Meds That Improve Some Symptoms Can Exacerbate Others
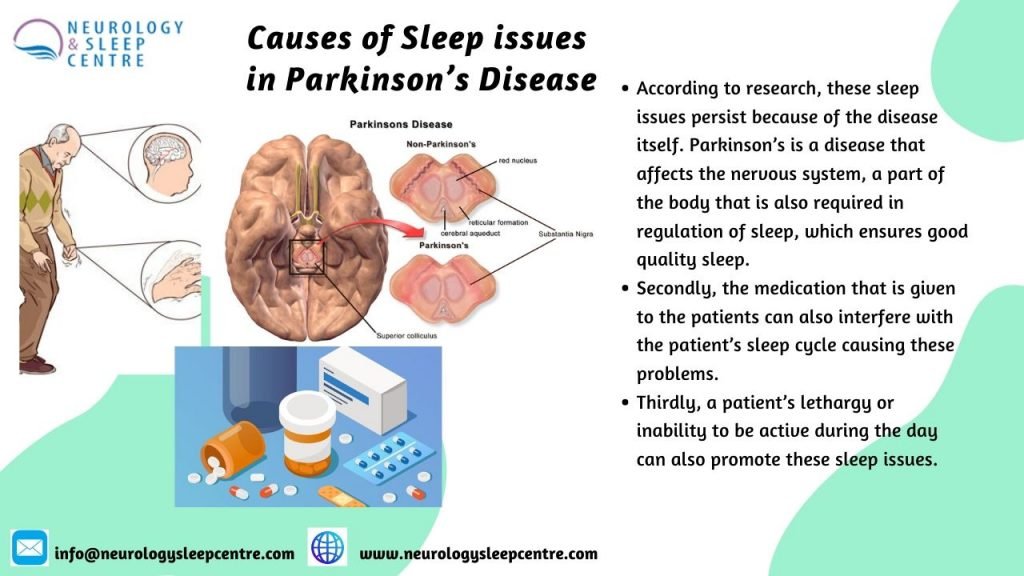
SAN ANTONIO — Roughly three out of four people living with Parkinson’s disease also have sleep disorders, and there is growing recognition that sleep problems are greatly complicated by the disease, its symptoms, and the many medications used to treat it.
“Sleep disorders are among the most common non-motor symptoms in PD, and sleep is something clinicians have to continually monitor when considering medication dosing,” Scott Kutscher, MD, of Stanford School of Medicine in California, told MedPage Today.
“Sleep issues can appear years before the classic motor symptoms of Parkinson’s, but it has only been relatively recently that sleep has become part of the diagnostic workup of the disorder,” he added.
Insomnia, excessive daytime sleepiness, sleep fragmentation, circadian rhythm disorders, restless leg syndrome, and rapid eye movement behavior disorder are all common in patients with Parkinson’s disease.
Although there is some debate about whether having PD increases the risk for obstructive sleep apnea , a recent review of the literature found an increased frequency of OSA and other sleep-disordered breathing conditions associated with the neurodegenerative disorder.
One mechanism suggested for this association is that upper airway musculature may be affected by involuntary movements characteristic of the disease, resulting in abnormal spirometry and upper airway obstruction.
Diagnostic Assessment Of Sleep Disorders In Pd
The history taken from the patient and its neighbors is very important in assessing sleep disorders in PD. The type of sleep disorder should be identified in the history, and information about possible related factors should be obtained from the history. In PD, general and specific scales can be used to investigate the subtype of sleep disorder and to determine its severity. Objective methods can be used to further investigate the diagnosis of these disorders. Further investigative techniques include sleep recording methods such as actigraphy or PSG. Polysomnographic findings of each sleep disorder have been explained in the relevant section. In addition, information about screening scales used in each sleep disorder has been described in the relevant section.
Actigraphy is an electrophysiological device that measures the movements of the patient during sleep by recording from wrist or ankle for many days. Actigraphy evaluates indirectly the circadian sleepwake patterns . It is especially used in circadian rhythm disorders or insomnia and prolonged daytime sleepiness .
How Are Sleep Problems Diagnosed In People With Parkinsons Disease
If youre having problems sleeping, sit down with your healthcare provider to discuss the issue in detail. Your provider will ask you questions to better understand your symptoms.
Be prepared to explain when sleep disruptions happen and how they affect your life. Keeping a sleep journal for a few weeks can help you remember the details.
If your provider suspects you may have a sleep disorder, they may recommend you have a sleep study. This overnight test uses electrodes attached to your skin to track how your body functions when youre sleeping.
You May Like: What Type Of Exercise Is Best For Parkinson’s
Why Do Parkinsons Patients Have Trouble Sleeping
Despite having daytime tremors, Parkinsons patients do not shake in their sleep. However, both Parkinsons disease itself and the medications used to treat it can give rise to a number of sleep problems that lead to insomnia and excessive daytime sleepiness.
Patients with motor symptoms may have trouble adjusting sleeping positions to get comfortable. Others may experience distressing nocturnal hallucinations when trying to fall asleep. These may be a result of medications or cognitive impairment.
In turn, excessive daytime sleepiness may occur as a consequence of sleeping poorly at night. It may also be triggered by medications. Parkinsons patients who suffer from EDS may be at a higher risk of accidents and unable to safely carry out activities such as operating a motor vehicle.
Since insomnia frequently goes hand-in-hand with anxiety and depression, it may be a contributing factor to sleep problems in people with Parkinsons disease. For that reason, doctors often look for mental health disorders in people with Parkinsons disease who have sleep problems.
Restless Legs Syndrome And Periodic Limb Movements Of Sleep

Restless legs syndrome usually occurs as one is trying to fall asleep and is characterized by an unpleasant, restless feeling that is only relieved by moving the legs. Periodic limb movements of sleep are rhythmic moving or jerking of the limbs during sleep.
Both RLS and PLMS affect the quality and quantity of sleep. Medications are available that can help these syndromes. Some people also experience relief with an increase in dopaminergic treatment.1
You May Like: What Are The Stages Of Parkinson’s Disease
Associations Of Insomnia And Subjective Sleepiness With Specific Pd Features And Comorbidities
For the 128 subjects, insomnia severity as reflected by ISI score correlated significantly with age, levodopa equivalent dose, Beck Depression Inventory, Trait Anxiety Score, Fatigue Severity Scale, Survey of Autonomic Symptoms, 39-item Parkinson Disease Questionnaire, and parts I and II subcategories of the MDSUPDRS . Daytime sleepiness as assessed by the ESS was significantly correlated with Hoehn and Yahr stage, duration of illness, levodopa equivalent dose, Beck Depression Inventory, trait score of State Trait Anxiety Inventory, Fatigue Severity Scale, Survey of Autonomic Symptoms, 39-item Parkinson Disease Questionnaire, and each of the 3 assessed components of the MDS-UPDRS. Subjects who were taking dopamine agonists alone and those who took levodopa alone showed no significant differences in ESS scores. The ISI and ESS scores were moderately correlated with each other.
Table 2 Correlation of subjective sleep questionnaire and objective polysomnographic findings with age and measures of Parkinson disease or related symptom severity
|
Table 2 Correlation of subjective sleep questionnaire and objective polysomnographic findings with age and measures of Parkinson disease or related symptom severity |
Table 3 Results of multivariate stepwise logistic regression of insomnia symptoms or sleepiness on specific Parkinson disease features and comorbidities
Diagnosis Of Insomnia In Pd
In the diagnosis of insomnia in PD, the clinical history including the stages of insomnia and its associated factors are essential. For example, the factors associated with initial insomnia should be learned from the clinical history because the identification of factors associated with insomnia is necessary for the treatment plan. Table 2 shows the factors associated with insomnia . For example, for the diagnosis of RLS, as a reason for the difficulty of falling into sleep, clinical assessment is sufficient. Thus, patients should be asked for the features in the definition mentioned below for the diagnosis of RLS . In contrast to idiopathic RLS, family history of RLS is less frequent in PD . Polysomnography and actigraphy can be used to detect the objective findings of the insomnia . It has been reported that insomnias PSG findings may be an increase in the number of brief EEG arousalsor arousal index, number of stage shifts to stage 1 or wake, wake time after sleep onset , and percentage of stage 1 sleep . The actigraphic findings of insomnia include the presence of irregularity in sleep onset and increased number of awakening times during the night . One review has been reported that studies comparing PSG to actigraphy in insomnia show that PSG and actigraphy have no significant difference in showing the measurements of WASO, total sleep time , and sleep efficacy .
| Factors |
|---|
Recommended Reading: When Was Muhammad Ali Diagnosed With Parkinson’s Disease
Diagnosis Of Excessive Daytime Sleepiness In Pd
In patients describing the symptoms of EDS, it is very important to determine the level of sleepiness. The Epworth Sleepiness Scale is widely used in the evaluation of EDS. Thus, ESS is a useful scale for the subjective assessment of sleepiness in patients with EDS .The ESS contains eight items, and each item is rated as maximum three points. A higher score means more sleepiness level. In addition, there are objective tests such as multiple sleep latency test and maintenance of wakefulness test for assessment EDS. The MWT is evaluation used as a polysomnographic measurement of EDS. The MSLT is measured after a PSG performed in the night to assess nighttime sleep quality and quantity . One study found that the risk of traffic accidents increased in PD patients with an ESS score greater than 7 .
Insomnia And Sleepiness In Parkinson Disease: Associations With Symptoms And Comorbidities
Sleep Disorders Center and Department of Neurology, University of Michigan, Ann Arbor, MI
Department of Psychiatry, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Republic of Korea
Department of Radiology, Division of Nuclear Medicine, University of Michigan, Ann Arbor, MI
Department of Neurology, University of Michigan, Ann Arbor, MI
Department of Radiology, Division of Nuclear Medicine, University of Michigan, Ann Arbor, MI
Department of Neurology, University of Michigan, Ann Arbor, MI
Recommended Reading: What Cold Medicine Can You Take With Parkinson’s
Sleep Disorders In Parkinsons Disease
In this 17-minute lecture Dr Gary Leo discuses sleep challenges caused by the neurochemical changes, medications and mood disturbances of Parkinsons disease, and normal changes of aging. He discusses possible causes and treatment options of sleep maintenance insomnia, REM Sleep Behavior Disorder, daytime sleepiness, sleep apnea, and restless leg syndrome, ending with some tips for good sleep.
What Types Of Sleep Problems Do People With Parkinsons Disease Have
Parkinsons disease affects every person differently. It also impacts sleep in different ways. People with Parkinsons may have:
- Insomnia, finding it hard to fall asleep.
- Fragmented sleep, waking up many times over the night.
- Excessive daytime sleepiness, finding it hard to stay awake during the day.
- Very vivid dreams, which may cause hallucinations or confusion after waking up.
- Emotional dreams or nightmares, which may make you feel emotionally drained after waking up.
Don’t Miss: What Are The Symptoms Of Early Onset Parkinson’s
Parkinsons Sleep Problems: Diagnosis And Treatment
Parkinsons disease is chronic and progressive, meaning it tends to get worse over time. However, there are treatment options that can help manage symptoms and allow patients to get more restful sleep.
The simplest way to start sleeping better with Parkinsons disease is by adopting healthy sleep habits. Sleep hygiene tips for Parkinsons disease sufferers include:
- Sticking to regular bedtimes
- Following a consistent bedtime routine with soothing activities such as listening to music or reading a calming book
- Getting regular exercise, preferably early in the day
- Getting adequate exposure to light, whether outdoors or through light therapy
- Avoiding long naps and naps late in the day
- Creating a cool, dark, and comfortable sleeping environment
- Restricting bedtime activities to sex and sleep only
- Turning off screens an hour before bedtime
- Reducing liquid intake before bedtime
- Avoiding caffeine, alcohol, and tobacco
- Eating a healthy diet and avoiding large meals at night
Light therapy, exercise, and deep brain stimulation have been successfully used to improve overall sleep quality and to treat specific conditions, such as REM sleep behavior disorder, in patients with Parkinsons disease. Cognitive behavioral therapy for insomnia has proven effective at reducing insomnia in healthy adults, although further research is needed on the effects of CBT in patients with Parkinsons disease.
- Was this article helpful?
Classification Of Sleep Disorders In Parkinsons Disease
Sleep disorders in PD may occur during the day or at night. In PD, sleep disorders can be classified into three major categories such as abnormal behaviors and events during or around sleep , inability to sleep , and EDS . These three categories of sleep disorders can be seen separately or together .
| Categories |
|---|
| NREM parasomnias |
| Inability to sleep/sleeping difficulty |
|
|
|
Recommended Reading: What’s The First Sign Of Parkinson’s Disease
Stooping Or Hunching Over
Are you not standing up as straight as you used to? If you or your family or friends notice that you seem to be stooping, leaning or slouching when you stand, it could be a sign of Parkinson’s disease .
What is normal?If you have pain from an injury or if you are sick, it might cause you to stand crookedly. Also, a problem with your bones can make you hunch over.
The Different Stages Of Sleep
- Rapid eye movement sleep
- Non-rapid eye movement sleep
The lightest stage of sleep is NREM, after which comes deeper sleep states. As people move back through to the lighter stages, they enter the REM state. If awoken during REM sleep, the sleeper will often report a dream.
Also Check: Are There Any New Drugs For Parkinson’s
Whats The Relationship Between Parkinsons And Sleep
Parkinsons disease and sleep are connected in complex ways that not even scientists completely understand quite yet.
Sometimes, Parkinsons disease directly causes sleep problems. According to one study, sleep-related symptoms may be one of the earliest signs of Parkinsons disease. These signs may include things like thrashing while youre asleep.
Other factors can also play a role. One thing is clear: For many people with Parkinsons disease, a restful nights sleep can be hard to find.
Parasomnias In Parkinsons Disease
In PD, parasomnias are quite common, and REM parasomnias are more common than those in NREM . As REM parasomnia in PD, RBD can be seen in near two-thirds of patients . In PD, non-NREM parasomnias can include sleepwalking, confusional arousals, and sleep terrors. However, NREM parasomnias are not a frequent cause of sleep disorders in PD .
Read Also: How Long Does It Take For Parkinson’s Disease To Progress
Why Do Parkinsons Patients Sleep So Much
Parkinson’s patients experience difficulties with their sleep due to the disease itself and the medications that treat it. This can lead to increased sleepiness during the day.
Parkinsons disease can cause problems with sleep, and the medications used to treat it can cause even more. Difficulties sleeping during the night can cause daytime sleepiness, and the medications can also cause drowsiness. This disruption to the circadian rhythms can lead to more frequent, lower quality sleep.
Sleep Problems At Later Stages Of Pd
In addition to the conditions already mentioned, during the later stages of PD, you also may experience sleep problems related to higher doses of medications, such as hallucinations.
As many as 33% of Parkinson’s patients during mid and later stages of the disorder experience hallucinations, related to medication side effects. Hallucinations tend to occur visually rather than hearing them . They are frequently associated with vivid dreams.
- Cartwright, R. . Dreaming as a mood regulation system. In: Principles and Practice of Sleep medicine. 4th edition, ; pps 565-572.
- Kumar, S., Bhatia, M., & Behari, M. . Sleep disorders in Parkinson’s disease. Mov Disord, 17, 775-781.
- Larsen, J. P., & Tandberg, E. . Sleep disorders in patients with Parkinson’s disease: epidemiology and management. CNS Drugs, 15, 267-275.
- Olson, E. J., Boeve, B. F., & Silber, M. H. . Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain, 123 , 331-339.
- Pappert, E. J., Goetz, C. G., Niederman, F. G., Raman, R., & Leurgans, S. . Hallucinations, sleep fragmentation, and altered dream phenomena in Parkinson’s disease. Mov Disord, 14, 117-121.
- Stacy, M. . Sleep disorders in Parkinson’s disease: epidemiology and management. Drugs Aging, 19, 733-739.
Read Also: What Tests Are Used To Diagnose Parkinson’s
Gait And Balance Problems
One of the most debilitating effects of Parkinsons disease is the loss of coordination and control in body movements, which in many cases leads to severe walking disabilities. Although gait symptoms can vary among patients, there are some commonly observed movements. These include a tendency to lean or stoop forward while walking, dragging and shuffling of feet, and a decreased arm swing.
How Is Daytime Sleepiness Treated

Consider making certain lifestyle modifications, such as:
- Establish good sleep hygiene, including a set bedtime and wake-up time.
- Get exposure to adequate light during the day and darkness at night.
- Remember indoor lighting may not be sufficient to promote a normal circadian rhythm.
- Avoid sedentary activities during the day.
- Participate in activities outside the home. They may help provide stimulation to prevent daytime dozing.
- Get physical exercise appropriate to your level of functioning, which may also promote daytime wakefulness. Strenuous exercise, however, should be avoided six hours before sleep.
- Do NOT drive while sleepy if you experience excessive daytime sleepiness. Motor vehicle accidents increase during periods of drowsiness and may be associated with sudden onset of sleep .
- Talk to your doctor about possibly decreasing the dosage of dopamine agonists if you experience daytime sleepiness or sleep attacks.
- Talk to your doctor about decreasing stimulants like caffeine, modafinil and methylphenidate .
Don’t Miss: How Does A Person With Parkinson’s Feel
Sleep And Parkinsons Disease
The Palo Alto Parkinsons Disease support group February 2020 meeting featured Dr. Emmanuel During, a Stanford sleep medicine neurologist. During the meeting, Dr. During discusses sleep disturbances that can occur in PD, such as insomnia, restles legs syndrome, sleep apnea, and REM sleep behavior disorder , along with available treatments. There’s a question and answer session.
Nighttime Hallucinations Psychosis & Confusion
Nighttime hallucinations and confusion may result from any combination of cognitive impairment, dopaminergic medications, age and PD-related vision changes and lack of sleep. Psychosis may first appear after infection, trauma, surgery or prolonged hospitalization. Symptoms may range from a sensation that someone or something is standing at the side of or behind the person, to very detailed and often frightening visions. Delusions may occur as well.
Treating Parkinsons Psychosis
The first-line approach to treatment of PD psychosis involves simplification of the anti-PD medication regimen and adjusting dose timing , treating other sleep disturbances, providing a consistent and familiar sleep environment , and in more severe cases, the use of atypical antipsychotic drugs.
Most of the available anti-psychotics are always avoided in PD psychosis because they block dopamine receptors and can cause significant problems with movement. However, two anti-psychotic medications, quetiapine and clozapine, are sometimes used as they have less of an ability to worsen motor symptoms. However, data for the use of quetiapine is limited and clozapine requires the patient to undergo frequent blood draws to monitor blood counts. A newer medication pimavanserin, was approved by the FDA to treat PD psychosis. It has a different mechanism of action, and does not block the dopamine system, but rather the serotonin system, and therefore does not increase motor symptoms.
Recommended Reading: Is There Genetic Testing For Parkinson’s Disease
Parkinsons Disease And Sleep: Common Symptoms
Sleep problems can occur at any stage of Parkinsons disease. Some of the most common sleep problems for PD patients include:
- Insomnia: Difficulty falling or staying asleep
- Excessive daytime sleepiness: Feeling drowsy or fatigued during the day. In Parkinsons, sleeping all day is also common
- Nightmares or night terrors: Bad dreams that seem unusual for you
- Sleep attacks: Sudden, involuntary episodes of sleep, also known as narcolepsy
- Periodic leg movement disorder
- Restless leg syndrome
- REM sleep behavior disorder: Acting out dreams while asleep
- Sleep apnea: When breathing becomes obstructed during sleep
- Nocturia: Frequent night-time urination
When prescribing one of the drugs I take, my doctor warned me of a common side effect: exaggerated, intensely vivid dreams. To be honest, I’ve never really noticed the difference. I’ve always dreamt big. Michael J. Fox
Memory Or Thinking Problems
Having issues with thinking and processing things could mean your disease is progressing. Parkinsons is more than a movement disorder. The disease has a cognitive part as well, which means it can cause changes in the way your brain works.
During the final stage of the disease, some people may develop dementia or have hallucinations. However, hallucinations can also be a side effect of certain medications.
If you or your loved ones notice that youre getting unusually forgetful or easily confused, it might be a sign of advanced-stage Parkinsons.
Recommended Reading: What Are The Four Cardinal Signs Of Parkinson’s Disease
Changes In Sleep With Aging
As people age, they experience a number of changes in their circadian rhythms, and among the most noticeable are the changes in the sleep-wake cycle. Older people tend to wake up earlier and go to bed earlier than they did when they were younger. They wake up more often during the night and have more difficulty going back to sleep than younger people. They also tend to sleep more during the daytime hours. Therefore, if one looks at total sleep time over the 24-hour day, the total time spent sleeping changes very little but the distribution of sleep may be quite different. Younger people experience a consolidated nighttime episode with little or no daytime sleep, whereas older individuals experience sleep episodes throughout the 24-hour day. Daytime sleepiness is affected by two major factors: the amount and quality of nighttime sleep, and the strength of the circadian rhythm. In addition, older people tend to have a reduced amount of N3 or deep slow wave sleep.
What Else Can I Do To Sleep Better With Parkinsons Disease
Practicing healthy sleep hygiene habits may also promote more restful sleep.
- Get outside during the day. Bright light tells your body its time to be awake.
- Keep your body moving during the day. Even if all you feel up to is a short walk or two, all physical activity offers benefits.
- Try at-home remedies, such as massage or a warm bath. Relaxing your mind may help your body fall asleep.
Dont:
- Take long naps during the day.
- Use stimulants, such as caffeine, within six hours of bedtime.
- Use your bedroom for activities other than sleeping. Go to another room to read, watch TV or work.
Don’t Miss: Does Parkinson’s Cause Depression
Sleep: A Mind Guide To Parkinsons Disease
This 36-page booklet explains normal sleep patterns, the body clock, how much sleep we should get, challenges to sleeping well, tips for good sleep hygiene, and sleep in normal aging before discussing symptoms, diagnosis and treatment of sleep disorders, including insomnia, REM sleep behavior disorder, sleep apnea, restless leg syndrome, and daytime sleepiness.
Parkinsons Disease And Sleep Problems: Symptoms Treatments

Parkinsons disease and sleep issues affect around 75% of patients. Despite the importance of sleep when dealing with a long-term illness, most people with PD experience sleep issues at some stage of their condition. Sleep problems often occur long before motor symptoms have begun, making them one of the first signs of Parkinsons disease. Some of the most common sleep problems in PD are insomnia, restless leg syndrome and excessive daytime sleepiness. Parkinsons can also cause night-time disturbances such as sleep apnea, bad dreams and frequent night-time urination. Let’s explore Parkinson’s disease and sleep problems in more detail.
Don’t Miss: How Do Parkinson’s Tremors Start
Increased Feelings Of Anxiety Or Depression
Anxiety and depression have been linked to Parkinsons. In addition to movement problems, the disease can also have an impact on your mental health. Its possible that changes in your emotional well-being can be a sign of changing physical health as well.
If you are more anxious than usual, have lost interest in things, or feel a sense of hopelessness, talk to your doctor.
The Relationship Between Parkinsons Disease And Sleep
Its unclear whether poor sleep causes parkinsonian symptoms to worsen or whether worsening parkinsonian symptoms cause poor sleep. In many cases its likely a case of bidirectionality, with each one exacerbating the other.
Fragmented sleep and sleep deprivation appear to leave the brain more vulnerable to oxidative stress, which has been tied to the development of Parkinsons disease. Parkinsons disease is not usually diagnosed until individuals have developed sufficient motor symptoms, by which time a significant portion of brain cells have already been damaged. If poor sleep quality or having sleep disorders foreshadows the development of parkinsonian symptoms, these could be useful in early diagnosis of the disease.
More research is needed to clarify the multifaceted relationship between Parkinsons disease and sleep. A better understanding of this connection may offer medical experts the unique opportunity to screen at-risk individuals and perhaps delay the onset of the disease.
Also Check: Can Lyrica Cause Parkinson’s
