Exploring The Clinical Burden Of Off Periods In Parkinson Disease
Supplements and Featured Publications
ABSTRACT
Parkinson disease, the second-most-common neurodegenerative disorder, affects approximately 1 million individuals in the United States, and this number is projected to increase to 1.2 million by 2030. Characterized pathologically by degeneration of dopaminergic neurons, with widespread pathology in nondopaminergic systems, Parkinson disease leads to an array of motor and nonmotor symptoms that can significantly impact an affected individuals quality of life. Treatments for Parkinson disease typically focus on controlling the motor symptoms of the disease, including treating OFF periods when motor symptoms return. OFF periods can occur for many individuals with Parkinson disease, especially as the disease progresses, and can pose a substantial burden to those with the disease and their caregivers. Available treatments for OFF periods may help alleviate this burden.
Am J Manag Care. 2020 26:S255-S264.
For author information and disclosures, see end of text.
Introduction
Diagnosis of PD usually occurs after age 50 years, and incidence rises with increasing age.1 In most populations, incidence of PD is twice as common in men as in women.1 In a population-based study conducted in Olmsted County, Minnesota, incidence was observed to increase over a 30-year period, particularly in men 70 years or older .4
Etiology
Diagnosis of Parkinson Disease
Symptoms of Parkinson Disease
Nonmotor Symptoms
How To Help Reduce Episodes
Off times become more common after people with PD have been taking medication for a longer time and as their disease progresses. While the presence of off times happens as a normal progression of PD, there are things that can help manage or reduce these episodes:
Statistics About Off Periods
Currently, it is estimated that approximately 350,000 people with Parkinsons in the United States experience OFF periods.11-13 They can occur throughout the day, can be unexpected, and may appear more often over time.3,7,14
As the disease progresses, people with Parkinsons will experience symptom return.7,8
In a study of 617 Parkinson’s patients, ~50% of a subset with disease duration of 5 years experienced OFF symptoms7
Another study following people with Parkinson’s for 15 years after diagnosis found that 50 out of 52 experienced OFF periods8
Time spent in OFF periods can really add up. In a 2014 survey of more than 3,000 people with Parkinson’s conducted by the Michael J. Fox Foundation, two-thirds of respondents reported having more than two hours of OFF time per day. Twenty-two percent of those surveyed were OFF 2-3 hours a day, 20% were OFF 3-4 hours a day, and 22% were OFF more than 4 hours a day. That translates to15:
The unpredictability and frequency of OFF periods negatively impact the lives of patients with Parkinsons, affecting their quality of life.16
~70% of approximately 3,000 people with Parkinsons who participated in a 2014 Michael J. Fox Foundation survey reported OFF periods at least twice a day.15
Also Check: Can Parkinson’s Run In The Family
Spotlight On Emerging Therapy
Intranasal drug delivery can bypass the blood-brain barrier and nanotechnology is being used with selegiline and ropinirole to deliver these adjunctive treatments. A study using chitosan nanoparticles for pramipexole dihydrochloride has shown that some of these nanoparticles can diffuse across artificial membranes that resemble the BBB at percentages as high as 93.32%.2 The particles are very small and easily entrapped by cells studies show entrapment efficiency of 292.5 nm+/- 8.80 at percentages as high as 91.25%.2 A similar study showed intranasal administration of selegiline and chitosan nanoparticles to rats delivered 20-fold higher plasma concentrations and 12-fold higher brain concentrations of selegiline compared to rats given selegiline orally.10 The higher concentrations of these medications within the brain and increased uptake by cells leads to increased dopamine activity and better performance in locomotor activity.
Both the intranasal and sublingual formulations are to be available in late 2018 or early 2019.
The Physical And Emotional Effects Of Off Episodes
The majority of patients experience Parkinson’s disease ON/OFF time in the latter stages of the disease. 64% of people with PD reported having 2 hours or more of OFF time per day. Many of those same people feel frustrated and helpless when their medication stops working.
According to OFF Limits PD, there are four types of OFF episodes, each with different physical and emotional effects:
Morning OFF
Morning OFFs occur in roughly 60% of PD patients. They typically appear after a treatment-free night, making it difficult for people with Parkinsons to get up and on with their day. Symptoms may diminish after you take your first dose of Parkinsons disease medication, or they may linger throughout the morning. You may have a delayed ON or no ON at all. Morning OFFs can result in depression, lethargy, physical inactivity and pain.
Wearing OFF
Wearing OFF happens when the effectiveness of medication starts to deteriorate toward the end of a dose. Patients may feel frustrated and hopeless as they feel the medicine beginning to wear off and their symptoms returning. Not only does this take an emotional toll, but it can also be physically debilitating. The good news is, your doctor can help you manage your medication to reduce your wearing OFF episodes.
Delayed ON, partial ON, no ON
Unpredictable OFF
Also Check: Cardinal Symptoms Of Parkinson’s
What You Can Expect
Parkinson does follow a broad pattern. While it moves at different paces for different people, changes tend to come on slowly. Symptoms usually get worse over time, and new ones probably will pop up along the way.
Parkinsonâs doesnât always affect how long you live. But it can change your quality of life in a major way. After about 10 years, most people will have at least one major issue, like dementia or a physical disability.
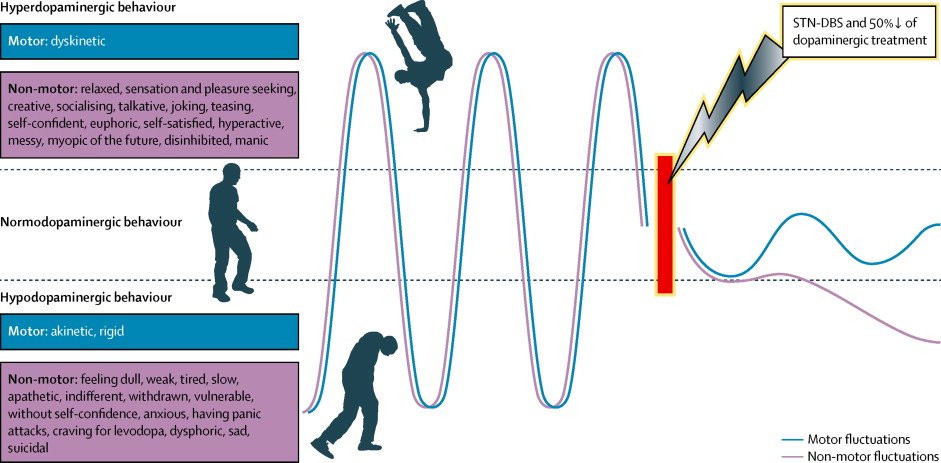
Dopaminergic Treatments And Their Side Effects
The overall goal of Parkinsons disease treatment is to alleviate the symptoms as much as possible with as few side effects as possible. No medication is perfect, but treatment should improve quality of life, and the benefits should outweigh the risks. Dyskinesia usually occurs when taking levodopa, but it can also occur with dopamine agonists, MAOIs, and COMT inhibitors.
Read Also: Can Parkinson’s Run In The Family
Mjff Offers Free Resources About Off Time
Two other posters assessed the potential benefits of Gocovri in patients who may be candidates for device-aided therapies, and the medicines impact on daily activities in people with Parkinsons.
In a poster titled Should Amantadine DR/ER be Considered Prior to Device-Aided Therapies for Parkinsons Disease? researchers conducted a post-hoc analysis of pooled data from 63 patients enrolled in the EASE LID and EASE LID 3 trials.
All of the patients, who had a mean age of 53 at diagnosis, had advanced Parkinsons, according to pre-defined criteria specifically, more than five doses of levodopa, two hours or longer of off time, and one hour or more of dyskinesia per day and were potential candidates for device-aided therapies to manage motor complications.
Of the 63 patients, 30 received Gocovri and 23 a placebo for 12 weeks, or about three months. The results showed that Gocovri increased on time without troublesome dyskinesia by a mean of 2.8 hours compared with placebo.
According to the researchers, these results suggest that Gocovri should be considered in patients otherwise eligible for device-aided therapies.
Another poster, Amantadine DR/ER-related Reduction in OFF and Dyskinesia Improved Patient-Rated Interference with Activities and Social Interactions, presented analysis results that showed that Gocovri significantly reduced patients off time and dyskinesia and had a positive impact on their daily activities.
How Continuous Dopaminergic Stimulation Can Help Prevent Or Minimize Off Times
As Parkinsons progresses, your brain produces less and less dopamine. This means it must rely much more heavily on levodopa to control your symptoms. Yet as Parkinsons progresses, many people begin to experience fewer benefits from their medications, and the benefits may also be less consistent. This can increase your wearing OFF periods and ON-OFF fluctuations.
Several years ago, Parkinsons researchers found that once dopamine terminals have degenerated a certain amount, intermittent doses of levodopa lead to dramatic peak and trough fluctuations, which ultimately results in the development of motor complications. They developed the hypothesis that continuous delivery of levodopaa concept known as continuous dopamine stimulation might be associated with a reduced risk of these motor complications.
The goal of CDS is to help the brain maintain more constant levels of dopamine it does this by imitating the brains normal continuous pattern of stimulating dopamine receptors. By keeping dopamine levels more constant over 24 hours, CDS can help reduce OFF times, improve sleep quality, and positively impact quality of life.
Subcutaneous apomorphine infusion
Carbidopa/levodopa enteral suspension
Deep brain stimulation
Extended-release medications
Don’t Miss: Parkinson\’s Life Expectancy
How Do You Know When Your Parkinsons Is Getting Worse
Oral dopaminergic treatments and Neupro reduced off time by 15-29% compared with the placebo. In patients given any of the oral treatments, dyskinesia increased by 12-31%, the analysis showed.
Gocovri was the only medication to significantly reduce both off time and on time with troublesome dyskinesia and was similar to DBS in its effectiveness.
The final poster, Analysis of Amantadine Formulations for OFF and Dyskinesia in Parkinson Disease, compared the effectiveness of Gocovri with other formulations of amantadine. These formulations included amantadine immediate release and amantadine IR/extended release .
The results showed that Gocovri reduced off time by 36% and dyskinesia by 27%. Meanwhile, other formulations led to a more modest reduction in off time, by 19%, and dyskinesia, by 13%.
Moreover, only Gocovri led to a statistically significant reduction in off time while providing significant improvements in dyskinesia. These improvements were associated with the early morning amantadine levels relative to bedtime administration not observed for the other two formulations.
Taken together, the analyses support the use of Gocovri for Parkinsons patients, according to Adamas.
Overall, we are pleased to offer patients a non-surgical treatment option that increases their GOOD ON time and doesnt necessitate a trade-off between treating OFF or dyskinesia, Quartel said.
Types Of Motor Fluctuations
Motor fluctuations take a variety of forms:
“On-off” phenomenon. You cycle between good control and periods of symptoms. During the “on” times, your symptoms are well managed. In “off” periods, the problems come back.
Some people only get “off” periods when their levodopa starts to wear off. Others get symptoms at random times that aren’t related to their medicine. Your doctor may prescribe add-on medications which can lessen the “off” times.
Wearing off. The effect of your levodopa starts to fade before it’s time to take the next dose. You might be tempted to take your medicine earlier than usual to prevent symptoms.
Delayed “on.” You have to wait longer than usual after you take levodopa for your symptoms to improve. This delay can happen when you take your first dose in the morning. It’s also common after meals, because the protein in your food can cause the medicine to get absorbed more slowly.
Delayed “on” is more common with time-release versions of levodopa. These drugs take a while to get from your stomach into your bloodstream and then travel to your brain.
Partial “on” or dose failure. Partial “on” means that your symptoms don’t fully improve after you take a dose of levodopa. A dose failure is when you don’t feel any better after taking your medicine.
You’re more likely to have freezing during an “off” period.
Dyskinesia. This is uncontrolled twitching, jerking, or other movements. It can affect one limb, such as an arm or leg, or your whole body.
Recommended Reading: Parkinson’s Disease And Life Expectancy
Characteristics Of Eligible Studies
Studies were published between 2007 and 2016. The details extracted from studies are summarized in Tables to . Five studies were from the UK, three studies were from each of Spain, United States, and the Netherlands, two studies from each of Italy and Singapore, and one each from Denmark, Germany, Brazil, China, Russia, Austria, Norway, Australia, and France. One study involved participants in the United States and Canada and one from United States, Australia, and multiple European countries. All studies involved patients four studies additionally involved carepartners, and one study involved physicians. Twelve studies gathered data using questionnaires or scales and three used qualitative interviews. Twentythree studies evaluated the impact or experience of off periods in patients, three evaluated the impact upon carepartners, two papers addressed understanding of off periods, one study evaluated communication about off periods, and three studies evaluated a facilitator of communication about off periods. No studies evaluated behavioral interventions to promote or support knowledge or communication about off periods, and no studies identified barriers to communication.
Impact Of Off Periods On Carepartners
Three studies reported on the impact of off periods on carepartners of patients ., , Carepartners need to play a more active role both to help patients in public and at home during off periods. Patients’ reluctance to leave the home because of off periods has implications for carepartners, given that they are forced to stay home more often, or be prepared to return home early should an off periods occur. Additionally, off periods force patients and carepartners to compromise and develop strategies that allow the person with PD to get the help they need, but, at the same time, allow spouses to be able to do the things they like to do. Carepartners of patients residing in nursing homes expressed the need for more emotional support, particularly related to off periods.
Don’t Miss: Parkinsons Life Span
What Is The Wearing Off Symptoms For Parkinsons Disease
Wearing off symptoms characteristically occur when the impact of levodopa medication come down / diminish before the time of the next dosage. The symptoms of Parkinsons disease is expected to return or even worsen before the next dosage of levodopa is scheduled, and then again improve after the patient is given the next dose. When the medication works and its effects can be seen, it is said the patient is on during that time, and again the when the effect of the medication worn out, it is said that the patient is in off phase. Thus, cycle is also called the on-off episode of Parkinsons disease.
What Causes Off Episodes
More research is needed to understand the cause of OFF episodes. Experts believe that fluctuations in dopamine levels play a role.
Dopamine is a neurotransmitter that carries signals between nerve cells. Low levels of dopamine contribute to symptoms of PD.
When you take levodopa, your body converts it into dopamine. This reduces symptoms of PD. As your body uses up each dose of levodopa, your dopamine levels begin to fall. This drop in dopamine may cause an OFF episode.
Many people with PD also have gastrointestinal complications that interfere with their ability to absorb oral medications If you take oral levodopa, it may take some time for your body to absorb the medication. This may lead to a delayed ON episode.
Don’t Miss: Can Parkinson’s Run In The Family
How To Talk To Your Physician About On/off Periods
Even after youve taken time to notice, assess, and track what OFF feels like to you, communicating about your unique OFF experiences can still be challenging. One strategy to help is, as we explained above, taking a written tracker of your medication doses and symptom fluctuations throughout the day to all your physician appointments.
Another strategy is to have your care partner go with you to your appointments so your physician can get the full storythe one experienced by you as the person with Parkinsons and the one observed by your care partner.
Be proactive and speak up about your symptoms and any ON/OFF fluctuations you experience at all appointments. Never assume that your physician can guess what your symptoms are or that you even have them. Your appointment time with your doctor is limited, and unless they prompt you to discuss OFF in a specific way, you may miss some key information about your medication and how it is supposed to work. Take these questions with you the next time you go to get the conversation about OFF started.
- How long should it take my medication to start working?
- Should my medication be working the same throughout the day?
- What should I do if my medication begins to wear OFF before my next dose?
- What if I take a dose and nothing happens?
- Can I take my medication when OFF symptoms occur, even if its not time for my next dose?
You Dont Have To Have Off Times With Parkinsons
Everyone knows what it means to feel off, to feel like somethings just not quite right. But if youre living with Parkinsons, OFF times can be debilitating. The good news is that although many people with Parkinsons believe that frequent OFF periods are an inescapable part of the experience, there are strategies you can use to minimize, or even prevent, being OFF. In this post, well show you how.
Recommended Reading: Parkinson’s Disease Awareness Color
The Impact Of Parkinsons Disease
On September 22, 2015, the US Food and Drug Administration held a public meeting for individuals living with Parkinsons, their care providers, as well as other representatives to hear their perspectives on the most significant effects of the disease.* When discussing OFF periods, most participants described living with both daily motor and non-motor symptoms and expressed that the symptoms impact all aspects of their lives. A few individuals emphasized the unpredictability that OFF time brought into their lives on a daily basis. Participants brought up limitations in performing at work, caring for self and family, and maintaining relationships.20
*This includes a range of experiences and may not completely represent all individuals with PD.
Because of the multifaceted impact of OFF periods on patients with Parkinsons disease, the recognition of these periodswhile challengingbecomes an important part of ongoing disease management.9
