Parkinson’s Disease Symptoms: Life Expectancy
Even though Parkinson’s disease is a serious, progressive condition, it is not considered a fatal illness. People who have Parkinson’s disease usually have the same average life expectancy as people without the disease.
But when the disease is in its advanced stages, Parkinson’s symptoms can lead to life-threatening complications, including:
- Falls that lead to fractured bones
- Pneumonia
- Choking
Thinking about the progression of Parkinson’s disease can be frightening. But proper treatments can help you live a full, productive life for years to come. And researchers hope to one day find ways to halt the progression of Parkinson’s and restore lost functioning.
How Can I Support Someone With Parkinson’s At The Advanced Or Palliative Stage
In the advanced stages of Parkinsons, your patients care needs may be more complex and require careful planning along with the patient, their family and other health and social care professionals involved.
Palliative care should be holistic, considering the whole person to support the personal, social, psychological and spiritual needs of your patient and their family. It should give your patient some control and choice over areas such as treatment options and where they will be cared for, as well as providing advice and support to all the people involved in their care.
Palliative care in Parkinsons may be supported by a number of professionals, including a Parkinsons nurse specialist, local hospice or specialist palliative care team, physiotherapist, occupational therapist, speech and language therapist or dietitian. Many people with Parkinson’s also find complementary therapies beneficial.
It is important that you find out whether the person has a care plan in place regarding their preferences for how the issues surrounding advanced Parkinsons should be managed. This could include legal documentation such as a Lasting Power of Attorney and an advance care plan. Advance care plans include information on what the persons wishes and preferences are for their care in the future. They may include decisions on any treatments the person doesnt want to have in the future this is called an Advance Directive, Advance Decision to Refuse Treatment or Living Will.
What Does End Stage Parkinson’s Disease Look Like
In the final stage of Parkinson’s disease, patients are unable to perform basic movements without assistance and require one-on-one care, according to Healthline. Quality of life rapidly declines as sufferers become bedridden or wheelchair bound and experience worsening memory and speaking problems. Infections become more common and incontinence worsens. Sadly, medications and treatments provide little or no relief to patients in this stage of the disease.
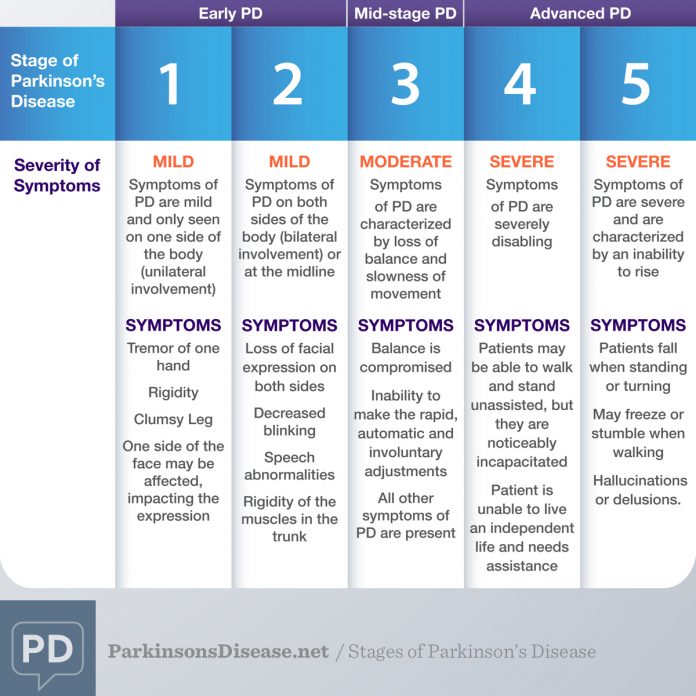
The progression of Parkinson’s disease is divided into five stages, with the disease increasing in severity as the number of the stage increases, explains Healthline. The speed of progression of the disease and specific symptoms vary from patient to patient.
In stage one, Parkinson’s patients experience mild symptoms that affect only one side of the body, such as tremors or shaky limbs, notes Healthline. In stage two, motor symptoms begin to affect both sides of the body, and patients may start to experience difficulty walking and maintaining balance. Stage three is considered moderate Parkinson’s disease, and patients in this stage typically have difficulty performing basic physical movements, but can still function on their own without assistance. In stage four Parkinson’s disease, patients begin to experience severe, disabling symptoms and often cannot live on their own without a caregiver. Stage five is the end stage of Parkinson’s disease.
Recommended Reading: Do Dogs Get Parkinson’s
Managing Symptoms In The End Stage Of Parkinsons
Because of the degenerative nature of the disease, patients in the end stage of Parkinsons are at severe risk of:
- Rashes
- Digestive Problems
To avoid serious complications, patients require 24-hour assistance. This includes:
- Shifting Them Every Two Hours. To prevent their weight from opening wounds on the skin.
- Toileting. Besides walking patients to the bathroom, caregivers need to help them undress and clean up afterwards.
- Changing Diapers. If the patient is confined to bed, their diapers need to be checked and changed every two hours to prevent excoriation .
- Bathing & Grooming. If the patient cannot get to the shower, the caregivers will need to give them a sponge bath. Patients will also need help trimming their nails, combing their hair, and brushing their teeth.
- Eating. Caregivers may have to push patients to eat, if they are able. Because of difficulties chewing and swallowing, soft foods may be all they can eat at this stage. Oatmeal, scrambled eggs, yogurt, applesauce, mashed potatoes, and smoothies are good choices. If you serve solid food, cut it into small pieces to prevent choking.
- Drinking. Patients need to drink 6-10 glasses of water a day to stay hydrated.
- Organizing Medication. Patients are usually prescribed several medications to reduce shakes and control movement. Medications need to be carefully organized and all caregivers need to be briefed on their instructions.
When is it Time for Hospice Care?
Data Abstraction And Risk Assessment
Any two of three investigators independently screened titles, abstracts and retrieved full papers with eligibility criteria. Differences were resolved by review of the third investigator.
We assessed risk of bias by reviewing study design characteristics, including appropriate temporal relationships between exposures and outcomes, matching populations through individual variables or propensity scores and other adjustment methods. However, given we did not develop a meta-analysis from the findings, we did not exclude reporting any studies that met our inclusion criteria.
Don’t Miss: Can Parkinson’s Run In The Family
Stage Three Of Parkinsons Disease
Stage three is considered mid-stage and is characterized by loss of balance and slowness of movement.
Balance is compromised by the inability to make the rapid, automatic and involuntary adjustments necessary to prevent falling, and falls are common at this stage. All other symptoms of PD are also present at this stage, and generally diagnosis is not in doubt at stage three.
Often a physician will diagnose impairments in reflexes at this stage by standing behind the patient and gently pulling the shoulders to determine if the patient has trouble maintaining balance and falls backward . An important clarifying factor of stage three is that the patient is still fully independent in their daily living activities, such as dressing, hygiene, and eating.
Theory Of Pd Progression: Braaks Hypothesis
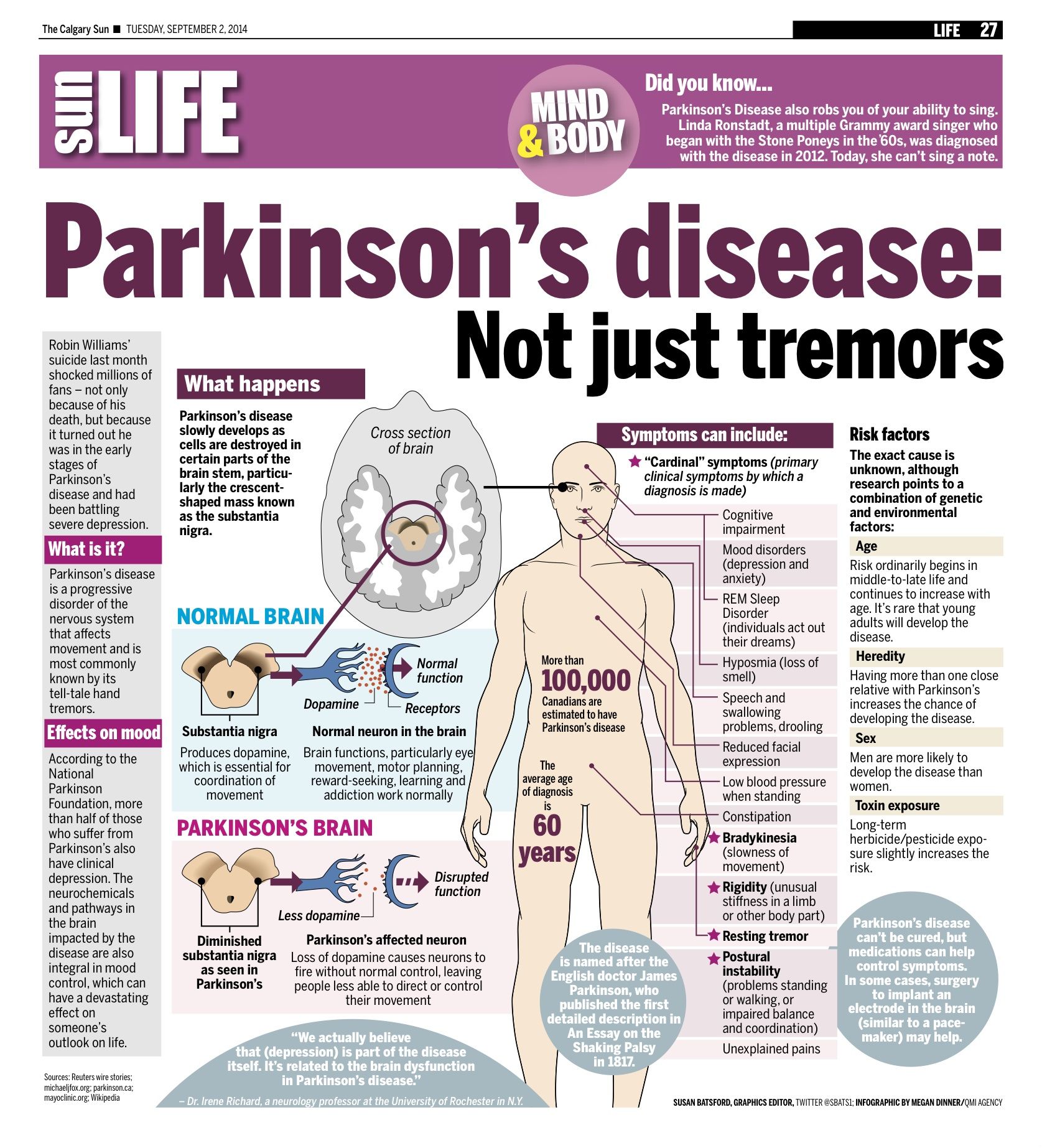
The current theory is that the earliest signs of Parkinson’s are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinson’s only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
Read Also: Parkinson’s Disease Awareness Ribbon Color
Two Areas In Which Parkinsons Disease May Bring About Death
I. Falls
PD patients are at an increased risk of falling and bad falls can lead to death. This usually occurs as a complication of a fall that requires hospitalization, particularly if it involves surgery. While most people do not fracture their hips when they fall, some do, and hip surgery, while routine, is still major surgery. It carries the risk of infection, delirium related to pain medications and anesthesia, heart failure, pneumonia, blood clots in the legs that then go to the lungs, and general weakness from immobility. Hip fractures are probably the main cause for death for those who fall, but people can fracture other bones and require surgery. They may fracture their ribs, which leads to reduced coughing, because of the pain, and an increased risk of lung infections . It is surprisingly uncommon for Parkinsons Disease patients to die from brain injuries related to falls, but it still may occur.
II. Pneumonia
PD patients also may develop pneumonias completely unrelated to difficulties with swallowing, just like their non-PD friends and relatives.
How Is Parkinson’s Managed
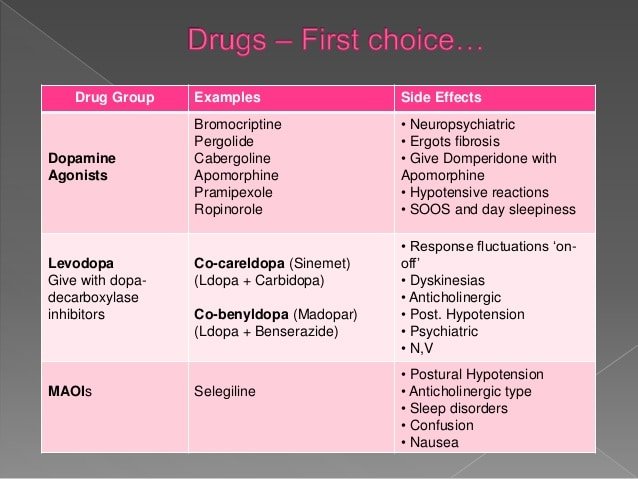
There is currently no cure for Parkinsons but there are medications and therapies that can help to manage Parkinsons symptoms.
Medicines that increase the level of dopamine in the brain are the main treatment used to manage the symptoms of Parkinson’s. Medicines are tailored to each individuals needs.
Symptoms will get worse when someones Parkinsons medicines are wearing off and improve again after Parkinsons medicines are taken. If people with Parkinsons dont get their medication at the right time, it leads to their motor symptoms becoming uncontrolled. It can take some time to get their symptoms under control again. If you work in a hospital or care home, it is important to be aware that medicine timings will vary from person to person and may be different to ward medicine rounds.
As well as medicines, surgical options are available for some people with Parkinson’s, depending on their symptoms.
Treatments can help to manage the symptoms, but may become less effective in the later stages of the condition.
Parkinsons UK has more information on how Parkinsons affects people and how it can be managed.
Read Also: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed
In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half of the patients were described as unable to make any decisions in the last month of life. 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
What Are The Symptoms Of Parkinson’s
The main motor symptoms of Parkinsons are:
- tremor
- slowness of movement
- problems with balance.
However, the condition doesnt only affect movement. People living with the condition can experience a range of non-motor symptoms that can often have a greater impact on their lives than movement difficulties.
Non-motor symptoms include:
- urinary urgency, frequency
- pain.
These non-motor symptoms are present at all stages of the condition but they can become more severe in the later stages of Parkinsons and have a major impact on quality of life.
Parkinsons gets worse over time and it can be difficult to predict how quickly the condition will progress. For most people, it can take years for the condition to progress to a point where it can cause major problems. For others, Parkinsons may progress more quickly.
Read Also: Is Parkinson’s Disease Fatal
Motor Symptoms And Global Disability
Motor symptoms, as measured using the Unified Parkinsons Disease Rating Scale , Hoehn and Yahr Scale and the Progressive Supranuclear Palsy Rating Scale , were significant predictors of mortality in patients with PDRD. Beyer et al found higher mean UPDRS scores, 65 versus 42 , suggesting that greater motor impairment predicted death. Studies with median follow-up times ranging from 4 to 8 years estimated the association of 10-unit increases in baseline motor UPDRS Score on mortality and found statistically significant increased HRs for mortality of 1.17 up to 1.4 for each 10-unit increase in UPDRS Score. Baseline H& Y staging was significantly higher among those who died ) compared with those who survived ). Posada et al went further by splitting H& Y into early and later progression stages at baseline as a predictor for mortality and found that HRs increased by stage, from 1.5 for H& Y stages 1 and 2 to 2.3 for H& Y stages 35, both compared with patients with no PD and after controlling for comorbidities and demographic characteristics. Oosterveld et al stratified UPDRS total motor scores by greater than or equal to 30 compared with less than 30 and found an HR of 1.63 . Chiu et al compared the association of PSPRS scores on mortality and found increased HRs of 1.96 for 3548 on the PSPRS, 2.99 for 4862 and 8.55 for greater than 62 when compared with scores of 034.
What To Expect In The Late Stages Of Parkinsons Disease
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinsons Disease In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinsons Disease Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
Read Also: Can Alcoholism Mimic Parkinson\’s
Parkinsons Disease Symptoms Of Dementia
Up to one-third of people living with Parkinson’s disease experience dementia, according to the Parkinson’s Disease Foundation. Problems with dementia may include trouble with memory, attention span, and what is called executive function the process of making decisions, organizing, managing time, and setting priorities.
RELATED: 12 Famous People With Parkinson’s Disease
What Are The Important Points Regarding Apomorphine At The End Of Life
Apomorphine is a dopamine agonist, which is given as a subcutaneous infusion either continuously or intermittently and also as single subcutaneous injections. An overview of studies into apomorphine use shows improvement in motor off periods and in dyskinesias.39
Apomorphine has side-effects similar to other dopaminergic medication but also notably nausea and vomiting. Ondansetron is not recommended for nausea in patients using apomorphine due to adverse effects.21
Subcutaneous apomorphine has been used at the end of life in a patient with advanced PD although with the recommendation that this is by a healthcare professional experienced in its use.40
Also Check: How Is Parkinson’s Disease Inherited
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
Causes Of Parkinson’s Disease
Parkinson’s disease is caused by a loss of nerve cells in part of the brain called the substantia nigra. This leads to a reduction in a chemical called dopamine in the brain.
Dopamine plays a vital role in regulating the movement of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinson’s disease.
Exactly what causes the loss of nerve cells is unclear. Most experts think that a combination of genetic and environmental factors is responsible.
Also Check: Essential Oils For Parkinson Disease
Caring For A Person With Advanced Parkinsons Disease
In this 47-minute webinar Anne Wallis, Associate Director of Education at the Parkinsons Foundation, talks with doctor of physical therapy, Sarah King, about when to look for outside help, how to lasso the power of your friends and family , and how to build an allied healthcare team that decreases your stress and improves your loved ones care.
How Can Healthcare Professionals Support People With Parkinsons When They Are Making Decisions About End Of Life
Access to resources is a specific issue for different countries and communities, as palliative care and end of life management varies through European countries.
Still, there is an ongoing need for awareness about palliative care among healthcare professionals especially in the ability to explain the conditions progression, accompanying problems, interventions for relief and end of life activities. Skills for identifying spiritual distress and arranging an end of life should be included in the expertise of Parkinsons disease practitioners, to help people with the condition with any legal and financial issues, existential challenges, care plans, wishes for treatment, wills and anything else that needs to be considered.
Recommended Reading: Late Stage Parkinson