Combination Of Pen And Paper And Computer
Several CT programs over the last decade have also utilized a combination of pen and paper and computer-based delivery. París et al. were the first to conduct a study of CT in PD in which a control group received a placebo intervention . In this study, over the course of 4 weeks, the experimental group received 12 × 45 min CT sessions using interactive multimedia software , as well as weekly paper and pencil-based homework exercises and a weekly tutoring session. The control group received speed therapy. Following the intervention, the CT group significantly improved in several cognitive domains . However, there were no significant improvements in ADL or self-rated QoL , suggesting that, while CT may be beneficial for improvements on specific neuropsychological tests, these skills may not generalize to improvements in everyday functioning. Similarly, in a study investigating the effects of CT specifically targeting prospective memory , Costa et al. utilized a combination of pen and paper and computer-based tests, finding the intervention improved performance on measures of executive function however, generalizability was not assessed across other domains. It is difficult to comment on the acceptability of combined programs in the PD population from these studies alone however, their investigations suggest the need for future studies utilizing this combination of techniques.
Table 2. Summary of Cognitive training in Parkinsons disease study outcomes.
Cognition And Mood And How To Manage Them
In this 50-minute webinar Greg Pontone, MD, distinguishes the cognitive changes commonly seen in those with dementia from the cognitive changes seen in Parkinson’s disease . He shares medications used to treat dementia and highlights those that are more effective for the cognitive changes in Parkinson’s. Dr. Pontone also talks about depression and anxiety specifically, the impact depression has on quality of life, and meditations to treat it, and how increased feelings of anxiety can be directly related to the wearing-off of medications.
The Use Of Adaptive And Assistive Technology To Deliver Ct In Pd
To date, the vast majority of studies of CT in PD have typically used either a manual pen and paper approach or a computer-based approach with standard keyboard and mouse functionality. This may represent a substantial and under-addressed barrier for the successful implementation and assessment of CT in the population. In support of this, a 2010 survey found that nearly 80% of PC-users with PD have significant and severe difficulties using a computer due to their illness . In particular, muscle stiffness, inertia and tremor were frequent problems, resulting in significant-highly severe difficulties using a standard mouse and keyboard . This represents a significant barrier to the current technical delivery of CT in PD, potentially altering the successful evaluation of outcomes, as well as prospective benefits. Consequently, not only should commercially available CT programs be adapted to address the cognitive dysfunctions specific to PD patients, but technical implementation should also be approached in light of the restrictions imposed by the often-debilitating motor impairments. To address this concern, this may involve the use of currently available technologies for adaptation, or the optimization of new assistive technologies to aid in delivery.
Read Also: Parkinson’s Disease Home Exercise Program
Multimodal Delivery: Ct + Exercise
Exercise is a common non-pharmacological intervention for neurodegenerative diseases, particularly PD . Aerobic training is believed to promote neural rearrangement and, as such, may complement and enhance the efficacy of cognitive rehabilitation programs. While the cellular mechanisms via which these neuroplastic effects occur are still unclear, they may involve enhanced neurogenesis/synaptogenesis or increases in myelination . Physical exercise leads to increased levels of neural growth factors, including BDNF), which is essential for facilitating neurogenesis, cell survival and SP . Thus, physical exercise may promote neurogenesis/synaptogenesis and CT may promote the survival of these cells and synapses . In support of this, several recent studies have reported beneficial effects when combining CT with aerobic exercise in schizophrenia .
Is There A Test To Diagnose Pd Dementia
There is no single test for PDD. The diagnosis is made clinically. If you or someone you spend time with notices cognitive changes, it is important to discuss them with your care team. If you dont have a care team in place, its important to find a specialist or physician familiar with dementia or geriatric medicine. Call the Parkinson’s Foundation Helpline 1-800-4PD-INFO for a referral.
Recommended Reading: Parkinson’s And Sleep Patterns
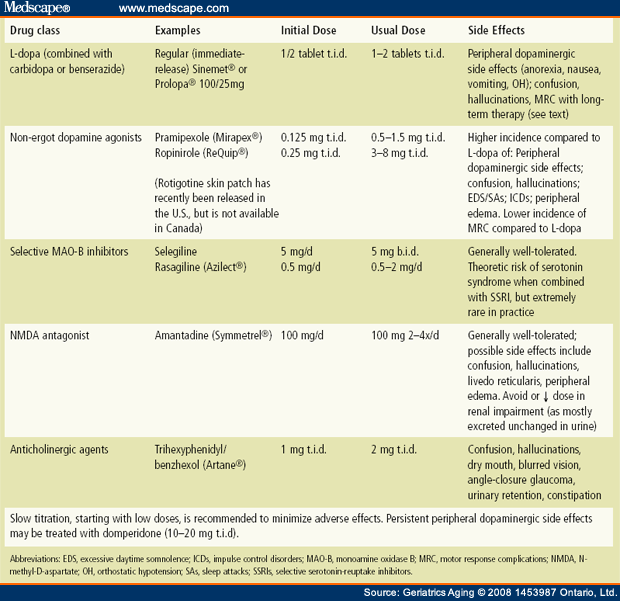
Pharmacologic Management Of Pd
To date, it is surprisingly slow in the advancement of therapeutic interventions specifically developed for PD-MCI. Not only that, but existing pharmacological and nonpharmacological measures have been identified to be typically marginal and nonsustained coupled with potential adverse effects.
As mentioned earlier, the pathogenesis of PD-MCI may involve the changes of cholinergic neurotransmitter, which may provide a theoretical basis for its pharmaceutical therapy. There is ample evidence that the disturbed cholinergic system may be the important cause of cognitive decline in patients with PD. Donepezil is the second acetyl cholinesterase inhibitor developed for improving cognitive function of PD patients, which has been approved by the FDA. It can selectively inhibit the degradation of acetylcholine in the central nervous system and effectively increase the concentration of acetylcholine in the synaptic cleft of nerve cells and delay progressive cognition impairment of PD patients with less adverse reaction and more obvious clinical safety and good tolerance. One clinical research trial has reported that cholinesterase inhibitors can benefit PD patients with cognitive impairment by significantly slowing the loss of Mini-Mental State Examination score, but the treatment with memantine does not work, both of which can improve the overall clinical symptoms of PD patients .
Predictors Of A New Cognitive Impairment Diagnosis
Table 3 depicts the results of the logistic regression evaluating factors associated with the identification of cognitive impairment. For the overall population, diagnosis of CVD and use of PD medication increased the odds of cognitive impairment by 24.0% and 46.0%, respectively. Enrollment in an MAPD plan increased the odds of having a cognitive impairment by 60.0% compared to those enrolled in a commercial plan . Furthermore, individuals eligible for both Medicare and Medicaid had a 36.0% higher chance to have cognitive impairment than individuals who were not dual eligible .
Table 3
Logistic Regression of Factors Associated With a New Diagnosis of Cognitive Impairment in Patients With Parkinsons Disease
| Parameter | Odds Ratio | Pr> ChiSq |
| Number of unique medications | 1.01 | |
| Use of Parkinsons disease medications | 1.46 | |
| Plan type | 1.60 | |
| Dual eligibility | 1.36 |
ChiSq, Chi square MAPD, Medicare Advantage and Prescription Drug plan Pr, probability.
Recommended Reading: What Is Dystonia In Parkinson’s Disease
Cognition Deficits In Parkinson’s Disease
Cognitive dysfunction is one of the major clinical nonmotor symptoms of PD with insidious onset, including mild cognitive impairment and dementia, especially for executive dysfunction with coexisting other cognitive domains impairment such as speech dysfunction, visual spatial ability, and memory impairment. Cognitive dysfunction is increasingly found prevalent in PD individuals and even in clinical newly diagnosed PD patients . Emerging epidemiologic study indicates that the cumulative prevalence of Parkinson’s disease dementia in 8 years is as high as 78.2% . Roughly 40% of PD subjects at an earlier stage have co-existing mild cognitive impairment, boosting the risk of converting to PDD . Cognitive deficits in PD has certain heterogeneity as described in Kehagia’s proposed dual syndrome hypothesis . PD with cognitive impairment can be divided into two broad categories: one is given priority to planning, working memory, and executive dysfunction that is related to the frontal lobe-striatum loop coupled with decreased dopamine levels and the other is disturbances of attention, semantic verbal fluency, and visual spatial ability with involvement of not only the temporal lobe but the posterior cortical dysfunction.
How The Brain Progresses With Pd
In this one-hour webinar movement disorder specialist Yasar Torres-Yaghi shared how the pathology of Parkinson’s disease begins in the gut before progressing to the brain. As the pathology expands throughout the brain it affects more neurotransnitters than just dopamine causing both motor and non-motor symptoms. Dr. Torres-Yaghi shares a widely used cognitive evaluation tool before answering questions about communicating well with your neurologist and advocating for the care you need.
Also Check: How Old Does Parkinson’s Start
Thinking Changes In Parkinson’s
In this 1-hour webinar Travis Turner, PhD, explains why you might be referred for a neuropsychological evaluation, what is done during such an evaluation, how the information learned during an evaluation is used, and tips for performing your best during an evaluation. After the talk he answered several questions about coping with cognitive changes when you have PD or are caring for someone with PD.
Prediction Of Cognitive Outcomes
Using records of cognitive diagnosis over an 8-year time period , we subset two cognitive outcomes. The first outcome tested development of overall cognitive impairment, including a group showing solely normal or subjective cognitive decline and another with development of MCI and Dementia . The second outcome tested dementia development comparing a dementia conversion group to a set of combined normal, SCD and MCI cases . Four ML algorithms were used for prediction using baseline variables, with each evaluated based on metrics of overall accuracy. Descriptive statistical summaries of each cognitive outcome group tested are shown in Table . Baseline variables were binned into individual subsets of genetic/epigenetic , biofluid , and clinical measures and tested individually and collectively. An overview of individual ML algorithm accuracy for each variable subset and outcome are summarized in Fig. and Table .
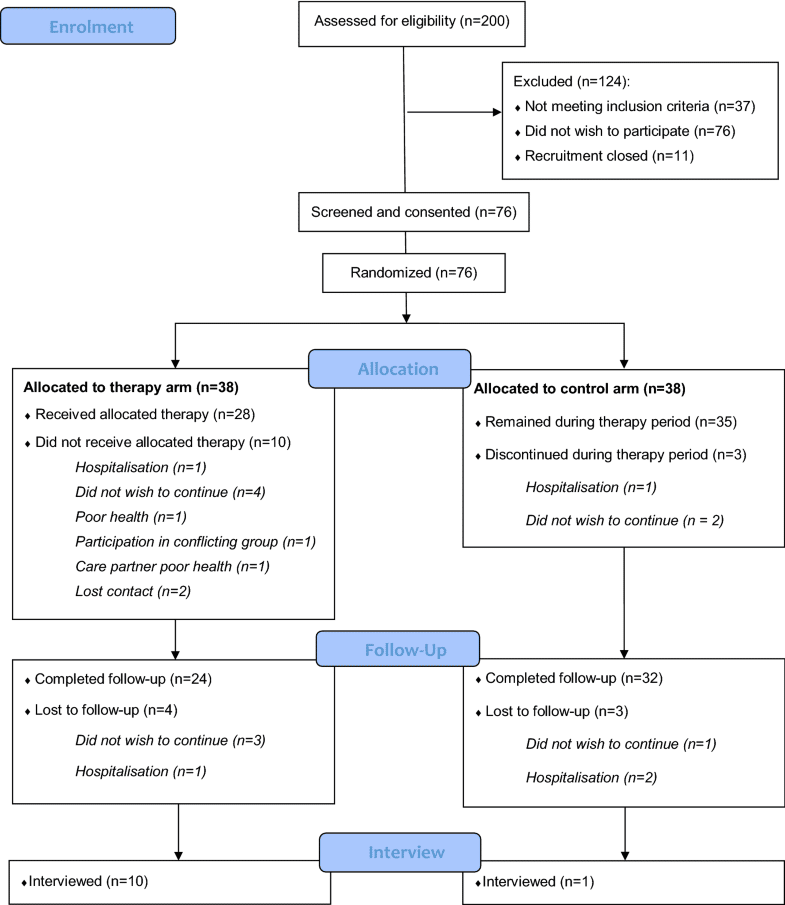
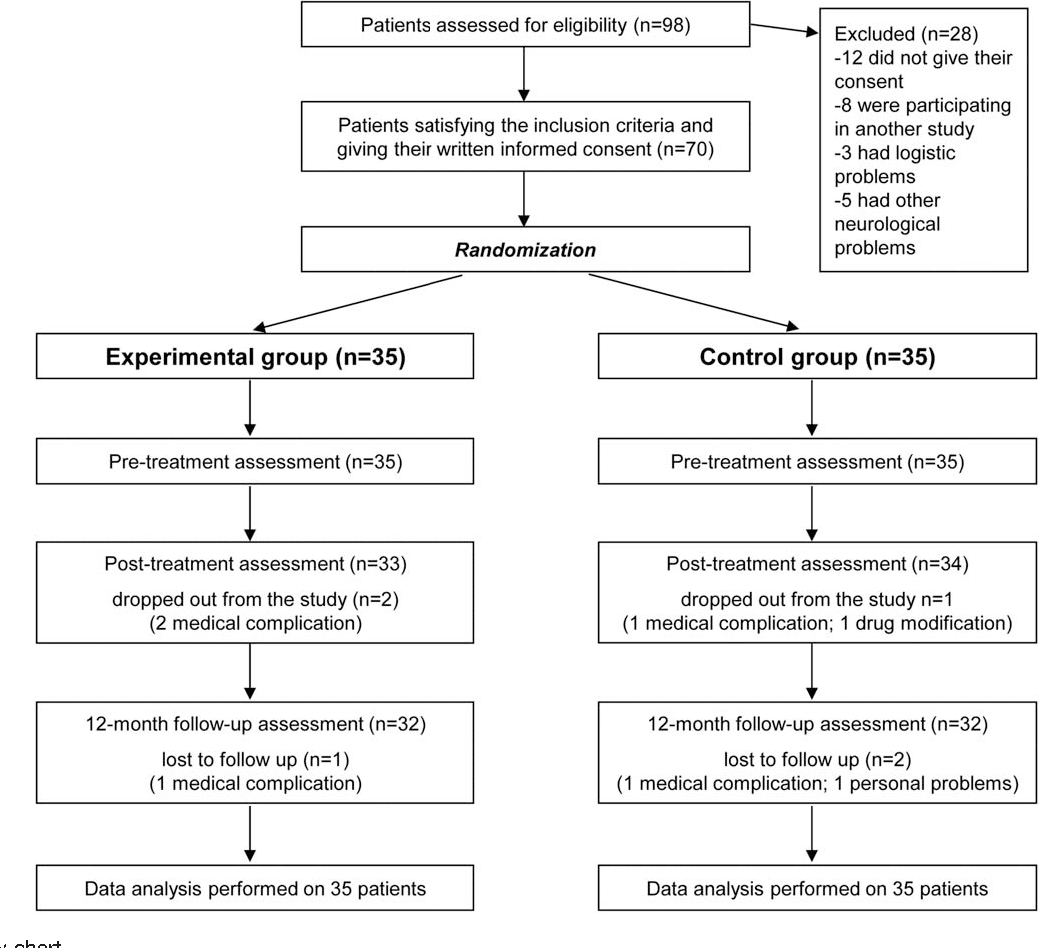
Fig. 1: Flow diagram of case subsetting criteria.
Samples retained in each stage are shown as black lines between boxes, samples excluded shown as dotted gray lines and boxes. Case numbers for each selection stage are shown overlaid on each plot. Final subset groups are shown at the bottom of the flow diagram. MDS Movement Disorder Society, MoCA Montreal Cognitive Assessment, MCI Mild Cognitive Impairment, SCD Subjective Cognitive Decline.
Also Check: What Part Of The Brain Is Affected By Parkinson’s Disease
Prodromal Pd Phenotypes And Conversion
Recent evidence suggests that individuals with prodromal features of PD, such as hyposmia , REM sleep behaviour disorder and reduced dopamine transporter binding, may present with worse cognitive performance compared with people without any or with only one of these features,,. Interestingly, prodromal PD and DLB may overlap and it is not yet known how to distinguish between those who will develop PD versus those who will develop DLB. Of note, cognitive deficit has been recently defined as a new prodromal marker and has been included in the last update of the research criteria for prodromal PD.
What Happens In Pdd
People with PDD may have trouble focusing, remembering things or making sound judgments. They may develop depression, anxiety or irritability. They may also hallucinate and see people, objects or animals that are not there. Sleep disturbances are common in PDD and can include difficulties with sleep/wake cycle or REM behavior disorder, which involves acting out dreams.
PDD is a disease that changes with time. A person with PDD can live many years with the disease. Research suggests that a person with PDD may live an average of 57 years with the disease, although this can vary from person to person.
Don’t Miss: Can Sleep Apnea Cause Parkinson’s Disease
Study Design And Data Source
This was a retrospective cohort study utilizing claims data for individuals with PD, enrolled in Humana, Inc.s Medicare Advantage and Prescription Drug or commercial health plans. MAPD plans are insurance plans offered to US consumers through private companies that cover medical and hospital services included under Medicare Parts A and B and include additional coverage not available in Medicare, typically including a prescription drug plan . Medicaid in the US is a jointly funded federal and state program that assists with medical costs for some individuals with limited income including eligible low-income adults, children, pregnant women, elderly adults, and individuals with disabilities . The study did not include individuals enrolled only in Medicaid but those eligible for both Medicare and Medicaid. Commercial insurance, which is either employer-sponsored or privately purchased, is defined as any type of healthcare ben-efit not provided by the government .
Patients with PD with and without cognitive impairment were matched on age and gender. The index date for the control group, PD without cognitive impairment, was based on the index date for the matched patient with cognitive impairment. Patients in all cohorts were 1989 years of age on the index date and were enrolled in a MAPD or commercial plan for at least 3 years pre- and post-index date.
Biomarkers Of Cognitive Decline
Many of the pathologies associated with cognitive impairment can be identified in vivo using a variety of imaging and blood-based or CSF-based markers. These biomarkers can be used to provide an increased understanding of the mechanisms underlying cognitive impairment in PD and, from a clinical perspective, can identify patients with an increased risk of early and rapid cognitive decline.
One of the first identified predictive markers was temporo-parietal atrophy on MRI , confirmed in many subsequent studies. In addition, basal forebrain atrophy observed using MRI is also associated with cognitive impairment in PD,. Hypometabolism in the medial frontal and parietal regions using FDG-PET is associated with a decline in executive and memory function. More recent MRI techniques, such as diffusion tensor imaging, also hold promise as biomarkers of cognitive function. For example, increased radial and axial diffusivity in the thalamus observed using diffusion tensor imaging was associated with a decline in MoCA scores.
Read Also: Best Jobs For Parkinson’s Patients
Background: Assessment Of Mild Cognitive Impairment
Cognitive decline is a common and disabling symptom of Parkinsons. It is vital that clinicians have clear guidance on its assessment. In response, this quick-reference clinical algorithm and series of supporting Critically Appraised Topics have been created.
Cognitive decline is a common and disabling symptom of Parkinsons. It is vital that clinicians have clear guidance on its assessment. However, the Evidence-Based Practice Thematic Working Group identified a lack of consensus across current guidelines about who should be assessed for cognitive symptoms, when, and how. The group felt that assessment was particularly challenging when there is a clinical suspicion of PD-MCI. To address these challenges, the group developed a convenient, quick-reference clinical algorithm.
The algorithm promotes shared, individually tailored decisions, based on thoughtful integration of best available evidence, clinical expertise, and an appreciation of how proactive the person with Parkinsons wishes their cognitive assessment to be.
The clinical algorithm also assesses whether cognitive symptoms impact performance of so-called instrumental activities of daily living – for example, managing personal finances, handling mail or using public transport. This provides a more meaningful assessment, with measures that can be monitored over time.
Cognition: A Mind Guide To Parkinsons Disease
This 52-page booklet offers coping strategies for people with cognitive changes due to Parkinsons disease, and their caregivers. The information, tips, and stories are intended to help organize thoughts and questions for your medical team. Read online, download the e-book, or order a physical copy.
Also Check: How Do Anticholinergics Work In Parkinson’s
The Future Of Ct For Pd
In addition to the recommendations above, in order to further improve the delivery and efficacy of CT programs, specific consideration should also be given to developing technologies that better adapt the CT platform to the unique needs and physical limitations of the PD population. One way this may be done is via multi-modal techniques, incorporating CT with interventions targeting the neural mechanisms that underlie cognitive function. Evidence in healthy aging supports this potential, with older participants who walked on a treadmill while playing a spatial navigation game demonstrating stability of hippocampal volume over a 4-month training period, whilst volumes in the control population deteriorated . Potential techniques identified that lend themselves to integration include transcranial Direct-Current Stimulation and exercise/aeorobic training.
Other Reasons For Cognitive Symptoms
Besides PD, there are other important causes of cognitive dysfunction to keep in mind. Medical illnesses such as thyroid disease or vitamin B12 deficiency can cause cognitive symptoms. Urinary tract infections or pneumonia can acutely cause confusion or hallucinations. In these settings, the cognitive symptoms are generally reversible after the infection or medical condition is treated. One should be aware that some medications for pain or bladder problems may cause sedation/sleepiness or confusion, and, thereby, impair cognitive function.
You May Like: Is There A Parkinson’s Gene
How Can We Support The Sleep/wake Cycle Of Pdd
For people with PDD who are confused about the day-night cycle, some daily strategies can be helpful. At night, starting a lights out routine that happens at the same hour every day, where all curtains are closed and lights are turned off, can help the person understand that it is sleep time. During the day, opening the curtains, allowing the person with PDD to spend as much time in the daylight as possible, avoiding naps, and organizing stimulating activities, can be helpful. Having lots of calendars and clocks in every room might also help a person with PDD be less confused about the time of day.
Tips For Communicating With A Person With Pdd
PD-related mood and motor changes can impact communication cognitive changes and Parkinsons disease dementia can further these difficulties.
- Stay calm and be patient. It is not usually helpful to try to reason or argue with someone experiencing a hallucination or delusion. If the person is frightened by the hallucination or delusion, try to redirect their attention to something else.
- Acknowledging what the person is seeing, even if you do not see it, can reduce stress.
- Speak slowly and at eye level. Communicate in simple sentences.
- Ask one question at a time and wait for an answer.
- Limit distractions. Turn off the TV or radio before asking a person with PDD to do something.
- Consider causes behind disruptive behavior. Can your loved one be hungry, thirsty, tired, in pain, frustrated, lonely or bored?
- If the person is stuck on an idea, try agreeing with them, then changing the subject.
- Its okay to use humor to diffuse stressful situations but avoid negative humor or sarcasm these can be misunderstood.
Page reviewed by Dr. Chauncey Spears, Clinical Assistant Professor and Dr. Sydney M. Spagna, Clinical Fellow at the University of Michigan.
Don’t Miss: Does Parkinson’s Affect The Mind

