Nighttime Hallucinations Psychosis & Confusion
Nighttime hallucinations and confusion may result from any combination of cognitive impairment, dopaminergic medications, age and PD-related vision changes and lack of sleep. Psychosis may first appear after infection, trauma, surgery or prolonged hospitalization. Symptoms may range from a sensation that someone or something is standing at the side of or behind the person, to very detailed and often frightening visions. Delusions may occur as well.
Treating Parkinsons Psychosis
The first-line approach to treatment of PD involves simplification of the anti-PD medication regimen and adjusting dose timing , treating other sleep disturbances, providing a consistent and familiar sleep environment , and in more severe cases, the use of atypical antipsychotic drugs.
Most of the available anti-psychotics are always avoided in PD because they block dopamine receptors and can cause significant problems with movement. However, two anti-psychotic medications, quetiapine and clozapine, are sometimes used as they have less of an ability to worsen motor symptoms. However, data for the use of quetiapine is limited and clozapine requires the patient to undergo frequent blood draws to monitor blood counts. A newer medication , was approved by the FDA to treat PD psychosis. It has a different mechanism of action, and does not block the dopamine system, but rather the serotonin system, and therefore does not increase motor symptoms.
Inclusion And Exclusion Criteria
The following inclusion criteria were used for study selection: Human studies; English language; OSA diagnosed by polysomnography ; use of case-control, cohort, cross-sectional or retrospective study design, sufficient background data for estimating the OR with 95%CI of PD and non-PD patients. Exclusion criteria were duplicate articles; data from case report, reviews or letters to the editor; subjects with ineligible general population controls ; criteria studies with patients that had neurodegenerative conditions, Parkinsonian syndromes, or Parkinsonism other than idiopathic PD.
Parkinsons Disease Linked To Sleep Disorders Sleep Disturbances
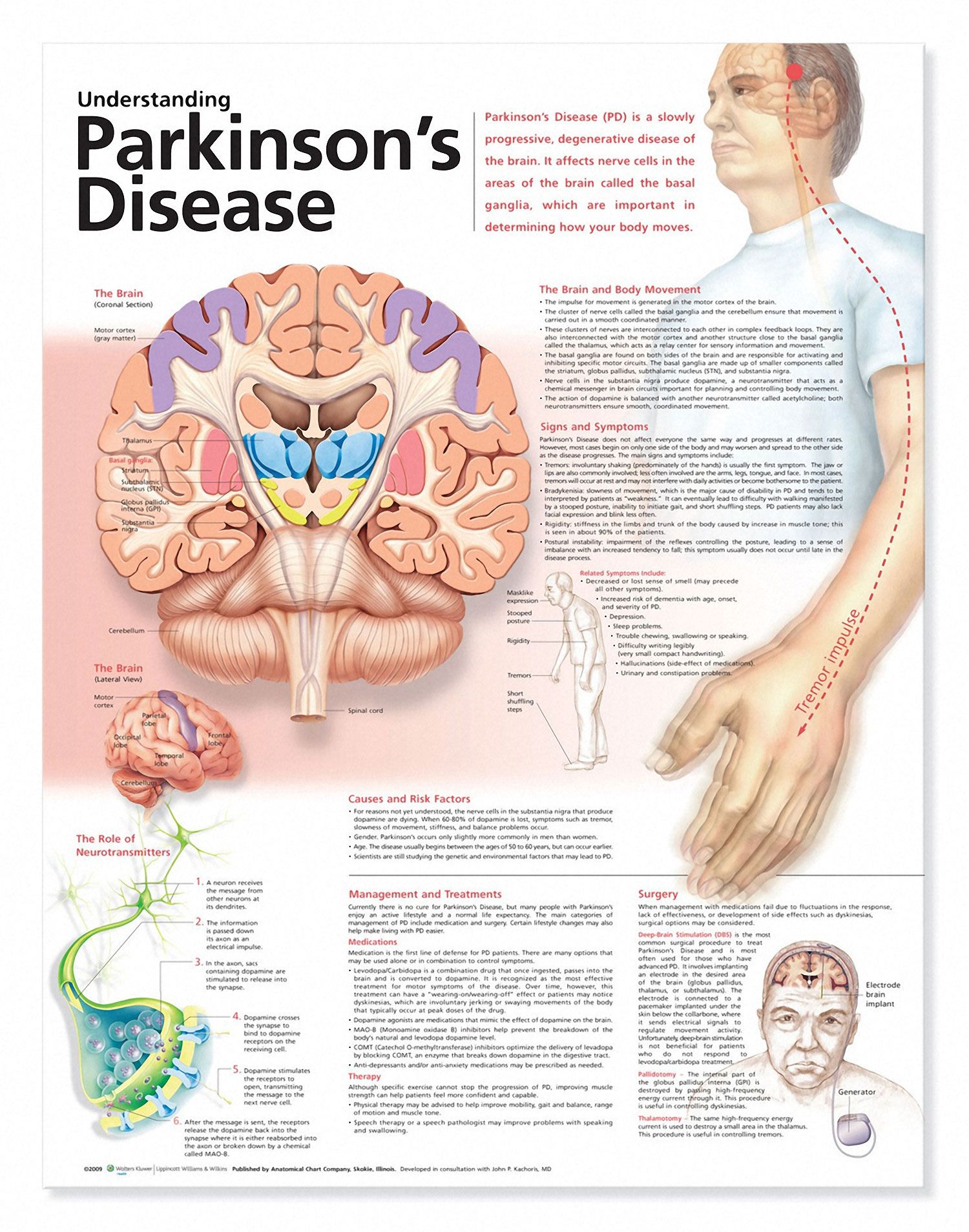
Parkinsons disease has been linked to sleep disorders and sleep disturbances. Parkinsons disease is characterized by the loss of brain cells that control movement. Symptoms of Parkinsons disease can include tremors, stiffness, slowness of movements, as well as balance and coordination problems. Memory problems, depression, and sleep problems can all occur in Parkinsons disease, too.
Sleep problems and sleep disorders may occur as an early sign of Parkinsons disease, even before motor symptoms have started. Common sleep disorders experienced in Parkinsons disease include insomnia, excessive daytime sleepiness, nightmares, sleep attacks, REM sleep behavior disorder , periodic leg movement disorder, restless leg syndrome, sleep apnea, and nocturia, which is frequent nighttime urination.
What Types Of Sleep Problems Do People With Parkinsons Disease Have
Parkinsons disease affects every person differently. It also impacts sleep in different ways. People with Parkinsons may have:
- , finding it hard to fall asleep.
- Fragmented sleep, waking up many times over the night.
- Excessive daytime sleepiness, finding it hard to stay awake during the day.
- Very vivid dreams, which may cause hallucinations or confusion after waking up.
- Emotional dreams or nightmares, which may make you feel emotionally drained after waking up.
Identifying Sleep Apnea In Someone With Parkinson’s
We already know that PD is linked to the parasomnia known as REM sleep behavior disorder .
If a person with PD presents symptoms that resemble , they are urged to have an overnight test in a sleep lab. Not only is this important for treating RBD, but research suggests that, in severe OSA, its symptoms may mimic those in RBD
Nocturnal polysomnography , more commonly referred to as an overnight sleep study, is the gold standard diagnostic assessment used to identify OSA.
If someone with PD is diagnosed with OSA, the go-to treatment is a form of noninvasive ventilation, usually along the line of therapies known as PAP, or positive airway pressure. Current research continues to support the long-term use of PAP therapy to treat OSA in people with PD. Kaminska et al found that PAP therapies improved the overall non-motor symptom burden of PD .
Falling Asleep During The Day
Not getting enough restful sleep at night, some medications, and possibly the disease itself leading to neurodegeneration can lead to daytime sleepiness and even sleep attacks in people with Parkinsons disease.
Excessive daytime sleepiness is one of the most frequent sleep disorder symptoms in Parkinsons disease and can affect a patients quality of life.
Trying to get more restful sleep at night and adjusting medications can help with excessive daytime sleepiness.
A new therapy from is also currently being investigated in a Phase 2 clinical trial to help with excessive daytime sleepiness.
***
Parkinsons News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Rem Sleep Behavior Disorder And Disease Modification In Pd
Impairments of neural circuit switching and imbalance between the inhibitory and excitatory neuronal populations described above are likely responsible for episodic sleep disturbances, in particular found in RBD . This might occur through malfunction of a putative flip-flop switch for REM control, or through a breakdown of the underlying REM sleep circuitry . The majority of idiopathic RBD cases will eventually be diagnosed with PD, dementia with Lewy bodies or multiple system atrophy , with clinicopathological correlations in 172 RBD cases showing that the vast majority has a -synucleinopathy . RBD is common among the -synucleinopathy disorders of PD, DLB and MSA probably because in these diseases cell loss is common within neuronal structures regulating REM sleep atonia, namely the subceruleus nucleus and magnocellularis nucleus in the brainstem, and the amygdala, which is linked to the emotional content of dreams.
RBD is characterized by dream-enacting behaviors and nightmares linked to REM sleep without muscle atonia. RBD can be classified into an idiopathic form and a secondary form, which occurs in patients already diagnosed with PD , DLB , MSA , autoimmune disease and focal brainstem lesions . The use of some medications can also trigger RBD.
Parkinsons Disease And Sleep
Parkinsons disease is a progressive neurodegenerative disorder characterized by the loss of dopamine-producing nerve cells in the brain. Dopamine is a cell-signaling molecule that relays information between nerve cells and between the brain and the muscles. The loss of dopamine leads to symptoms of the motor system such as , , impaired balance, and. It can also cause non-motor symptoms, including speech, cognitive, mood, and sleep problems.
Most sleep problems in Parkinsons patients can be broken down into one of three categories: trouble falling asleep, trouble staying asleep or getting restful sleep, or falling asleep at the wrong times.
What Is Pap Therapy For Osa
PAP therapy involves the use of a nasal interface to mechanically deliver pressurized air to the upper airway while the user sleeps. This delivery system essentially splints the airway open, preventing its collapse and keeping the airway unobstructed. The different kinds of PAP include:
- CPAP = Continuous positive airway pressure
- BiLevel PAP = BiLevel positive airway pressure
- AutoPAP = Autotitrating positive airway pressure
- ASV = Adaptive servoventilation
On The Horizon: Drug Therapies For Treating Osa In Pd
Another option gaining favor is the use of sustained-release levodopa/carbidopa in people who have both PD and OSA.
This pharmacological approach uses this drug combination to improve the rigidity of the tissues of the upper airway, preventing their collapse while also improving their coordination with the muscles in the upper airways.
The recent FDA approval of the oral inhalation medication , prescribed to treat episodes in people with PD using a levodopa/carbidopa regimen, makes potential pharmaceutical relief an attractive option for those with both PD and OSA who dont respond well to or tolerate PAP therapy.
Tips For Better Sleep
- Keep a regular sleep schedule go to bed at the same time and get up at the same time.
- Choose your bedtime based on when you want to get up. Plan to spend seven to eight hours a night in bed.
- Make a bedtime routine for example, snack, bath, tooth-brushing, toileting and follow it every evening.
- Spend time outdoors and exercise every day, in the morning if possible. Avoid exercise after 8:00 p.m.
- If you cant get outdoors, consider light therapy sitting or working near a light therapy box, available at drug stores and department stores.
- If you nap, try to do so at the same time every day, for no more than an hour, and not after 3:00 p.m.
- Sleep in a cool dark place and use the bed only for sleeping and sexual activity.
- Do not read or watch television in bed.
- Use satin sheets and pajamas to make moving in bed easier.
- Minimize drinking liquids for three hours before bedtime to avoid frequent nighttime urination.
- Go to the bathroom immediately before retiring.
- Place a commode next to the bed, to minimize the effort, and light to get up during the night.
- Avoid:
- Alcohol, caffeine and other stimulants such as nicotine
- Heavy late-night meals
- Heavy exercise within six hours of bedtime
- Thoughts or discussions before bedtime about topics that cause anxiety, anger or frustration
- Clock watching
- Screen time television, phones, tablets one or two hours before bed.
Characteristics Of Included Studies
The primary online database search identified 173 studies of potential interest. After reviewing their titles, we excluded 25 studies that were not in English and of the remaining 148 studies the abstracts were studied. Among them, 30 studies were excluded for not meeting inclusion criteria I and 118 full-text studies were finally reviewed. After the second selection round 113 studies were excluded because they did not meet the inclusion and exclusion criteria. For example, one study was excluded concerning its ineligible control referring exclusion criteria V. Consequently, five studies were included in the meta-analysis for evaluating the association between PD and the risk of OSA . Figure 1 shows the detailed procedure of the selection.
Rem Sleep Behavior Disorder
REM stands for rapid eye movement. This is the stage of sleep when dreams take place. People with REM sleep behavior disorder act out their dreams, which can be violent. RBD is one of the early warning signs of Parkinsons. Healthy people with RBD have a higher risk of developing Parkinsons. RBD can be treated with the drug clonazepam .
How Are Sleep Problems Diagnosed In People With Parkinsons Disease
If youre having problems sleeping, sit down with your healthcare provider to discuss the issue in detail. Your provider will ask you questions to better understand your symptoms.
Be prepared to explain when sleep disruptions happen and how they affect your life. Keeping a sleep journal for a few weeks can help you remember the details.
If your provider suspects you may have a sleep disorder, they may recommend you have a sleep study. This overnight test uses electrodes attached to your skin to track how your body functions when youre sleeping.
The Physiological Basis Of Sleep: Sleep Neurobiology And Neurophysiology
In humans, as in most mammals, three vigilance states characterized by differences in electro-encephalogram , electromyogram , and electro-oculogram recordings exist. Different neurochemical mechanisms acting in fine balance are responsible for the transition between the three vigilance states across the 24 hour day.
Waking state typified by high-frequency , low-amplitude desynchronized EEG activity, sustained EMG24-hourty and ocular movements on EOG.
Non-REM sleep ) typified by low-frequency , high-amplitude delta oscillations on the EEG, low EMG muscular activity and no ocular movement. NREM sleep is currently subdivided into three stages according to the American Academy of Sleep Medicine scoring rules, defined mainly on the EEG. The EEG pattern in NREM sleep is described as synchronous, with characteristic wave forms such as sleep spindles, K-complexes and high-voltage slow waves. NREM stages 1 to 3 represent a depth-of-sleep continuum where the arousal threshold is generally lowest in stage 1 and highest in stage 3 sleep. NREM sleep is a stage of minimal energy expenditure and motor activity.
Sleep Apnea And Incident Pd: Intermittent Hypo
Sleep apnea is characterized by repeated periods of hypoxia and reoxygenation during sleep. Sleep apnea may have central, obstructive/peripheral or mixed causes. It has been hypothesized that sleep apnea-induced chronic intermittent hypoxia may increase oxidative stress and inflammation , which may contribute to the pathophysiology of PD . A recent 3-year nationwide retrospective population-based study of 1,944 Taiwanese patients with sleep apnea and 9,720 matched control subjects showed a higher risk of incident PD diagnosis in the apneic patients compared to 0.4% in the controls . The risk of PD remained significant after adjustments for potential confounders, including sex, age, hypertension, lung disease, head injury, rural vs. urban living, geographic region, income, diabetes, hypertension and hyperlipidemia. After age and sex stratification, PD development was independently associated with sleep apnea only in men and in patients aged 60 years and over . In contrast, women did not exhibit a significantly increased risk of PD in the sleep apnea cohort compared to those in the non-apnea cohort during the 3-year follow-up period. Whether sleep is an independent risk factor for PD or merely an early symptom during the prodromal phase of PD remains unclear .
Fig.1
Hypothesized bidirectional changes between the presence of disturbed sleep, risk, and progression of PD. The selected neurodegenerative mechanisms do not follow a pre-specified order and likely overlap.
Parkinsons & Sleep Apnea
One of the many side effects of Parkinsons is interrupted sleep and nighttime disturbances. Due to the tremors and limb stiffness, it is often difficult for those with Parkinsons to fall asleep. These interruptions can also wake you up if you are in the middle of a deep sleep. Discomfort due to limb rigidity and tremor movements do not help the situation either. Some medicines can also interrupt sleep and some patients end up getting their days and nights mixed up with certain prescription medicines.
According to the Parkinsons Disease Foundation, over 40% of Parkinsons Disease patients suffer from sleep apnea. Many people with Parkinsons are loud snorers as well, a symptom of sleep apnea. Sleep apnea and snoring occur when there is an obstruction in the airway. When air has to find another route around an obstruction, it passes down the throat near the sides of the pharynx next to the fatty mouth tissues. These tissues start to vibrate as the air hits them and the vibration creates the loud sound of snoring. Sleep apnea comes into play when your body actually pauses breathing or snoring, and the oxygen flowing into your body and brain become interrupted. When this happens, you literally stop breathing. When your body senses this stop, a signal from the brain is sent and you wake up and start breathing again, usually with a deep gasp for air or extremely loud snore. This type of sleep apnea is called obstructive sleep apnea or OSA.
What Else Can I Do To Sleep Better With Parkinsons Disease
Practicing healthy sleep hygiene habits may also promote more restful .
Do:
- Get outside during the day. Bright light tells your body its time to be awake.
- Keep your body moving during the day. Even if all you feel up to is a short walk or two, all physical activity offers benefits.
- Try at-home remedies, such as massage or a warm bath. Relaxing your mind may help your body fall asleep.
Dont:
- Take long naps during the day.
- Use stimulants, such as , within six hours of bedtime.
- Use your bedroom for activities other than sleeping. Go to another room to read, watch TV or work.
Steps To Sleeping Better
Beyond receiving treatment, there are steps you can take personally to improve your sleep. Particularly when dealing with issues such as difficulty maintaining sleep at night and excessive sleepiness during the day, the concept of sleep hygiene is crucial. Sleep hygiene refers to the behaviors and habits that we can control that affect our bodies day-night cycling and readiness to go to sleep or be alert at a given time of day. Follow these tips for better sleeping habits:
Sleep Disorders In Parkinsons Disease
Parkinsons sleep apnea: Sleep apnea is a sleep-related breathing disorder in which the person stops breathing for brief moments throughout the night. This can cause the individual to awaken abruptly in order to resume breathing. Sleep apnea sufferers often wake up tired, may experience headaches and jaw pain, and may have other health problems, like hypertension and diabetes.
Some studies have shown that up to 20 percent of Parkinsons disease patients suffer from sleep apnea, compared to five percent of the general population. The good news is, sleep apnea can easily be treated with a continuous positive airway pressure device.
Parkinsons insomnia: Insomnia in Parkinsons disease occurs in up to 30 percent of patients. Insomnia can be a sign of anxiety and may also be linked to depression the two other symptoms of Parkinsons disease that may explain its high occurrence. Medication for Parkinsons disease may contribute to insomnia as well, and thus some adjustment of insomnia treatment may be required.
Therapy may help resolve insomnia issues, and practicing good sleep hygiene only using the bed for sleeping, for example may help improve the condition.REM behavioral disorder: The REM sleep phase is when our dreams form and occur. REM behavioral disorder is when a person acts out their dreams. Generally, this is harmless, but it can increase the risk of injury and danger for the sleeper, especially if motor function is impaired.
Related Reading:
What Does Osa Look Like
OSA is a sleep breathing disorder with several identifiable risk factors. Sleeping partners may have witnessed their loved ones choking or gasping for air in their sleep. Also, snoringthough not proof alone of OSAis still suspect if its loud and frequent.
OSA is identified as pauses of breathing during sleep which last at least 10 seconds each and which occur five times or more per hour, on average, during a full nights sleep. By comparison, healthy people without OSA experience less than three episodes of breathing pauses per hour per night.
When these pauses occur, a flurry of other processes within the body take flight: higher blood pressure and pulse, the release of stress hormones, and shifts in insulin-glucose ratios.
When experienced repeatedly over the long-term, but left untreated, OSA is a leading cause for many chronic health issues, including cardiovascular disease, hypertension, type 2 diabetes, major depression, and anxiety disorder. Untreated OSA is also a significant cause of motor vehicle accidents and dangerous mistakes and errors that occur during the day as a result of lingering daytime sleepiness.
Other classic symptoms include frequent nocturnal awakenings, and a variety of sensations upon awakening, such as shortness of breath, sore throat, dry mouth, and headache.
Symptoms That May Be Related To Pd But That Few People Know About
People with PD and care partners may suspect that a particular symptom is related to PD, but they cant find information about it, so they are not sure. Two symptoms that pop up in this category are runny nose and breathing problems, which well focus on today. Of course, if these are new symptoms for you, they could be indicative of a new problem, including infection with COVID-19, so make sure to get yourself checked out by your doctor. However, if all else is ruled out, PD could be to blame. Excessive sweating and specific skin disorders are in this category as well and have been addressed previously.
Assessment Of Sleep Disturbances In Patients With Pd
In general, a comprehensive sleep history is often a very useful first step to narrow down the type of sleep disorders in patients with PD. It should start with the time when the patient goes to bed and gets up and also include planned daytime naps. It should involve the perceived sleep latency, perceived awakenings . The Epworth sleepiness scale or other scales can be used .
Specifically, the evaluation of insomnia should rule out sleep hygiene or circadian disorders. Patients should be questioned specifically about the presence of impulse control disorders and nighttime activities, particularly in case of suspected circadian rhythm disturbances. If a circadian disorder, such as delayed or advanced sleep phase syndrome or non-24-h sleepwake disorder is suspected, assessments with actigraphy or dim light melatonin onset may prove useful .
For patients with prominent daytime sleepiness, polysomnography should be used in every case , but a multiple sleep latency test is also warranted .
Respiration questioning should at least include snoring and witness apneas, positional dependence, breathing pauses, intensity of snoring, nocturnal hypertranspiration or nocturia. In specific cases stridor should also be assessed. If underlying sleep disordered breathing is suspected, cardiorespiratory polygraphy or polysomnography should be performed .
Daytime Tips For Better Sleep
- Wake up at the same time every day, using an alarm if you have to.
- Get out of bed right after you wake up. Too much time spent in bed can lead to more waking at night.
- Eat regular, healthy meals, and eat at the same time every day. Three to four small meals are better than 1-2 large meals.
- Limit daytime napping to a 40-minute NASA nap . Too many or too-long naps can make sleep at night more difficult.
- Do not drink coffee, tea, sodas, or cocoa after noon. They contain caffeine and can interfere with normal sleep.
- Do not drink alcohol after dinner. It may help you fall asleep faster, but makes sleep shallower later in the night. Alcohol can also make snoring and sleep apnea worse.
- Use caution when taking headache and cold medicines. Some contain stimulants that can affect sleep.
- Stop smoking. Cigarette smoking stimulates the body and makes sleep difficult.
- Increase or start doing daily exercise. Regular exercise helps to deepen sleep. Avoid heavy exercise 2 hours before bedtime.
How Does Parkinsons Disease Cause Sleep Problems
Researchers have yet to uncover every nuance of the Parkinsons and sleep connection. So far, medical experts believe several causes may contribute:
- Chemical changes in the brain: Ongoing research shows that Parkinsons disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinsons to get less sleep.
- Medication: Some drugs that treat Parkinsons disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinsons commonly deal with mood disorders, such as or . Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinsons symptoms: Pain, waking up at night to pee or other Parkinsons symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Good Night: Sleep And Parkinsons Disease
Lack of good sleep can worsen Parkinsons symptoms. In this 45-minute lecture, Dr. Rafael Zuzuárregui addresses causes of sleep loss and the latest treatments for: insomnia, restless leg syndrome, REM sleep behavior disorder, nocturnal urination, hallucinations, wearing off of medication, dystonia and sleep apnea.
