts 4 to 6 hours. The surgery generally lasts 3 to 4 hours.
Step 1: attach stereotactic frameThe procedure is performed stereotactically, which requires attaching a frame to your head. While you are seated, the frame is temporarily positioned on your head with Velcro straps. The four pin sites are injected with local anesthesia to minimize discomfort. You will feel some pressure as the pins are tightened .
Step 2: MRI or CT scanYou will then have an imaging scan, using either CT or MRI. A box-shaped localizing device is placed over the top of the frame. Markers in the box show up on the scan and help pinpoint the exact three-dimensional coordinates of the target area within the brain. The surgeon uses the MRI / CT scans and special computer software to plan the trajectory of the electrode.
Step 3: skin and skull incisionYou will be taken to the operating room. You will lie on the table and the stereotactic head frame will be secured. This prevents any small movements of your head while inserting the electrodes. You will remain awake during surgery. Light sedation is given to make you more comfortable during the initial skin incision, but then stopped so that you can talk to the doctors and perform tasks.
How Does Deep Brain Stimulation Work
Movement-related symptoms of Parkinsons disease and other neurological conditions are caused by disorganized electrical signals in the areas of the brain that control movement. When successful, DBS interrupts the irregular signals that cause tremors and other movement symptoms.
After a series of tests that determines the optimal placement, neurosurgeons implant one or more wires, called leads, inside the brain. The leads are connected with an insulated wire extension to a very small neurostimulator implanted under the persons collarbone, similar to a heart pacemaker. Continuous pulses of electric current from the neurostimulator pass through the leads and into the brain.
A few weeks after the neurostimulator has been in place, the doctor programs it to deliver an electrical signal. This programming process may take more than one visit over a period of weeks or months to ensure the current is properly adjusted and providing effective results. In adjusting the device, the doctor seeks an optimal balance between improving symptom control and limiting side effects.
Recommended Reading: Does Parkinsons Cause Neuropathy
Also Check: Healed From Parkinson’s Disease
Am I A Candidate For Dbs
DBS might be an option for you if medication no longer controls your movement symptoms well, or if it causes severe side effects.
You could be a good candidate for DBS if at least one of these situations applies to you:
- You’ve been diagnosed with idiopathic, or classic, Parkinson’s disease.
- Your symptoms improved with medication like Sinemet .
- Your medication no longer works as well as it once did.
- Your medication causes troublesome side effects.
- You need to take more types of medication, or more frequent or higher doses.
About The Therapy Dbs For Parkinson’s Disease
This is Medtronics main page for information about DBS therapy for Parkinsons disease. Links direct you to further webpages with text and videos on How DBS May Help, “The Right Time to Start,””Getting DBS: What to Expect,””A Closer Look at DBS Surgery,” personal stories and professional commentary.
Read Also: Did Katharine Hepburn Have Parkinson’s
Testing Before Deep Brain Stimulation
For patients with Parkinsons disease, the doctor must confirm that the PD is levodopa-responsive and determine which symptoms are most likely to respond to DBS and discuss these with the patient.
To accomplish these two objectives, the movement disorders neurologist will examine the patient in the absence of his or her PD medications, then again after having taken them. Seeing the effect of PD medications on the movement and non-motor symptoms helps the physician and patient identify good target symptoms for DBS.
A cognitive assessment can help determine a persons ability to participate in the procedure, which involves providing feedback to the doctor during surgery and throughout the neurostimulator adjustment process. This assessment also informs the team of the risk of having worsened confusion or cognitive problems following the procedure.
Some hospitals also perform an occupational therapy review or speech, language and swallowing assessment. A psychiatrist may examine the person to determine if a condition such as depression or anxiety requires treatment before the DBS procedure.
Dont Miss: What Foods Are Good For Parkinsons Disease
A Stanford Neurosurgeon Answered Questions About Deep Brain Stimulation

Stanfords Parkinsons Community Outreach Program hosts a quarterly deep brain stimulation support group meeting for those wanting to learn more about this surgical treatment for Parkinsons disease . The June 2020 meeting featured Dr. Daniel Kramer, a neurosurgeon and clinical instructor at Stanford, who answered audience questions pertaining to DBS.
Read Also: Why Do Parkinson’s Patients Cough
Innovative Deep Brain Stimulation Device Reads Brain Signals Allowing For Individualized Treatment For Parkinsons Patients
Pacific Neuroscience Institute at Providence Saint Johns Health Center among first treatment sites
SANTA MONICA Pacific Neuroscience Institute is the first provider in the Providence health system to treat a patient with an innovative surgically implanted Deep Brain Stimulation device.
Used for the management of symptoms of movement disorders such as Parkinsons disease, Percept PC Neurostimulator with BrainSense technology has been developed by Medtronic as a next-generation Deep Brain Stimulation system. The Food and Drug Administration-approved device is the first and only DBS system in the U.S. with ground-breaking BrainSense technology that allows clinicians to capture a patients brain signals, enabling more data-driven, personalized treatment for patients with neurologic disorders, such as Parkinsons disease, essential tremor and epilepsy.
Many patients with PD may be good candidates for deep brain stimulation surgery, said neurologist Melita Petrossian, MD, medical director at Pacific Movement Disorders Center, Pacific Neuroscience Institute. It is a way to reduce off time, increase the amount of time the medication is working on time, reduce tremor and reduce dyskinesias, which are the involuntary movements related to treatment.
Will I Be Asleep During The Entire Procedure
You will be sedated or receive local anesthesia for part of the procedure, may or may not be awake for lead and electrode placement, and will be asleep when the impulse generator is implanted. To provide more details:
- A local anesthetic is applied to areas of the head where pins or screws are used to secure the head frame and sedation is given.
- You will be sedated during the beginning of the procedure, while the surgical team is opening the skin and drilling the opening in the skull for placement of the lead.
- Most patients will be awake for lead and electrode placement. This part of the procedure is not painful, as the brain does not feel pain. Being awake allows the surgical team to interact with you when testing the effects of the stimulation. However, some patients who cannot tolerate the procedure while awake can have the electrode and lead placed under general anesthesia. The lead placement is guided in real time by magnetic resonance imaging. The procedure is performed in a special MR-equipped operation room.
- Implantation of the pulse generator in the chest and connection of the leads from the device to the lead in the brain is usually done under general anesthesia.
Also Check: Parkinsons Help For Caregivers
Recommended Reading: Is It Safe To Drink Alcohol With Parkinson’s Disease
Neurosurgery And Parkinson Disease: Past Present And Future Of Deep Brain Stimulation
Atom Sarkar, MD, PhDNeurologyLive
Surgical care for PD is safe and effective, and should no longer be treated as a consideration of last resort, but as a treatment option discussed early in the disease course with the patient and their family.
FOR AS LONG AS HUMANS have coalesced as communities, beginning nearly 10,000 years ago in the Neolithic period, there has been a fascination with the skull and brain. From here emerged the rudiments of neurosurgery. In regions ranging from the Ensisheim in Alsace, France, to the Peruvian Altiplano, we know trepanation was practiced. In trepanation, a hole is scraped or drilled into the human skull, and it is the oldest documented surgical procedure performed by man. While we can only speculate about the millennia-old reasons for such proceduresspanning from the mystical to spiritual and ritualthey must be favored over any current-day notion of medicinal. Nevertheless, such experiences of the shaman and healers of lore should not be discounted, because some of our current neurosurgical practices, in particular the practice of minimal-access surgery, harken back to their legacy of transcalvarial access.
Patients lose autonomy as the disease progresses, which is incalculable in terms of personal loss. Economically, the estimated annual cost to the health care system in the United States alone is more than $50 billion.6
Can I Use Electrical Devices
While you should be able to use most electronic devices, you should be aware that:
- Some devices, such as theft detectors and screening devices, like those found in airports, department stores, and public libraries, can cause your neurotransmitter to switch on or off. Usually, this only causes an uncomfortable sensation. However, your symptoms could get worse suddenly. Always carry the identification card given to you. With this, you may request assistance to bypass those devices.
- You will be able to use home appliances, computers, and cell phones. They do not usually interfere with your implanted stimulator.
- You will be provided with a magnet to activate and deactivate your stimulator. This magnet may damage televisions, credit cards, and computer discs. Always keep it at least 1 foot away from these items.
Also Check: Types Of Parkinsons Disease
Also Check: What Is Off Time In Parkinson’s Disease
Who Is Not A Good Candidate For Dbs
You are not a good candidate for DBS if:
- You do not have a clear diagnosis of Parkinson’s disease.
- You have Parkinsons plus or an atypical form of the disease. Parkinsons plus disorders include multiple system atrophy, progressive supranuclear palsy and vascular parkinsonism. DBS might make these disorders worse.
- You have certain brain conditions, such as ischemic brain disease, demyelinating brain disease or brain tumors.
- You are not healthy enough for surgery.
If you are evaluated for DBS and not a candidate, your OHSU movement disorders neurologist will recommend other options.
Parkinsons Disease Treatment: Why Choose Johns Hopkins
- Our team offers the newest and most effective therapies to address Parkinsons disease symptoms, from carbidopa/levodopa infusion therapy and laser ablation of brain lesions to deep brain stimulation and transcranial direct current stimulation.
- World-class neuroscientists at Johns Hopkins are exploring the biochemical pathways involved in Parkinsons disease, yielding greater understanding of the disease and paving the way for new treatments.
- Top specialists in neurology, neurosurgery, physical therapy, speech and swallowing, occupational therapy and mental health work together to improve quality of life for people with Parkinsons disease.
- Our Parkinsons disease center is a leader in establishing benchmarks for quality care and educating physicians, patients and caregivers.
Also Check: How Is The Brain Affected By Parkinson’s Disease
