Recognition Of Parkinson’s Disease
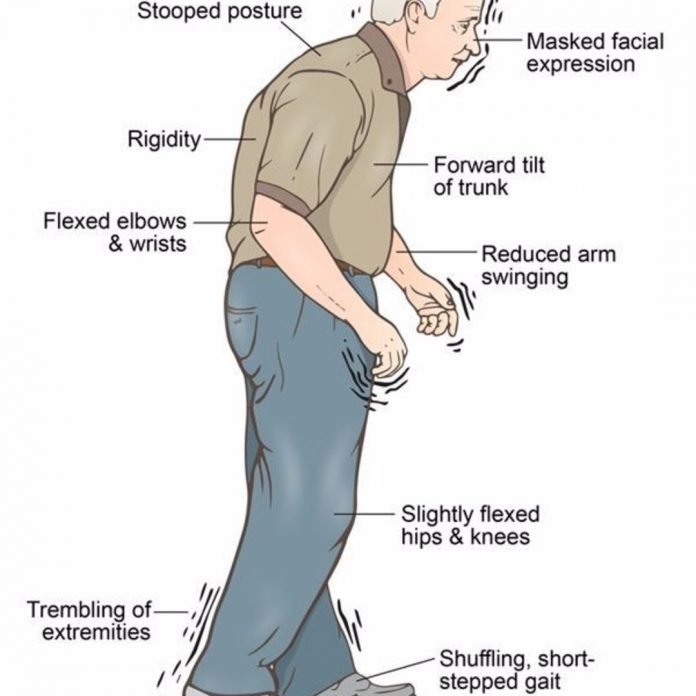
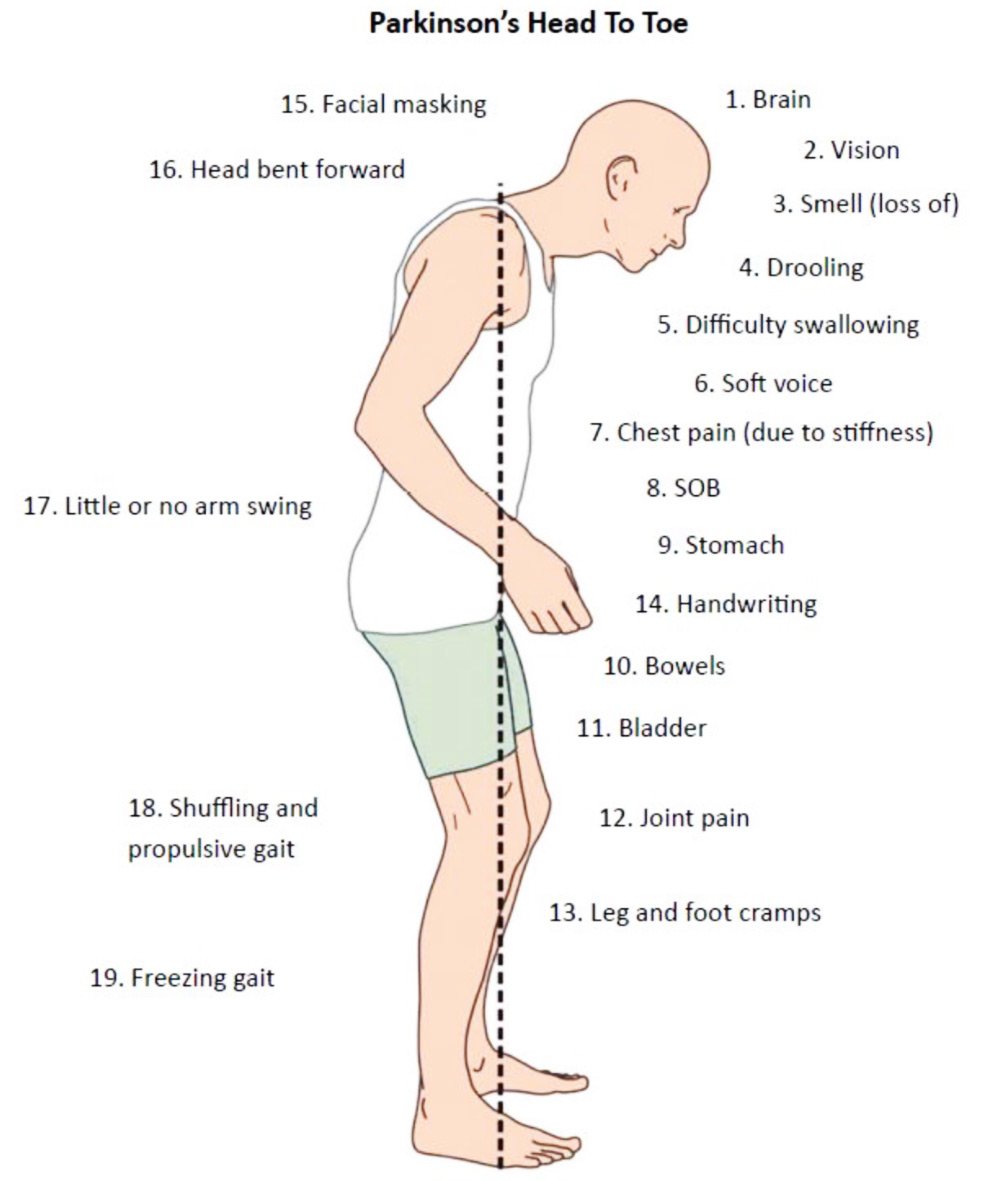
Parkinson’s disease is appreciated on clinical grounds no laboratory tests are used routinely to establish the diagnosis. The cardinal clinical features are bradykinesia, rigidity, and tremor. Shuffling gait and flexed posture are also characteristic and are sometimes listed together as a fourth principal sign. Bradykinesiaslowness of movementis the most disabling aspect of Parkinson’s disease. Patients describe it as stiffness, weakness, or a pervasive slowness that affects every aspect of movement. Dressing, eating, and other activities of daily living take extra time. There is also paucity of movement and difficulty initiating movement. Patients experience some loss of dexterity for buttoning, handwriting, and fine finger movement. Many describe difficulty getting up from a chair or getting out of the car, movements that require truncal mobility and complex postural adjustments. This same difficulty is likely to be reflected in the patient’s tennis serve, golf swing, or bowling score. It is difficult for patients with Parkinson’s disease to perform two complex motor acts at the same time, so many such activities acquire a slow, deliberate character. Arrests of ongoing movement sometimes occur .
There is no lab test or biological marker to use as an adjunct in diagnosis. Magnetic resonance imaging often is obtained in patients with atypical features to rule out a systemic degeneration or ischemic change in the basal ganglia as a cause of symptomatic Parkinsonism.
Pair Your Medication Dose With Exercise
Try to schedule your workouts during times when your mobility is best. Monitor how long it takes for your medication to kick in to determine when to exercise.
With Parkinsons disease, the phrase use it or lose it takes on greater meaning. The more you challenge your body and brain with exercise and learning, the better youll be able to maintain your quality of life for years to come.
Cupping 101: Everything You Need to Know About This Treatment
Athletes may want to try this ancient treatment to help heal soreness and ease muscle aches.
Can Exercise Help Prevent Dementia Later In Life?
Learn how working out can impact your brain health.
How Travel May Affect Your Workoutsand What to Do
You dont have to miss your daily sweat with these smart solutions.
Clinical Signs And Symptoms Of Parkinson
Parkinsonian gait known as shuffling gait presents as short steps, narrow-based with flexed knees and stooped posture. Four classic signs suggest a diagnosis of PD, including resting tremor, rigidity, bradykinesia, and postural instability. It is not necessary for all four to be present at the time of diagnosis.30,35 Resting tremors should not be confused with essential tremor. Essential tremor occurs with movements, has a frequency of 8 to 12 Hertz , and can be alleviated by alcohol or propranolol. Parkinsons pill-rolling tremor has a frequency of 3 to 6 Hz and usually involves the forefinger and thumb.36,37 Symptoms are oftentimes unilateral and when they progress to bilateral limbs, it has an asymmetrical pattern of involvement. PD is more likely to have a progressive prognosis with male gender, early-onset gait difficulty, and postural instability.
Paul Johns BSc BM MSc FRCPath, in, 2014
Don’t Miss: End Stage Parkinson Disease What To Expect
Gait Disorders Include Imbalance Shuffling Frequent Falls Staggering And Freezing
Gait disorders are very common in the adult population, increasing with age.
Sixty-two-percent of patients over the age of 80 have a gait disorder, whether from neurological or non-neurological cause. Ataxia refers to lack of coordination and can include staggering gait as well as uncoordinated arm movements, speech and eye movements. The spinocerebellar ataxias are a group of rare genetic neurodegenerative conditions which cause ataxia, among other symptoms.
Every patient with a gait disorder should be evaluated by a neurologist to assess for treatable neurological causes. Evaluation generally entails a detailed neurological exam, blood work, and typically an MRI of the brain. Multifactorial gait disorders are more common than isolated causes. As an example, a patient with Parkinsons disease may also have glaucoma and lumbar spinal stenosis, all of which could affect the risk of falls.
There are four neurological components to maintaining balance/gait and preventing falls:
Sensory ataxia due to peripheral neuropathy
Spg1/l1 Cam Knockout Mice
Mutations in L1 CAM cause X-linked CRASH syndrome , MASA syndrome , and X-linked hydrocephalus associated with spastic paraplegia. Two different L1 CAM knockout mice have been studied. One was produced by inserting a Tkneo cassette into L1 CAM exon 8 . This resulted in L1 CAM protein of reduced size and quantity. In addition to hindlimb motor impairment , these mice were less sensitive to noxious stimuli compared to control animals. Histologic analysis of these mice revealed reduced size of the corticospinal tracts compared to normal controls.
The second L1 CAM knockout mouse was produced by replacing L1 CAM exons 13 and 14 with the neomycin resistance gene cassette. This resulted in the complete absence of L1 CAM protein in these animals. These animals demonstrated a number of brain defects, including reduced size of the corpus callosum and hippocampus, enlarged ventricles, septal abnormalities, and abnormal migration of mesencephalic dopamine neurons . These results provide evidence that L1 CAM plays an important role in brain development, particularly that of the corticospinal tracts and the migration of dopamine neurons. Furthermore, studies of L1 CAM mutations in humans and mice illustrate that the HSP syndrome may be caused by developmental disturbance of corticospinal tract formation rather than corticospinal tract degeneration.
Raman Malhotra MD, Alon Y. Avidan MD, MPH, in, 2008
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Trouble Moving Or Walking
People without PD do not think about their walking. Their arms naturally swing, and their feet naturally land on the heels with each step. They can walk and talk and carry bags, purses and plates of food without difficulty.
Individuals with PD tend to lose their automatic movements. Especially as Parkinsons advances, it may bring with it a variety of symptoms that are uncommon in early stages, such as problems with walking and poor balance . Feet begin to shuffle, and performing two tasks at once becomes more difficult. Turning becomes challenging, often leading to a freezing episode and sometimes a fall.
Parkinsons Disease Is a Movement and Sensory Disorder
People with PD have trouble regulating the speed and/or size of their movements. Movements are bradykinetic or hypokinetic .
Changes in the movement system lead to challenges controlling movements, including the following:
- Starting and stopping movements
- Linking different movements to accomplish one task
- Finishing one movement before beginning the next
Changes in the sensory system also lead to challenges, particularly noticing and correcting movement and voice issues, including the following:
- Slowness or smallness of movements
- Lack of movement
- Changes in posture
- Changes in voice volume
Walking Changes
There are many PD-related walking changes:
Managing Walking Changes
Walking Tips
Turning Tips
Freezing
Managing Freezing
Tips for Care Partners
Freezing is a significant cause of falls.
Balance Orientation And Postural Control
Balance is the ability to automatically and accurately maintain your center of mass over your base of support. Postural orientation is the ability to control the segments of your body in relation to one another and to gravity, taking into account the environment and whatever task is being performed. Postural control involves both balance and postural orientation.
Control of posture has both musculoskeletal components and motor processes, which organize the muscles into neuromuscular synergies. Balance also involves neural componentssensory and perceptual processesthat integrate input from the somatosensory, visual, and vestibular systems, as well as higher level processes that contribute to anticipatory and adaptive aspects of postural control .
Poor balance and unstable posture are commonly observed motor symptoms in those with PD. Until recently, it was thought to occur relatively late in the course of the disease. This is reflected by the Hoehn and Yahr scale, in which postural instability is represented only in the advanced stages of the disease . However, there is significant evidence that changes in postural control occur even in the early stages of Parkinsons and, although there is fluctuation, generally increase over time .
You May Like: Best Mannitol For Parkinson’s
Physical Therapy Can Help
In addition to medication, physical therapy can help with walking. There are several strategies that can be used to overcome freezing episodes.
Strategies include taking a high marching step, counting to three before stepping, or walking along to the rhythm of a metronome. Using visual cues such or stepping over a target such as a laser beam or line on the floor can also help with gait.
Assistive devices such as walkers or canes can be helpful in reducing the risk of falling.
Engage with the community by asking a question, telling your story, or participating in a forum.
What Shoe Features Are Important For A Shuffling Gait
Buying the right proper footwear for seniors is crucial. Many seniors might think its better to switch to slippers or just go barefoot, but both are statistically almost twice as likely to lead to falls.
So, what should you look for in a great shoe for shuffling gait? The Vestibular Disorders Association offers this advice:
- Heel Height An inch or less. Higher heels negatively impact gait.
- Sole Hardness Thin, hard soles require less muscle activity to keep balance in check and positional awareness as compared to soft soles or thick hard soles.
- High VS Low Top Research is inconclusive for seniors at the time of writing, although higher collars support ankle joints and stability in younger athletes.
- Slip-Resistance Heel tread is ideal for the reduction of trips and slips. Rubber heels with bevels of 10 degrees are best. Having said that, some with gait might find too much friction/traction worsens their gait, as their feet seem to stick to the ground beneath them.
- Insoles Some shoes have a technology known as BalancePro. These raised-edge insoles reduce fall rates by almost half.
Read Also: Advanced Parkinson’s Disease Life Expectancy
Treating And Managing Gait Problems
Unfortunately, problems with gait, posture and balance tend not to respond as well to medications as other common motor symptoms, such as tremor, rigidity and bradykinesia . In addition, higher doses of medication over time to manage symptoms such as dyskinesia and orthostatic hypotension can sometimes increase problems with gait.
Nevertheless, there are lots of things you can do to help yourself and there are also experienced professionals who can offer very useful advice. Each case will be different and it is hard to generalise but depending on where you live your doctor will normally be your first contact and they may refer you to one or more of the professionals listed below.
The Most Important Thing
Do not neglect a slow shuffling gait. Do not neglect a festinating gait.
And finally, do not neglect other conditions which may cause similar walking problems.
These conditions have effective treatments.
Do not be afraid. See a doctor early.
| Caution: This information is not a substitute for professional care. Do not change your medications/treatment without your doctor’s permission. |
You May Like: Parkinsons Disease Hereditary
How Might Parkinson’s Affect Gait
Parkinsonian gait is a distinctive, less steady walk that arises from changes in posture, slowness of movement and a shortened stride. This is characterised by some, but not necessarily all, of the following:
- a tendency to lean unnaturally forwards in a stooped position when walking and, in some cases, a tendency to lean sideways when standing
- the head dropped forwards, with shoulders down, hips and knees bent
- steps taken on the front of the feet
- feet dragging on the ground, resulting in shuffling steps
- a reduced length of stride
- a reduced arm swing, particularly on the side on which Parkinsons is most noticeable.
If you develop this Parkinsonian gait you may experience some of the following problems:
- slowness
- start hesitation – a hesitation in initiating movements such as walking
- difficulty making a turn due to slowness, stiffness or instability
- difficulty making transfers, e.g. getting out of a chair or bed
- freezing – a sudden inability to start or continue walking, as if glued to the spot
- postural instability which makes falls more likely
- festination – progressively shorter but accelerated steps forward, often in a shuffling manner or as if falling forwards, in an attempt to maintain the position of the feet beneath the forward moving trunk. This tends to occur in later in Parkinsons.
Underactivation And Overactivation Related To Parkinsonian Gait
The present Parkinson’s disease patients revealed the gait-induced underactivation in some brain areas, as well as the overactivation in other areas. Lateralization of these areas could be related to the laterality of walking difficulty in Parkinson’s disease, which was not evaluated systematically in this study.
Cortical motor areas
A medial part of the underactive left frontal region is consistent with the pre-SMA, the function of which is more important in complex motor behaviour than in simple movements . Thus, this abnormality is likely to reflect poor integration of a complex motor regulation during walking. Previous activation studies showed that the SMA is impaired during upper limb movements in Parkinson’s disease and, furthermore, the SMA underactivation is ameliorated by treatments . On the other hand, in the present study the absence of the lateral premotor cortex-parietal overactivation that seemed to accompany externally triggered movements in the Parkinson’s disease patients supports the internally driven nature of the present treadmill-walk task. The left cingulate cortex, possibly belonging to a caudal part of the cingulate motor area , was shown to be overactive in the Parkinson’s disease patients, the significance of which needs to be clarified by further study.
Cerebellum
Parietal cortex
Other areas
Table 1
Don’t Miss: Parkinson Disease Autosomal Dominant
What Causes Parkinsonian Gait
While the cause of Parkinsons Disease itself is unknown, it is characterized by damage to the basal ganglia a group of structures that sit in the base of the forebrain and top of the midbrain. The basal ganglia is one of many stations in the communication circuit translating and moving neural impulses back and forth between the brain and the rest of the body.
The communication begins in the motor cortex the part of the brain controlling voluntary movement that creates a command, such as move your legs. This command moves to the basal ganglia, which produces dopamine, the brain chemical that facilitates the movement of messages between the brain and the body. The dopamine opens up the pathways for the signal to travel down to the rest of your body.
As Parkinsons progresses, the disease kills nerve cells in a subsection of the basal ganglia, the substantia nigra, which produces dopamine. As the supply of dopamine drops, the pathways between the brain and the body have trouble opening up. Without those pathways, the brain has greater difficulty sending impulses to the legs, arms, and other parts of the body involved with walking.
The body begins exhibiting symptoms such as inability to control the length and speed of steps, as well as decreased range of motion and sudden increases in pace . These are the typical symptoms of the small, shuffling steps that exemplify Parkinsonian gait.
Why Does Parkinsons Cause This Specific Gait Disorder?
Beyond The First And Second Moments: Fractal Analysis Of Pd Gait
Above, we described the changes in gait in PD that are related to the mean stride length or measures of gait variability, typically quantified as the standard deviation or the coefficient of variation of the stride time . While these gait features are important and describe much of the observable changes in PD, they fail to account for and explain a more subtle alteration in the gait of PD. In particular, they do not examine the dynamics of gait, i.e., how gait changes over time, from one stride to the next within a given walk. Two time series can have identical means and variance but with very different ordering or dynamics . There are many ways to capture and quantify such properties , , , , , , , , , , , , however, in this review, we focus on the fractal property of gait.
Example of time series of stride time during 1 h of walking in a healthy young adult at slow, normal, and fast walking rates, and below, after the fast data set is randomly shuffled. While there are subtle effects of gait speed, DFA shows that there is fractal scaling at all three gait speeds. When the data are randomly reordered , the slope becomes 0.5, reflecting white noise and an absence of fractal scaling . Data can be downloaded from www.physionet.org. Strictly speaking, Figs. should be plotted as discrete points rather than points joined with lines. The points are joined together as a continuous line, however, since this makes it somewhat easier to visualize the dynamics.
Don’t Miss: Parkinsons Disease Fatigue
Correlations Between Gait Parameters And Cognitive Domains
Results of correlations between cognitive domain and gait parameters are shown in . Step length and stride length were significantly associated with K-MMSE total score . Among cognitive domains, registration, attention/calculation, and visuospatial function were positively correlated with step length and stride length. In addition, visuospatial function was significantly associated with speed .
Changes In Fractal Properties Of Gait In Pd
What happens to the long-range correlations of gait in patients with PD? Perhaps not too surprisingly, among patients with PD, the memory in gait breaks down and the stride-to-stride fluctuations in gait now become very similar to white noise or random fluctuations. Figure shows an example of the times series of the stride time of a patient with PD, before and after the time series is randomly shuffled, artificially removing any memory and correlations. Visually, there is no difference between the original time series and the randomly shuffled time series. The DFA scaling exponent becomes close to 0.5 . Similar results were observed for a group of patients with PD demonstrating that the long-range scaling and fractal-like behavior are reduced and the stride-to-stride fluctuations become more random.
Gait rhythm dynamics in a patient with PD. On the left, time series are shown before and after random reordering of the data. Note that the temporal structure of the time series looks similar before and after reordering. This impression is confirmed using DFA . The slopes for the original data and the reordered data set are both close to white noise .
Recommended Reading: Can U Die From Parkinson Disease