Origins Of Breathing Disorders
The book by Leon Chaitow and co-authors cited above explains how breathing disorders are intrinsically linked to chronic stress and anxiety. The shallow, fast chest breathing through the mouth is a hallmark of the body preparing itself for the exertion of flight or fight due to a stress response. While this adaptive in acute stress situations, when stress is chronic and the body is spending a lot of time in fight or flight, the associated pattern of breathing becomes habitual, and eventually the system gets stuck in the new equilibrium of the CO2 intolerant state. However, the vicious circle work both ways, because overbreathing itself puts the body into a stress response state and feeds anxiety. A very good tutorial about the two way links between anxiety and breathing patterns is given by Robert Litman in the video below.
It is not surprising therefore that people with PD can present with disordered breathing associated with chronic stress and anxiety, since there are very significant overlaps between the other symptoms of chronic stress and those of Parkinsons Diseases, and ingrained fight or flight behaviours are common to the pre-diagnosis background histories of people with PD. Conversely, it is important to note that techniques which have been developed to treat breathing disorders should also help to decrease the symptoms of PD, including reduction of anxiety and increasing resilience to stress.
Recommended Reading: What Does Parkinsons Disease Do
Symptoms Of Parkinsons Tremor
Like most symptoms of Parkinsons disease, it is usually asymmetric. It starts generally on one side, which remains the more affected side forever. Having a tremor on one side does not mean that the other side will begin to shake as well. Many people have tremor on only one side throughout their illness.
Immunologically Mediated Inflammatory Brain Diseases
Antibodies reacting with N-methyl-d-aspartate receptor are associated with a very distinct disease course.60-62 Children develop behavioral changes, memory loss, psychosis, orofacial dyskinesia, movement disorders, seizures, alteration of speech leading to mutism, and autonomic dysfunction and hypoventilation if not treated.
McKeon and colleagues reported a syndrome characterized clinically by optic neuritis , transverse myelitis and/or episodic encephalopathic signs, ataxia, seizures, and vomiting .63 All had antibodies to water channel aquaporin 4 . MRI studies showed widespread lesions. The presence of anti-NMO antibodies should lead to the consideration of Sjögren syndrome in the differential diagnosis.64 Treatment with rituximab was reported to reduce the frequency of attacks and improve long-term outcome.65
Rasmussen’s encephalitis is a T-cellâmediated66 parenchymal inflammatory brain disease usually appearing in childhood as intractable focal seizures.67,68 Typically, only one brain hemisphere is involved. The etiology of Rasmussen’s encephalitis is unknown. Surgical resection of the affected tissue may be required to halt ongoing seizures.
Recommended Reading: Huntington’s And Parkinson’s Symptoms
Causes Of Tardive Dyskinesia
Tardive dyskinesia is a very serious side effect of antipsychotic medications, mainly due to the use of typical antipsychotics. Although less likely, the newer and atypical antipsychotics may also cause the disorder.
Medications that can cause TD include:
It may also occur as a side effect with some antiepileptic drugs, antidepressants, antiemetics, and anticholinergics.
One theory about the cause of tardive dyskinesia is that over time, blocking dopamine receptors on nerve cells can cause the brain to compensate by creating more dopamine receptors and making them more sensitive, which can lead to tardive dyskinesia.
The majority of cases of TD are due to the use of antipsychotics , however, other categories of medications, such as certain anti-nausea drugs and other psychiatric medication, have been connected with the development of TD.
What Does Tardive Dyskinesia Look Like
TD looks like different, uncontrollable movements and patterns of the limbs and face. Sometimes referred to as stereotypy, the activity can be patterned, repetitive, and rhythmic movements that can involve one or more body parts. More than 3/4 of those with TD experience oral-facial-lingual stereotypic movements .1 The Baylor College of Medicine Movement Disorders Clinic conducted a videotape review of 100 people with tardive dyskinesia. The evaluation showed that the majority experienced irregular and chaotic movements in the OFL region, including lip smacking, chewing and other tongue and mouth movements. Other areas of the body can also show signs of TD like nodding and rocking, repeated body movements like crossing and uncrossing arms and legs, and random vocalizations.
Those who experience these involuntary movements may not even realize it. Like other conditions, these stereotypies can get worse under stress. They can manifest as muscle contractions or spasms, inability to be still, facial tics, or other jerking and abnormal movements.
Don’t Miss: What Can Mimic Parkinson’s Disease
How Is Tardive Dyskinesia Diagnosed
A doctor may make a diagnosis of tardive dyskinesia if a person is taking a medication that can cause it, has signs and symptoms of the problem, or has undergone testing to rule out other neurological or movement disorders that can cause similar symptoms. Other conditions that can cause involuntary or uncoordinated movements include Huntingtons disease, cerebral palsy, Tourette syndrome, and dystonia per the National Organization for Rare Disorders.
Doctors may also use a tool called the Abnormal Involuntary Movement Scale to detect tardive dyskinesia in people who are taking neuroleptic drugs and to track the severity of their symptoms over time. During an AIMS test, your doctor will gauge the involuntary movement throughout your body on a five-point scale, assessing the severity of movements. The AIMS may be administered before a neuroleptic drug is prescribed so the doctor has a baseline against which to compare future results, according to an article published in April 2022 in StatPearls.
Wake Forest Baptist Multidisciplinary Approach
The treatment of movement disorders at Wake Forest Baptist is a collaborative effort between neurologists and neurosurgeons.
Quality of life is further enhanced by the participation of physical, occupational and speech therapists, and otolaryngologists who have special expertise in speech and swallowing difficulties.
Don’t Miss: Tango For Parkinson’s Disease
Who Is At Risk For Tardive Dyskinesia
Tardive dyskinesia affects all ages, genders, races and ethnicities. People who are older, Black or female are more likely to develop this problem.
Certain factors increase your risk, including:
- Smacking lips or making sucking motions with the mouth.
- Sticking out your tongue or probing the inside of your cheeks with your tongue.
Tardive dyskinesia can affect other parts of your body. You may:
- Make repetitive finger movements like playing the piano.
- Thrust or rock your pelvis.
- Walk with a duck-like gait.
How Is Tardive Dyskinesia Managed Or Treated
Your healthcare provider may gradually lower your medication dose. Eventually, you may stop the drug. If you need ongoing treatment, your healthcare provider may prescribe a different medicine.
For some people, these changes end tardive dyskinesia symptoms. You should only make medication changes under your healthcare providers care.
Some people still have symptoms despite medication changes. Over time, the symptoms may improve and go away. Rarely, symptoms become worse.
If symptoms persist, these treatments may help:
- Tetrabenazine, the only approved drug for the treatment of movement disorder symptoms.
- Botulinum toxin injections , which blocks facial nerve signals for a few months.
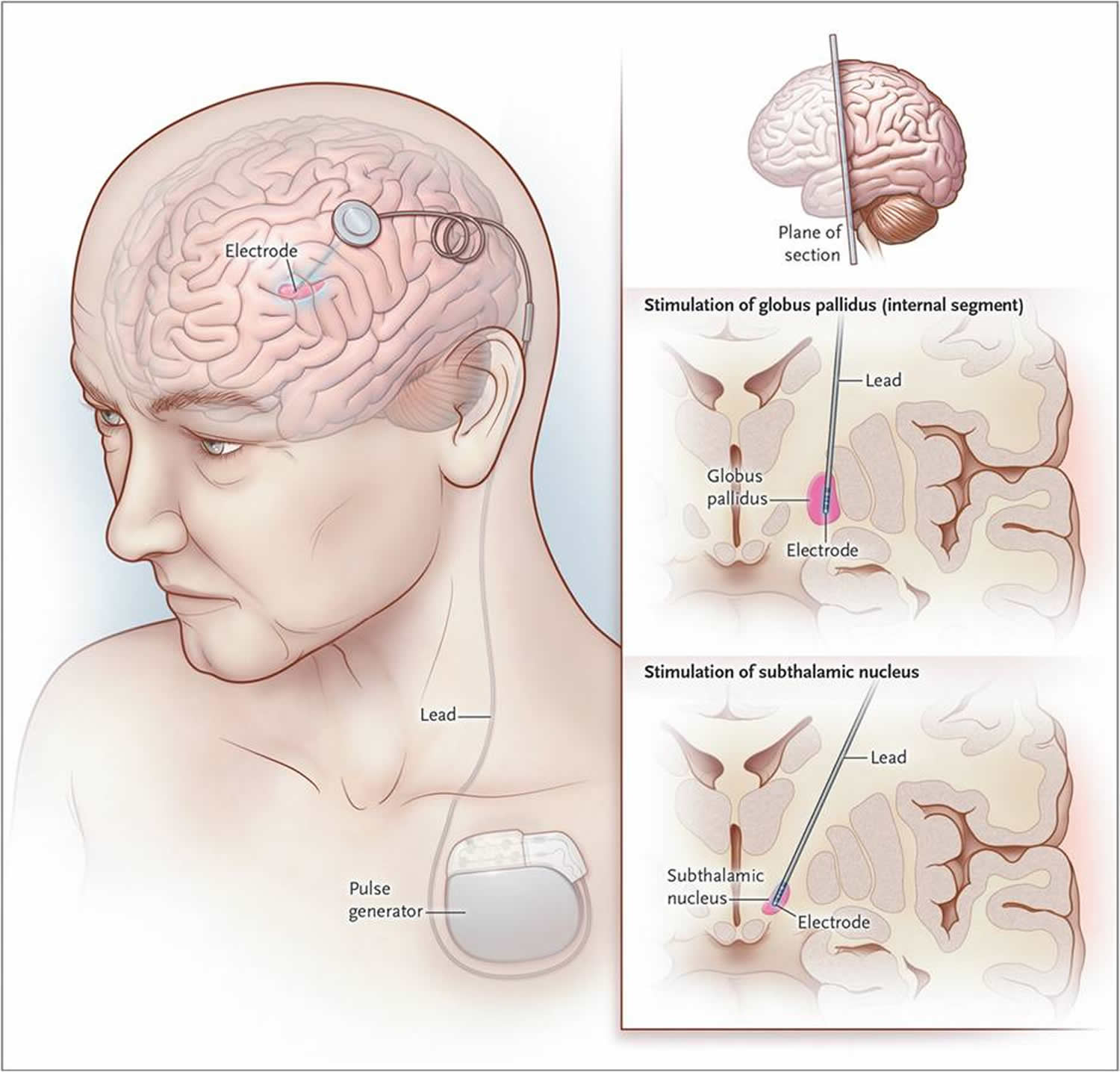
- Deep brain stimulation, an implantable device that blocks irregular nerve signals to areas of the brain that control movements.
Also Check: Sam Waterston Tremor
Also Check: What Are The End Stages Of Parkinson’s Disease
Common Characteristics Of Myoclonus Or Muscle Jerking
Myoclonus is muscle jerking, in which the muscles suddenly tighten and release. Everyone has experienced this with hiccups or “sleep start,” the sudden jerk that may happen just as a person falls asleep. These types of myoclonus are normal, but the condition can become severe and greatly disrupt normal life.
- Action myoclonus: This is triggered by trying to move.
- Stimulus-sensitive myoclonus: This is triggered by noise, light, or being startled.
- Essential myoclonus: This occurs for no known reason and usually stabilizes over time.
- Epileptic myoclonus: This is a form of epilepsy.
- Secondary myoclonus: This is due to neurodegenerative disease.
Ataxia / Dysmetria / Asynergia
Ataxia is an unsteady and swaying walk, often with feet planted widely apart. People have difficulty walking a straight line with their heel touching the toe of the shoe in front . Ataxia can occur in a number of neurologic conditions.
Dysmetria is misjudging the distance to a target. A person with dysmetria will have problems reaching out and accurately touching a targeted object.
Asynergia is a breakdown of movement, so that movements of the arms and legs become irregular and clumsy.
For more information, visit the National Ataxia Foundation website at www.ataxia.org.
Don’t Miss: What To Buy Someone With Parkinson’s
Surgical Management Of Hyperkinesis
Some degree of synkinesis, hypokinesis, and hyperkinesis accompanies reinnervation of the face, whether nerve regeneration occurs with nerve grafting or nerve substitution techniques or with spontaneous recovery from a denervating injury. Synkinesis can be improved by sensorimotor re-education, in which the patient practices in front of a mirror, with the help of electromyography, to separate facial muscle activities.19,20 Hyperkinesis may be treated medically or surgically.21 Botulinum toxin injected into muscles involved in hyperkinesis causes temporary paralysis and temporary relief from hyperkinesis. When the effects of the botulinum toxin dissipate , injection can be repeated. Surgically selective neurolysis or regional myectomy can provide longer lasting treatment for hyperkinesis. Selective neurolysis involves weakening or paralyzing innervation to the hyperkinetic muscle. The results of neurolysis are difficult to predict, however, and hyperkinesis may return, even after excision of a segment of nerve. For these reasons, regional myectomy is the currently preferred surgical technique for management of hyperkinesis in patients who fail or who are unwilling to use botulinum toxin.
Adam W. Grasso, Sorin J. Brener, in, 2010
Treatment And Medication Options For Tardive Dyskinesia

There is no standard treatment for tardive dyskinesia. Most likely, your doctor will adjust the medication thought to be causing the symptoms. In many cases, neuroleptic medications will be lowered to the lowest possible dose or discontinued if possible. But theres limited evidence that lowering the dose, administering the drug intermittently, or stopping the drug altogether will reduce tardive dyskinesia symptoms.
Abruptly stopping a neuroleptic medication is not recommended because doing so can worsen tardive dyskinesia or even cause it in a person who is not already affected by it.
Also Check: Is Parkinson’s Considered A Disability
Equipment And Walking Aids
You might find that equipment can help you to walk, such as a walking stick or a rollator .
Before you start using a walking aid, its very important to get advice from a physiotherapist. Some walking aids arent recommended for people with Parkinsons as they can affect your walking pattern and make you more likely to fall. But, the correct walking aid can increase your confidence and help you to lift your feet better.
What Are The Complications Of Tardive Dyskinesia
Tardive dyskinesia can make you self-conscious. You may withdraw from people. Isolation may bring on or worsen depression or anxiety, though. The condition can affect your ability to work. It may strain relationships with loved ones, as well.
A small number of people develop severe symptoms that can affect quality of life. Rarely, these problems are life-threatening. They include:
- Breathing issues.
- Irreversible facial changes, such as drooping eyelids or mouth.
- Speech difficulties.
Also Check: How Do I Stop Drooling In Parkinson’s
If Levodopa Causes Dyskinesia Then Why Should I Take It
At present, treatment with levodopa is the most effective way to relieve tremor, stiffness, and slow movement associated with Parkinsons. In the early stage of Parkinsons, levodopa may not be necessary and there are other medications available to treat this stage of the disease. However, as the disease progresses and symptoms begin to interfere with daily living, your doctor will prescribe levodopa.
- It typically doesnt develop immediately Its important to note that there is usually a time lag of roughly 4 to 10 years from the start of treatment with levodopa to when dyskinesia emerges, and its severity will vary among different individuals.
- Younger people are at a greater risk People who get Parkinsons in their later years may not show signs of dyskinesia or may have only mild symptoms within their lifetime. Being diagnosed with Parkinsons at a younger age is associated with a greater chance of developing dyskinesia.
- As with every aspect of Parkinsons, there is variability in dyskinesias Some do not develop dyskinesias at all. For those who do get them, not all experience them the same. Dyskinesia in its milder form may not be bothersome, and the mobility afforded by taking levodopa may be preferable to the immobility associated with not taking levodopa. People with Parkinsons must weigh the benefits from using levodopa versus the impact of dyskinesia on their quality of life.
Vocalizations As Part Of Stereotypies
The precise definition of stereotypies and their exact phenomenological distinction from other repetitive motor behaviors, for example, tics, is difficult. The term denotes a repetitive, often continuous, non-goal-directed movement pattern that is typically distractible. As with echolalic behaviors, stereotypies are also part of physiological development that often abate within the first years of life. Although the persistence of stereotypic vocalizations may still be part of normal development, in many cases it signifies pathology, and indeed stereotypic utterances are part of the diagnostic criteria of ASD . One large case series of 83 patients with Rett syndrome described phonic stereotypies with repetitive sounds, words, or phrases in only 6% of patients. We recently observed loud stereotypic vocalizations in a patient with 15q13.3 microdeletion syndrome and late-treated cases with phenylketonuria. Further, stereotypic vocalizations have been documented in patients with schizophrenia.
Also Check: Sam Waterston Parkinsons
Also Check: What Happens In Stage 5 Of Parkinson’s Disease
Causes And Risk Factors
Essential tremor occurs as the result of abnormal communication between certain areas of the brain. A genetic cause for essential tremor has been identified in 5070% of cases and, as a result, it has a strong tendency to run in families . While essential tremor can affect people of all ages, the average age of onset is 3545 years. The condition may get worse over time. It occurs equally in men and women, and can affect all ethnic groups.
If Your Tremor Persists When You Move Essential Tremor May Be To Blame
If the tremor persists despite intentional movement, the most likely culprit is Essential Tremor . Like PD, this condition can cause rhythmic shaking in any part of the body, and is sometimes misdiagnosed as Parkinson’s.ae0fcc31ae342fd3a1346ebb1f342fcb
“It may be difficult to figure out if a jaw tremor is from Essential Tremor or Parkinson’s,” explains the APDA. “Unfortunately, some people may have both disorders,” the organization adds, noting that some researchers have found “an association between the two conditions, so that more people with Parkinson’s disease have Essential Tremor than would be expected by chance alone.” However, more research is needed to fully understand the connection between the two conditions.
For more health news sent directly to your inbox, .
You May Like: Nyu Parkinson’s And Movement Disorders Center
Types Of Secondary Movement Symptoms
How To Approach The Symptom
If youve experienced involuntary mouth twitches and ignored them or seen someone do the same, its best to reach for medical help immediately. You might not dwell much on it now, but PD disease symptoms keep getting worse.
What is now involuntary twitching might turn into the unintentional opening and shutting of the mouth.
Your first visit should be to a neurologist specializing in movement. They will examine you for other symptoms. They will also administer medications such as Klonopin or Valium to deal with the signs and give you some relief.
One of the most effective solutions to Dystonia, like many serious illnesses, is early detection and treatment. After that, it is pretty standard for patients to live long and healthy lives with the proper treatment.
Recommended Reading: Are Hallucinations Part Of Parkinson’s
Stooping Or Hunched Posture
People who have Parkinsons disease may notice changes in their posture due to other symptoms of the disease, such as muscle rigidity.
People naturally stand so that their weight is evenly distributed over their feet. However, people who have Parkinsons disease may start bending forward, making them appear hunched or stooped over.
Neurological Or Neurodegenerative Diseases
These are progressive illnesses and slowly get worse over time. They are caused by disorders of the nerves in the brain and spinal cord, due to:
- Heredity: Many neurodegenerative illnesses run in families and are inherited, though not all family members need to be affected.
- Autoimmune conditions: The bodys own immune system turns against some of its other systems in this case, the nervous system. The reasons for this are not clear.
Recommended Reading: On Off Phenomenon
Read Also: What Age Does Parkinson’s Disease Usually Start
When Do Tardive Dyskinesia Symptoms Appear
Most people take medications for years before developing tardive dyskinesia. Rarely, symptoms develop within three months of starting a medicine.
Youre unlikely to develop tardive dyskinesia if you take a medicine for a few weeks. Although rare, some people develop tardive dyskinesia after they stop a medicine.
