What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
Recommended Reading: Beginning Of Parkinsons Symptoms
Developing A Holistic Approach
Utilising the principles of end of life care highlighted earlier in section 2.4 of this course, we will examine how to effectively manage and guide the person with Parkinsons, and those closest to them, through this end stage with the minimum of distress.
Promoting holistic assessment which respects the autonomy and choice of the person with Parkinsons is important and involves them in planning their end of life care through early discussions about advance care planning and Advance Decision to Refuse Treatment , as discussed in section 3.3
Holistic assessment in the end of life stage focuses on the physical, psychological, social and spiritual aspects of care for the person with Parkinsons. We will examine these in greater depth.
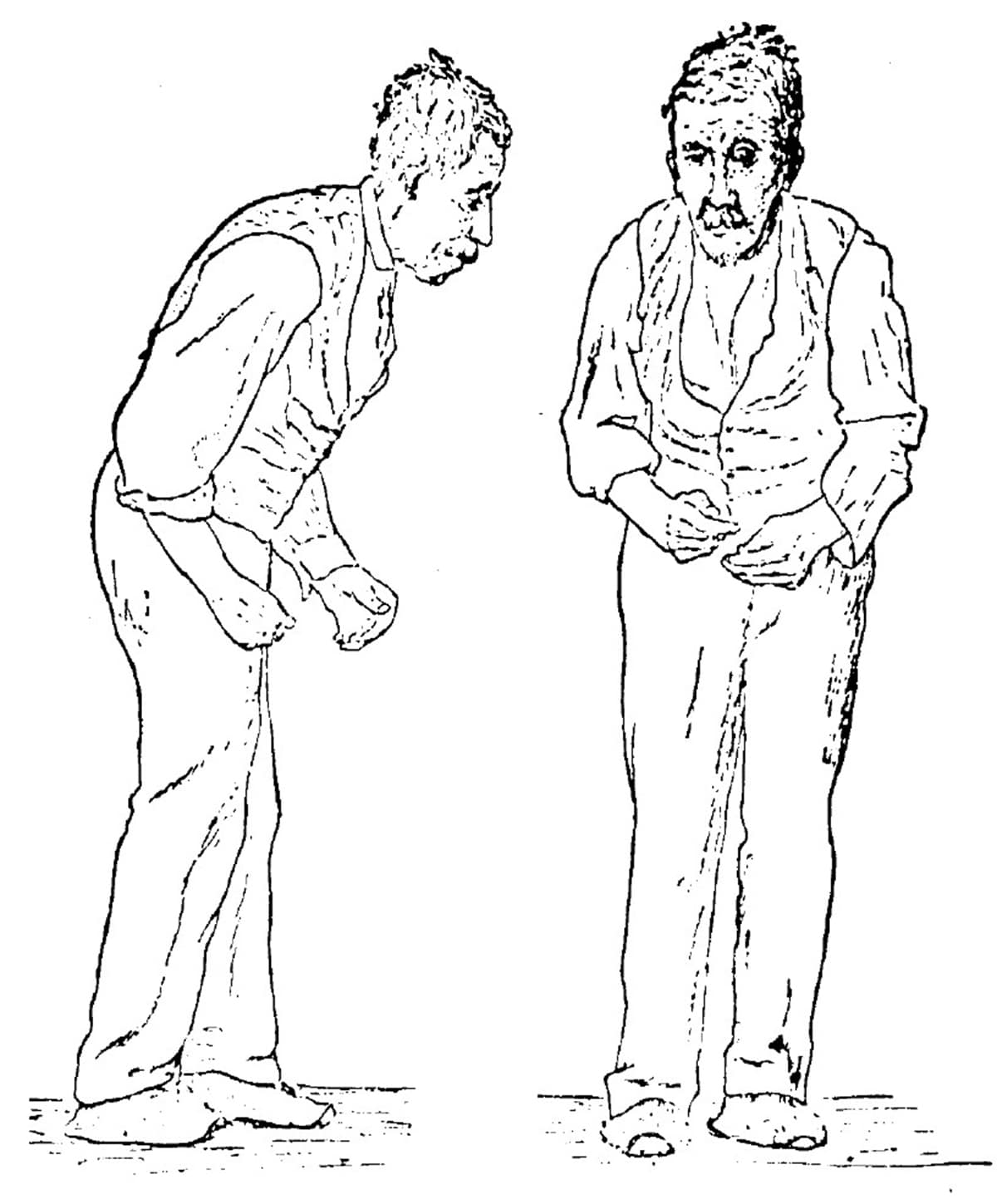
Stages Of Parkinsons Disease
While there may be no cure, Parkinsons follows a predictable path. In the early stages, symptoms are mild and inconvenient by the end stages, symptoms are incapacitating.
- Stage One: Patients begin to experience tremors on one side of the body. One arm or leg will feel heavy, but not to the point it interferes with daily life. Symptoms may be so slight, they can be sometimes overlooked.
- Stage Two: Symptoms are clearly visible and affect both sides of the body. Patients become stooped as tremors grow more pronounced. Muscles are rigid, making it difficult to bend their trunk, arms, and legs facial muscles begin to freeze at this stage, creating an almost mask-like appearance. At this stage, however, balance is not yet impaired, so most patients continue to live independently.
- Stage Three: Balance becomes increasingly compromised, and reflexes and coordination deteriorate, elevating serious risks of falling. Muscles grow so stiff that patients can only take short, shuffling steps. Tremors become more serious, and yet most patients can still complete daily tasks, though it requires more time and greater effort.
- Stage 4: Patients can no longer live on their own. Balance is so weak that while it may be possible for them to stand, they will not be able to move without a walker. Some freeze periodically, unable to move for short periods of time.
- Stage 5: Patients cannot walk or stand without assistance and require round-the-clock care.
Also Check: Parkinsons Disease Fun Facts
Also Check: What Causes Tremors Besides Parkinson’s
Palliative Care As An Option
If your loved one is not eligible for hospice, the good news is that they can still receive palliative care. This type of care focuses on alleviating symptoms, discomfort, and stress associated with any illness, including PD.
The main difference between palliative care and hospice is that palliative care can be given along with standard treatments, including therapies intended to prolong life.
When Should You Start Palliative Care For Parkinsons
You can start palliative care for Parkinsons at any time. Palliative care can help anyone who has a complex and progressive condition like Parkisons.
Although many people wait until their condition has progressed or until they are in the later stages of Parkinsons to seek out an option such as palliative care, you might get more benefit from starting this care earlier.
That way, youll have a supportive team with you over the years that can help you manage your diagnosis.
Read Also: When To Start Medication For Parkinson’s
Study Designs And Descriptions Of Included Studies
The 42 studies were published until February 2020. The study designs were: retrospective cohort studies, prospective cohort and longitudinal studies, casecontrol studies and cross-sectional studies. Predictors of mortality included demographic and clinical markers, medical events, medication changes, disease-specific symptoms and patient and caregivers ratings of health-related quality of life. Eight studies described both predictors of mortality and causes of death.
Caring For A Person With Advanced Parkinsons Disease
In this 47-minute webinar Anne Wallis, Associate Director of Education at the Parkinsons Foundation, talks with doctor of physical therapy, Sarah King, about when to look for outside help, how to lasso the power of your friends and family , and how to build an allied healthcare team that decreases your stress and improves your loved ones care.
Recommended Reading: What Is The Difference Between Parkinson’s And Parkinsonism
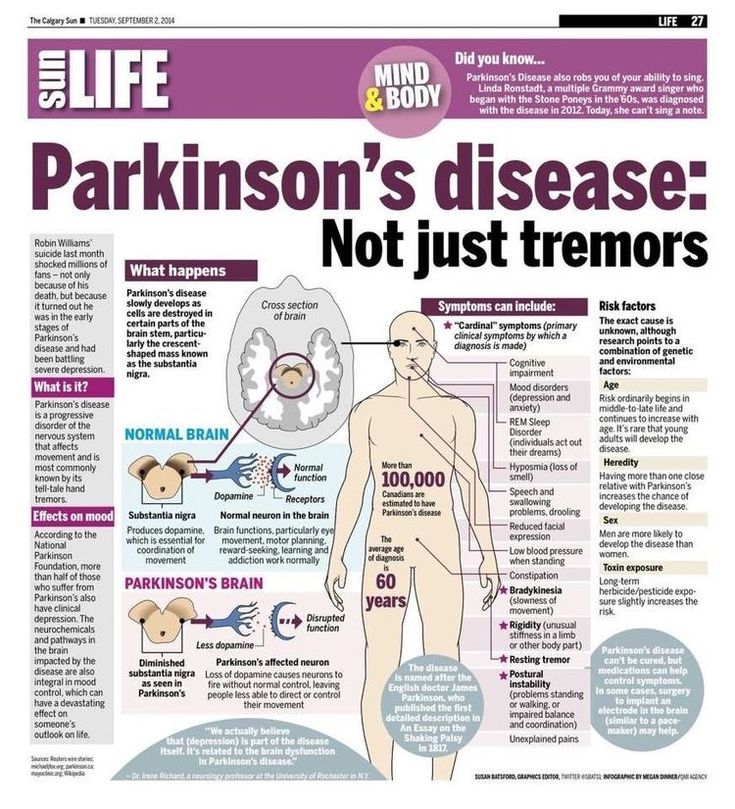
How Is Parkinson’s Managed
There is currently no cure for Parkinsons but there are medications and therapies that can help to manage Parkinsons symptoms.
Medicines that increase the level of dopamine in the brain are the main treatment used to manage the symptoms of Parkinson’s. Medicines are tailored to each individuals needs.
Symptoms will get worse when someones Parkinsons medicines are wearing off and improve again after Parkinsons medicines are taken. If people with Parkinsons do not get their medication at the right time, it leads to their motor symptoms becoming uncontrolled. It can take some time to get their symptoms under control again. If you work in a hospital or care home, it is important to be aware that medicine timings will vary from person to person and may be different to ward medicine rounds.
As well as medicines, surgical options are available for some people with Parkinson’s, depending on their symptoms.
Treatments can help to manage the symptoms, but may become less effective in the later stages of the condition.
Parkinsons UK has more information on how Parkinsons affects people and how it can be managed.
Managing The Terminal Phase
When the terminal phase can be anticipated by an acceleration in the patients global deterioration, a decision may have been taken with the patient and family not to treat further episodes of infection. A careful check for specific symptoms should be sought from the patient directly or from observing the patient for any signs of distress. Close family members will often recognise signs of unspoken distress. The views of experienced clinical staff may determine if the patient is frightened, in pain or has different nursing requirements.
For patients unable to swallow in the terminal stage, medication can be administered subcutaneously as needed or continuously using a syringe driver. Medication can be given, if necessary, to relieve specific symptoms as follows:
-
midazolam for fear or agitation
-
hyoscine butylbromide for drooling or chesty secretions
-
morphine for pain
If pain is present, a sufficient dose of morphine should be used to relieve it but without causing undesirable opioid side effects.
You May Like: Best Exercise Equipment For Parkinson’s
Hospice Care For Late Stage Parkinsons
There are a number of reasons why choosing to have home health care services for Parkinson patients is one of the best options. Hospice care for late stage Parkinsons is extremely important.
- End of Life 40% of those who were in a long term care facility died alone without a family member being with them. Every person in the study listed who had in home health care and hospice had at least 1 significant family member or loved one with them at the time of their passing.
- Satisfaction 83% of those who utilized hospice were satisfied to highly satisfied with their experience. They cited their satisfaction with the ability to handle the extreme grief and handling of the symptoms of the disease as two of the main reasons for being appreciative with the care received.
- Focus Hospice care for late stage Parkinsons focuses on comfort care, symptom care, grief counseling and acceptance. Maintaining a level of understanding and comfort for both the patient and their loved ones is a primary goal.
We can see the importance of a loved one remaining at home as they battle PD, especially as they move towards the final stages of the disease. Above & Beyond Home Health Care can be there for you with professional hospice care for late stage Parkinsons so you know that your loved one is provided for with the best care possible.
Cited Works:
End of Life Care for a Person with Parkinson Disease Dept. of Education
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinsons disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinsons disease.
The overlap in symptoms between Lewy body dementia and Parkinsons disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinsons disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinsons disease itself isnt fatal, but complications can be.
Research has shown a median survival rate of about
Don’t Miss: What Are The Symptoms Of Early Onset Parkinson’s Disease
What Is Advance Care Planning
The above diagram represents the topics covered during an ACP discussion.
This is an ongoing process of discussion between the person with Parkinsons, those closest to them and their health and social care professionals, focusing on the persons wishes and preferences for their care over the conditions trajectory and as they approach the end of their life.
NHS Scotland has also produced an Anticipatory Care Planning Toolkit.
Documentation of ACP
It is important that you are sensitive to the persons feelings and desires to have this conversation and so should avoid following a prescriptive method of interviewing and recording these discussions.
There is no set format for making a record of ACP discussions, but some health trusts and charities may be able to provide an informal document for the individual to use.
For example Gold Standards Framework provides guidance information and direction on ACP and this includes a document that allows the person to record their preferences and priorities for their future care.
The ACP is not a legally binding document, but must be taken into account when acting in the persons best interests.
It must be reviewed and updated as the individuals situation or views change. In accordance with the clients wishes a copy of the ACP may be held in the clients healthcare/electronic notes. The GP and family may be aware of the contents and where it is stored.
The timing and context of ACP
Reflective exercise
Case study
Recognising The Needs Of Carers
Caring for a person with Parkinsons, a long-term progressive condition, can be overwhelming and research has documented that carer burden may result in depression, stress, fatigue and even mortality .
Research indicates that carers for people with Parkinsons play an important role in the end of life care and death at home. Research also reveals unmet palliative care needs such as lack of information, ad hoc delivery of services and carers being unprepared for the stress and physical strain encountered at the advanced stage, and some carers being unprepared for death .
Carers of people with Parkinsons have been found to have fewer social contacts, fewer opportunities to socialise and tend to experience poor health. Changes in relationships, conflicting needs of the person and carer, communication problems, financial problems and fears about the future are all common issues experienced by carers of people with Parkinsons.
Reflective exercise
Use your reflection log to reflect on the following case study and identify the needs of the carer. In your reflection identify how to meet these needs.
Case study
Mr Thompson is an 86-year-old man who was diagnosed with Parkinsons 15 years ago. He is married and lives with his 80-year-old wife, who is his main carer.
Mrs Thompson has found this very stressful. Due to her age and personal ill health she has been finding it more difficult to manage her husband at home.
Discussion
4.8.2 Bereavement care
Recommended Reading: Is Frozen Shoulder An Early Sign Of Parkinson’s
Management Of Social Care
When someone faces diagnosis and then the progression of a life limiting condition, many psychosocial issues will arise. These may include fears around diagnosis and an uncertainty about their future, with loss of independence and losing their role within the family. They may have anxieties about finances, about their independence and finally a fear of developing dementia.
Management of these changes both physical and mental will require early identification and an impeccable assessment with prompt referral to the appropriate team or professional.
The family and/or carers will require support from social services, carer support groups and Parkinsons support groups. Signposting to charities that provide support, education and guidance is also advisable.
Dont Miss: Symptoms Of Parkinson Disease Webmd
My Parkinsons Story: Advanced Parkinsons
This 10-minute video alternates between an interview with a man and his wife and his palliative care team, including a doctor, nurse, clerg and social worker. The man and his wife shares his experience with late stage Parkinsons. The palliative care team explains that their job is to support the best physical, emotional and spiritual wellbeing of the immediate family as well as help the family make end of life decisions.
Also Check: What Happens In Late Stages Of Parkinson’s Disease
Why Are We Here
Before we start, lets think about reasons for studying this course about Parkinsons palliative and end of life care. You might have decided to take this course for one or more of these reasons:
- You are working as part of the specialist team to support a number of people with Parkinsons.
- You feel you could do a better job if you understood palliative and end of life care.
- Your expertise is in palliative and end of life care, but you have limited experience of Parkinsons.
- Your manager told you to take this course.
- You want to increase your knowledge around Parkinsons to learn more about specific topics.
As much as possible we have designed the course to support those different contexts. Please remember it is your responsibility to determine whether specific recommendations are relevant to your role, as many are aimed at the specialist team.
We have created a reflection log for you to record your thoughts when answering questions throughout the course. Remember there are no wrong answers here.
Reflective exercise
Use your reflection log to answer the following questions:
What Are The Important Points Regarding Apomorphine At The End Of Life
Apomorphine is a dopamine agonist, which is given as a subcutaneous infusion either continuously or intermittently and also as single subcutaneous injections. An overview of studies into apomorphine use shows improvement in motor off periods and in dyskinesias.39
Apomorphine has side-effects similar to other dopaminergic medication but also notably nausea and vomiting. Ondansetron is not recommended for nausea in patients using apomorphine due to adverse effects.21
Subcutaneous apomorphine has been used at the end of life in a patient with advanced PD although with the recommendation that this is by a healthcare professional experienced in its use.40
Also Check: Ot Interventions For Parkinson’s Disease
Parkinsons Disease: When Is It Time For Hospice
Knowing when its time for hospice care when living with Parkinsons Disease can be difficult as the disease may take many years to progress and each person with the disease may also exhibit a range of different symptoms. However, entering the end-stages of the disease , patients will have symptoms that will indicate that it is time to seek hospice assistance:
Behaviors Seen In Parkinsons Disease Dementia
As dementia progresses, managing disorientation, confusion, agitation, and impulsivity can be a key component of care.
Some patients experience hallucinations or delusions as a complication of Parkinsons disease. These may be frightening and debilitating. Approximately 50 percent of those with the disease may experience them.
The best thing to do when giving care to someone experiencing hallucinations or delusions from Parkinsons disease dementia is to keep them calm and reduce their stress.
Take note of their symptoms and what they were doing before they exhibited signs of hallucinating and then let their doctor know.
This element of the disease can be particularly challenging for caregivers. Patients may become unable to care for themselves or be left alone.
Some ways to make caregiving easier include:
- sticking to a normal routine whenever possible
- being extra comforting after any medical procedures
- limiting distractions
- using curtains, nightlights, and clocks to help stick to a regular sleep schedule
- remembering that the behaviors are a factor of the disease and not the person
Recommended Reading: What Medications Cause Parkinson Like Symptoms
