Take Your Parkinsons Medications As Prescribed
Take your medications exactly as prescribed by your doctor in the right dose, and at the right time of day, and in the right way. Youll be given instructions when youre first prescribed a drug. Some medications are meant to be taken on an empty stomach, while others should be taken with food.
Parkinsons patients who have trouble remembering when and in what dose to take their drugs can:
- Set a medication alarm on a smart phone, for instance. There are even special apps to remind you when to take your meds.
- Have their pills organized into a special medication box so they dont have to think about what to take each time.
- Many pharmacies are able to put together compliance medicine packages that organize your drugs in a way that makes it easier to take them at the right time.
- When you take your meds, mark it off on a calendar.
- If necessary, a partner or carer can help you remember to take your drugs.
How Anticholinergics Are Used
These medications are older and are not used very often for Parkinsons today. Sometimes they are prescribed for reducing tremor and muscle stiffness. They can be used on their own, especially in the early stages of your Parkinsons when symptoms are mild, before levodopa is prescribed.
Anticholinergics can also be used with levodopa or a glutamate antagonist. They are taken as tablets or as a liquid.
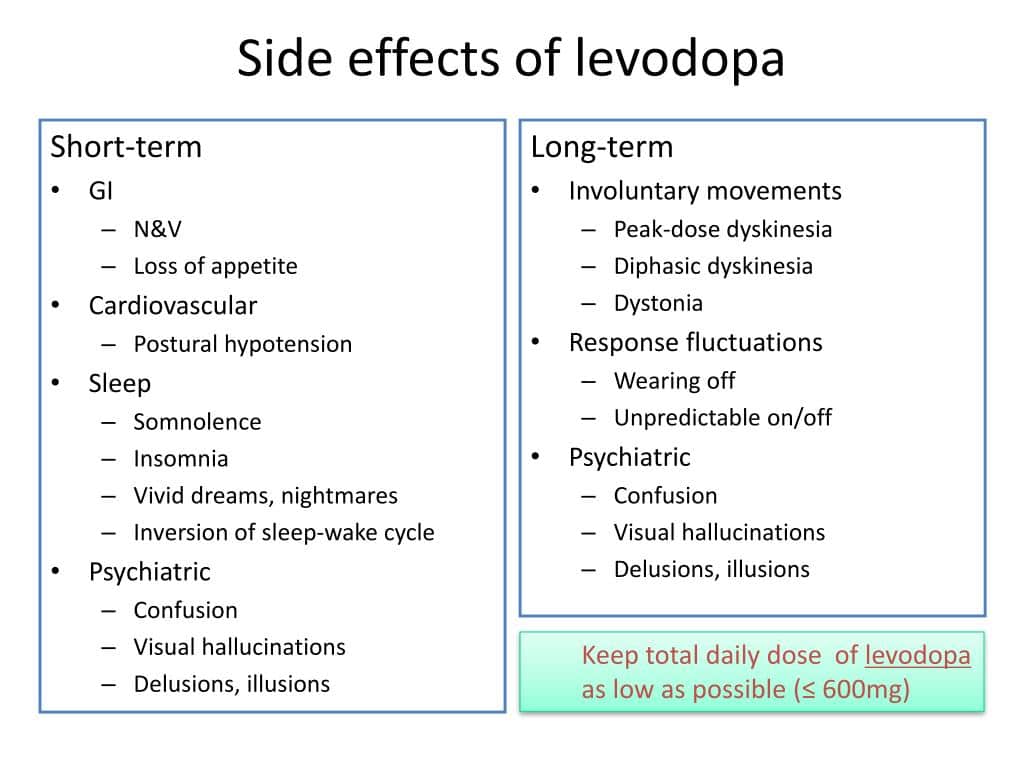
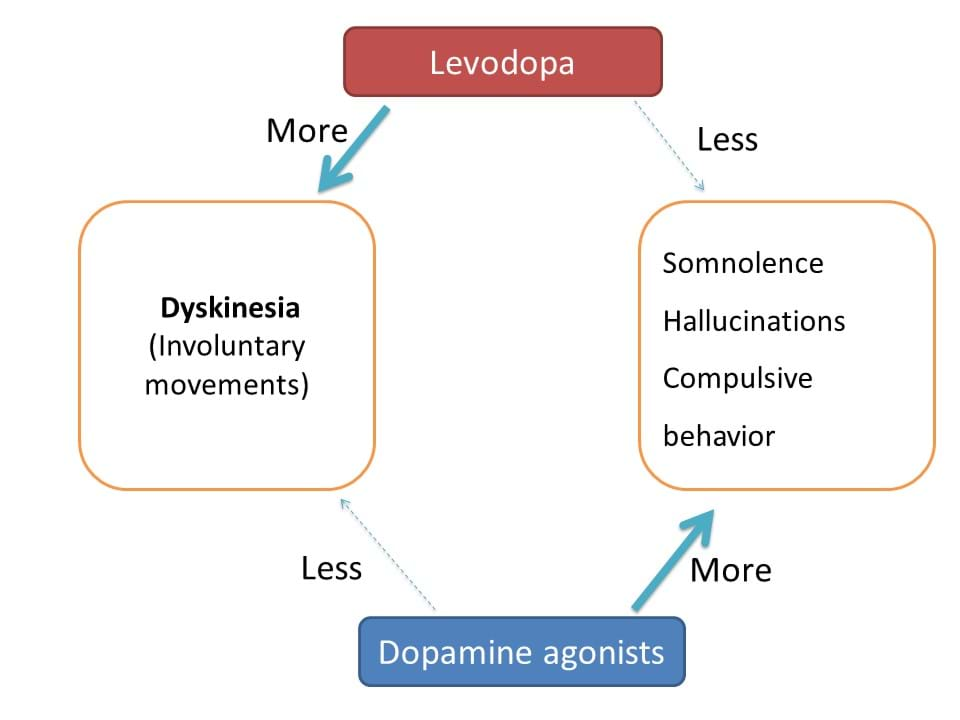
If Levodopa Causes Dyskinesia Then Why Should I Take It
At present, treatment with levodopa is the most effective way to relieve tremor, stiffness, and slow movement associated with Parkinsons. In the early stage of Parkinsons, levodopa may not be necessary and there are other medications available to treat this stage of the disease. However, as the disease progresses and symptoms begin to interfere with daily living, your doctor will prescribe levodopa.
- It typically doesnt develop immediately Its important to note that there is usually a time lag of roughly 4 to 10 years from the start of treatment with levodopa to when dyskinesia emerges, and its severity will vary among different individuals.
- Younger people are at a greater risk People who get Parkinsons in their later years may not show signs of dyskinesia or may have only mild symptoms within their lifetime. Being diagnosed with Parkinsons at a younger age is associated with a greater chance of developing dyskinesia.
- As with every aspect of Parkinsons, there is variability in dyskinesias Some do not develop dyskinesias at all. For those who do get them, not all experience them the same. Dyskinesia in its milder form may not be bothersome, and the mobility afforded by taking levodopa may be preferable to the immobility associated with not taking levodopa. People with Parkinsons must weigh the benefits from using levodopa versus the impact of dyskinesia on their quality of life.
You May Like: What Not To Eat If You Have Parkinson’s
Impulsive And Compulsive Behavior
Some people taking dopamine agonists may experience problems with impulsive or compulsive behaviours. For example an increased desire to gamble or engage in sexual activity. These behaviours often develop slowly so may not seem to be a problem immediately. It is important for both the person living with Parkinsons and their family to be aware of this side effect. If affected by this side effect, a reduction in dose or stopping the medication will stop the behaviour.
Speech And Occupational Therapy
Parkinsons disease can lead to slurred speech and difficulty swallowing. A speech and language therapist can provide muscle training techniques that may help overcome some of these problems.
An occupational therapist can help identify everyday tasks that can be challenging and work with the person to find practical solutions.
This may include new strategies for dressing, preparing meals, performing household chores, and shopping. Adaptations to the home environment can also make daily living easier.
For people with Parkinsons disease, deep brain stimulation may help manage:
- an electrode inside the part of the brain that controls movement
- a pacemaker-like device, or neurostimulator, under the skin in the upper chest
- a wire under the skin connecting the neurostimulator to the electrode
The neurostimulator sends electrical impulses along the wire and into the brain via the electrode. These impulses can prevent symptoms by interfering with the electrical signals that cause them.
There is a small risk of brain hemorrhage, infection, and headaches. Some people may see no improvement, or their symptoms may worsen. There may also be discomfort during stimulation.
Nevertheless, the AAN considers this treatment safe and effective for specific people and say any adverse effects are usually mild and reversible. Anyone considering this treatment should discuss the pros and cons with a healthcare professional.
Recommended Reading: Spinal Stenosis And Parkinsons Disease
Don’t Miss: Benadryl And Parkinson’s Disease
How To Cope With Side Effects
What to do about:
- loss of appetite, feeling or being sick having a low-protein snack with your medicine may help if youre feeling or being sick. If you lose your appetite, eat when you would usually expect to be hungry. It may help to eat smaller meals, more often than usual. If you are being sick, take small sips of water to avoid dehydration.
- feeling dizzy if you feel dizzy when you stand up, try getting up very slowly or stay sitting down until you feel better. If you begin to feel dizzy, lie down so you do not faint, then sit until you feel better. Do not drive, cycle, or use tools or machines if you feel dizzy or tired. Do not drink alcohol as it may make you feel worse.
- problems sleeping avoid big meals, smoking, or drinking alcohol, tea or coffee in the evening. Try not to watch TV or use your mobile phone before going to bed, and relax for an hour before bedtime. Do not take any sleep remedies, including herbal medicines, without talking to a pharmacist or your specialist nurse first.
- uncontrollable twitching, twisting orwrithingmovements let your doctor or specialist nurse know as soon as possible
How Is Parkinsons Treated In The Early Stages
Three main groups of medication are used to treat Parkinsons in the early stages:
- Levodopa : is converted into dopamine in the brain.
- Dopamine agonists: stimulate the nerve receptors responsible for the uptake of dopamine.
- MAO-B inhibitors : block the breakdown of dopamine in the brain.
The medications are usually taken in tablet form. Some dopamine agonists are also available as patches.
In the early stages, some people with mild symptoms cope just fine without medication. If at some stage the symptoms become too much of a problem, levodopa and dopamine agonists are the main medication options. They work slightly differently to each other, and some products may cause side effects more often or have worse side effects than others. But both are very effective in the early stages of the illness. That helps many people with Parkinsons to live a fairly symptom-free life for at least a few years.
Also Check: What Color Is Parkinson’s Awareness
Taking Sinemet With Food
Sinemet can be taken either with or without food. However, you should avoid taking Sinemet with foods that are high in protein. Some examples of high-protein foods are meat, eggs, or tofu.
Eating high-protein foods when you take your Sinemet dose may lengthen the time it takes for your body to absorb the drug. This delay means that your PD symptoms may not be reduced as quickly as usual after taking your dose.
Taking Sinemet while youre eating a diet high in protein may also decrease the total amount of levodopa that your body absorbs. This means that the drug may not work as well to treat your PD symptoms.
Talk with your doctor or pharmacist about when the best times are for you to take your Sinemet doses. They will be able to help you determine the best times, based on your other medications and your normal mealtimes.
How Long Does Rytary Last In Your System
Rytary lasts for about 4 to 5 hours inside your body. Over this period of time, the drug works to treat symptoms of your condition.
Rytary is an extended-release medication that contains two active drugs: carbidopa and levodopa. Because its ER, Rytary slowly releases these active drugs into your body over time. Rytary lasts longer in your body and works over a longer period of time than immediate-release drugs do.
Rytary is made up of:
- one-third IR levodopa and carbidopa
- two-thirds ER levodopa and carbidopa
So Rytary starts to work immediately, but it also continues to work over the following 4 to 5 hours. This helps to keep the medication levels more consistent in your body, so that your symptoms are better managed throughout the day.
Recommended Reading: How To Stop The Progression Of Parkinson’s Disease
Other Uses For Rytary
The Food and Drug Administration approves prescription drugs such as Rytary to treat certain conditions. Rytary may also be used off-label for other conditions. Off-label use is when a drug thats approved to treat one condition is used to treat a different condition.
Rytary is FDA-approved to treat Parkinsons disease .
In addition, Rytary is approved to treat parkinsonism, which is a condition that causes symptoms similar to those of PD. Below, we describe how Rytary is used for parkinsonism.
Dosage If Youre Switching From Immediate
Rytary comes as extended-release capsules that contain two active drugs: levodopa and carbidopa. ER medications slowly release their active drugs into your body over time. And ER medications work consistently over a longer period of time than do immediate-release medications.
Many other medications that contain both carbidopa and levodopa are IR formulations. This means the medications release their active drugs all at once into your body. The effects of IR drugs dont last as long as the effects of ER drugs do.
Dosages for ER drugs are different than dosages are for IR drugs. Compared with ER drugs, you may have to take IR drugs more often to manage your symptoms. So if youre currently taking an IR form of carbidopa and levodopa, your dosage wont be the same if you switch to Rytary, which contains ER carbidopa and levodopa.
If youre switching from IR carbidopa/levodopa, your Rytary dosage will be calculated based on how much IR levodopa youre currently taking. Your doctor will determine your Rytary dosage using the dosing chart below.
| Total daily dose of IR levodopa | Typical recommended Rytary dosage |
| 3 capsules of 61.25 mg of carbidopa/245 mg of levodopa, taken three times daily |
In any case, you shouldnt take more than 612.5 mg of carbidopa and 2,450 mg of levodopa in one day.
You May Like: How Prevalent Is Parkinson’s Disease In The Population
Who Can And Cannot Take Co
Co-careldopa can be taken by adults . It is sometimes prescribed for children to treat a movement disorder called dystonia.
It is not suitable for some people. To make sure co-careldopais safe for you, tell your doctor if you:
- have had an allergic reaction to co-careldopa, levodopa, carbidopa or any other medicines in the past
- have lung disease or asthma
- have problems with your adrenal glands , liver or kidneys
- are pregnant, trying to get pregnant or breastfeeding
Co-careldopa can affect the results of blood tests and urine tests. Remind your doctor that you’re taking co-careldopa if you need to have any tests.
Will I Need To Use This Drug Long Term
Rytary is meant to be used as a long-term treatment. If you and your doctor determine that Rytary is safe and effective for you, youll likely take it long term.
If youd like to stop taking Rytary, be sure to talk with your doctor first. Suddenly stopping this medication could cause certain withdrawal symptoms. For more information about this, see the Rytary withdrawal and dependence section below.
Also Check: What Drugs Induce Parkinson’s Disease
What Are The Most Common Medicines Used To Treat Pd
Sinemet®
Levodopa is the most commonly prescribed and most effective medicine for controlling the symptoms of PD, particularly bradykinesia and rigidity.
Levodopa is a chemical found naturally in our brains. When given as a medicine, it is transported to the nerve cells in the brain that produce dopamine. It is then converted into dopamine for the nerve cells to use as a neurotransmitter.
Sinemet is made up of levodopa and another drug called carbidopa. Levodopa enters the brain and is converted to dopamine while carbidopa prevents or lessens many of the side effects of levodopa, such as nausea, vomiting, and occasional heart rhythm disturbances. It is generally recommended that patients take Sinemet on an empty stomach, at least ½ hour before or one hour after meals.
There are two forms of Sinemet: controlled-release or immediate-release Sinemet. Controlled-release Sinemet and immediate-release Sinemet are equally effective in treating the symptoms of PD, but some people prefer the controlled release version. Ask your doctor which approach is best for you.
Dopamine agonists
Dopamine agonists are medicines that activate the dopamine receptor. They mimic or copy the function of dopamine in the brain.
Parlodel®, Requip®, and Mirapex® are all dopamine agonists. These medicines might be taken alone or in combination with Sinemet. Generally, dopamine agonists are prescribed first and levodopa is added if the patients symptoms cannot be controlled sufficiently.
Symmetrel®
Looking Out For Side Effects If Youre A Carer
If youre a carer of someone with Parkinsons, medication side effects can be difficult and tiring to cope with.
It may be that the person having side effects such as hallucinations and delusions or impulsive and compulsive behaviour does not realise they are experiencing them.
Its important to seek help from your specialist as soon as you can.
You May Like: How Do You Die From Parkinson’s Disease
Rytary And Other Medications
Below are lists of medications that can interact with Rytary. These lists dont contain all the drugs that may interact with Rytary.
Before taking Rytary, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Rytary and certain depression drugs
Rytary may interact with monoamine oxidase inhibitors , which are a group of drugs used to treat depression. There are two types of MAOIs: selective and nonselective. These two types of MAOIs work slightly differently in your body.
Rytary and nonselective MAOIs
You should never take Rytary with nonselective MAOIs. Taking Rytary along with nonselective MAOIs can cause your blood pressure to become too high. And in some cases, this can lead to a medical emergency.
Examples of nonselective MAOIs include:
- phenelzine
- tranylcypromine
If youre taking a nonselective MAOI, you should stop taking it at least 2 weeks before you start Rytary. But, be sure to talk with your doctor before stopping any medications that youre currently taking.
Rytary and selective MAOIs
If you take Rytary with selective MAOIs, you have an increased risk of orthostatic hypotension. Orthostatic hypotension could cause you to feel dizzy or faint.
- rasagiline
- selegiline
I Have An Excellent Response To Levodopa/carbidopa The Last Few Weeks The Response Has Been Minimal Could This Be Related To Issues With My Gastrointestinal System
This is a common issue that we encounter in the clinics. Abnormal motility of the gut is a common non-motor symptom of Parkinsons disease, and it may inhibit the absorption of levodopa in the small intestine. In such cases patients may report that dyskinesia has also stopped for a few days/weeks . Abnormal stomach and gut motility is also termed gastroparesis. If you face a similar situation, you should be in touch with your neurologist, and it may also be helpful to discuss the issue with a gastroenterologist. If you are experiencing constipation treatment may improve levodopa absorption. To objectively measure the degree of gastroparesis, your gastroenterologist may request a test called a gastric emptying study. Some medications may improve gastroparesis. This class includes domperidone, cisapride, mosapride, erythromycin, and pyridostigmine. However, these should be tried only after discussion with a gastroenterologist or neurologist.
Some patients report a better response when they take levodopa/carbidopa along with a small amount of a carbonated beverage. This is probably because carbonated beverages result in faster disintegration of the tablet and help in a more rapid absorption from the small intestine. It has been shown that dissolving the levodopa in a vitamin C solution and sipping it may also improve absorption . You may consider these options and also consider long term a gastroenterology consultation.
You May Like: Does Parkinson’s Cause Dementia
Parkinsons Treatment For Motor Symptoms
The majority of medications developed specifically to treat Parkinsons disease target common motor symptoms. Many of these treatments are designed to increase the level of the dopamine, a neurotransmitter that transfers signals between nerve cells. Dopamine is involved in regulating signals for movement, which is reduced in the brains of Parkinsons disease patients.
Does Sinemet Cause Side Effects
Sinemet is a combination of two drugs, levodopa and carbidopa. Carbidopa-levodopa is used in the treatment of Parkinson’s disease.
Parkinson’s disease is believed to be caused by low levels of dopamine in certain parts of the brain. When levodopa is taken orally, it crosses into the brain through the “blood- brain barrier.” Once it crosses, it is converted to dopamine. The resulting increase in brain dopamine concentrations is believed to improve nerve conduction and assist the movement disorders in Parkinson disease.
Carbidopa does not cross the blood-brain barrier. Carbidopa is added to the levodopa to prevent the breakdown of levodopa before it crosses into the brain. The addition of carbidopa allows lower doses of levodopa to be used. This reduces the risk of side effects from levodopa such as nausea and vomiting.
Common side effects of Sinemet include
Serious side effects of Sinemet include
- occasional involuntary movements ,
- and infrequently, a drop in white blood cell counts.
Drug interactions of Sinemet include amantadine, benztropine, procyclidine, and trihexyphenidyl because they can enhance the anti-Parkinson’s effects of levodopa.
Droperidol, haloperidol, loxapine, metoclopramide, phenothiazines, and thioxanthenes can inhibit dopamine in the brain and shouldn’t be used in combination with levodopa.
Methyldopa and reserpine also can interfere with the beneficial actions of Sinemet and can increase the risk of side effects.
You May Like: Does Parkinson’s Affect Your Sense Of Taste
