Caregiver Needs And Support
A caregiver refers an individual who provide ongoing care and assistance, without pay, for family members and friends in need of support due to physical, cognitive, or mental health conditions . Family caregivers are the greatest support of patients in advanced diseases especially when they wish to be cared for at home. On top of the caregiving role, the multiple roles played by the caregiver of palliative care patients include well-being enhancer, handyman in daily tasks, minimizer/manager of suffering, palliative care facilitator and responsible for the continuity of care, learner in care provision and decision-maker at the end-of-life .
While many PD patients felt their families were anxious or worried about them , most PD caregivers themselves indeed felt unprepared for their role . Particular challenges to PD caregiver are the cognitive, personality and behavioral changes that may occur, especially in advanced stages of disease .
Though at the mean time research on effective caregiver interventions in PD is pending, caregivers can benefit from information in internet resource and local social agents which provide generic support to caregiver. Referral to a clinical psychology may help caregiver in emotional distress. Bereavement care is also an integral part of the support to caregiver in end-of-life care.
Common Problems In Late Stage Parkinson’s
Parkinsons is a very individual condition and everyones experiences will be different but some of the common difficulties encountered in the late stage are:
Reduced response to Parkinson’s medication and re-emergence of symptoms – as Parkinsons medications become less effective over time, other physical symptoms may re-emerge and pain may worsen. If this happens the emphasis will be on minimising symptoms using other, more general medications. Any change in medication should always be discussed with your doctor who will monitor effectiveness or side effects on an on-going basis
Bladder and bowel problems – as Parkinsons medications become less effective, bladder control might be lost and bowel problems such as constipation may worsen. These can cause considerable distress if not carefully and sensitively managed. Your care team can prescribe various medications to help
Mobility and balance difficulties – mobility and balance may deteriorate, leading to falls and the risk of fractures. Depending on where you live, a physiotherapist and/or an occupational therapist will be able to help improve mobility and suggest strategies to minimise your risk of falling
Swallowing difficulties – a speech and language therapist will be able to help with any swallowing problem you experience. This can also help reduce the risk of aspiration pneumonia
For more information on symptoms see Symptoms.
Theory Of Pd Progression: Braaks Hypothesis
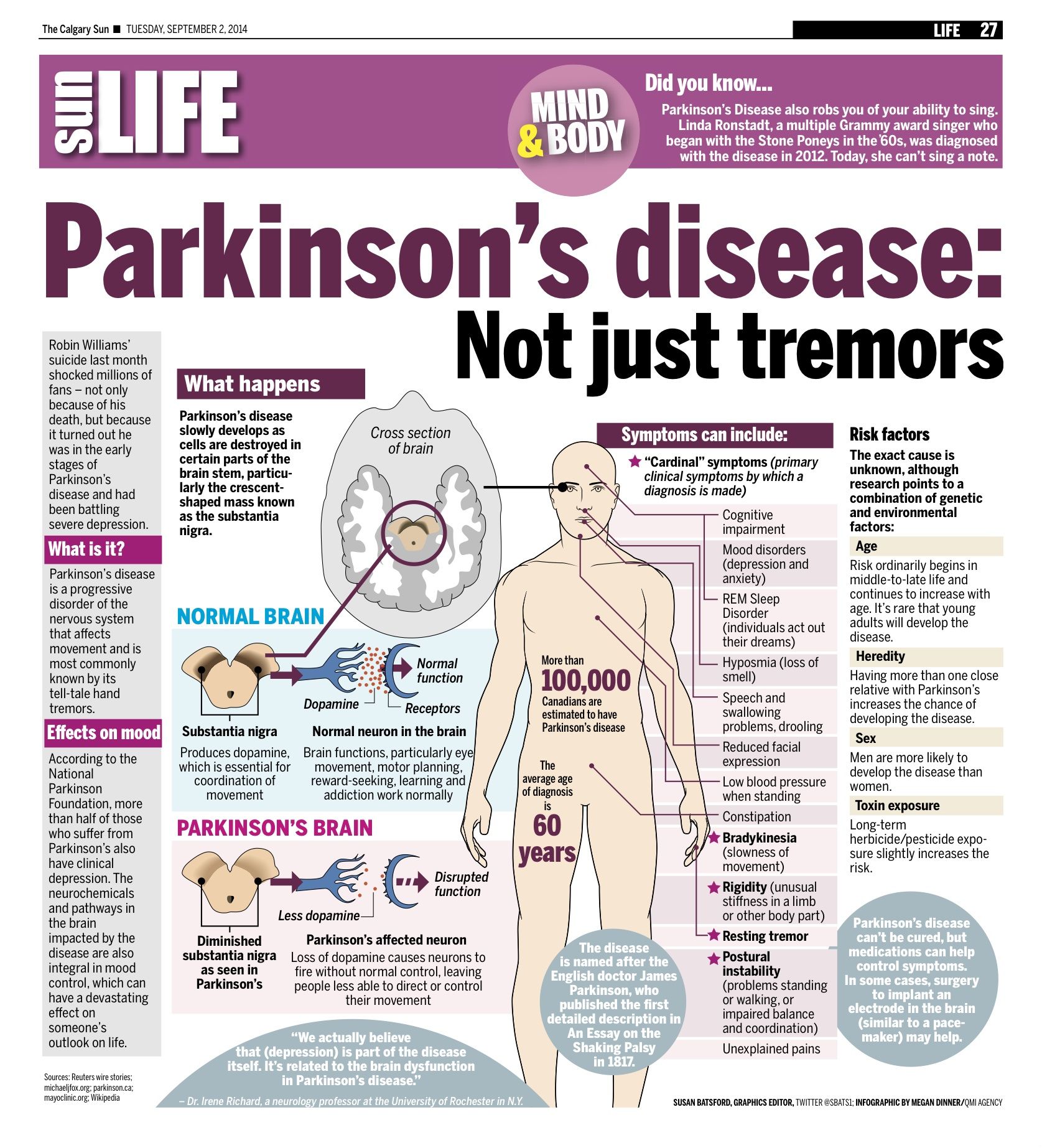
The current theory is that the earliest signs of Parkinson’s are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinson’s only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
You May Like: Where Do Parkinson’s Tremors Start
Parkinson’s Disease And Palliative Care
This page outlines the decline of Parkinson’s disease and helps those coping with Parkinson’s understand what a palliative care team provides. There is a brief discussion of when and how to get palliative care, an online quiz to determine if palliative care is right for your family and a link to a palliative care provider search tool.
Managing Care In Late Stages

, March 3, 2017
What to expect in the late stages of Parkinson’s disease and the challenges of caring with those difficulties and needs. Tips for helping someone overcome freezing, accomplishing activities of daily living as long as possible, managing medications and swallowing issues, and ways to minimize caregiver stress.
Recommended Reading: Is Anemia A Symptom Of Parkinson’s
Hospice Eligibility Of End
Since Parkinsons disease is progressive, patients need hospice care. If your family member or any loved one has been diagnosed with Parkinsons disease, expect that there will be a decline in their motor abilities. They will need professional nursing care to attend to their needs because it will be harder for them to speak and express their struggles.
Here are the things you need to observe to determine if the patient already needs hospice care:
- Difficulty in breathing and oxygen supply is necessary
- Difficulty in walking where a wheelchair is already needed
- Hard to understand speech
- Difficulty in eating and drinking
- More complications occur, such as pneumonia, sepsis, pyelonephritis, decubitus ulcers, and other comorbidities
What Happens In Stage 5 Parkinsons
Stage 5Stage 5stageParkinsons
When patients reach stage five the final stage of Parkinsons disease they will have severe posture issues in their back, neck, and hips. In endstage of Parkinsons disease, patients will also often experience non-motor symptoms. These can include incontinence, insomnia, and dementia.
One may also ask, how long does a person live with stage 5 Parkinsons? Parkinsons Disease is a Progressive DisorderIndividuals with PD have a somewhat shorter life span compared to healthy individuals of the same age group. Patients usually begin developing the disease around age 60, and many live between 10 and 20 years after being diagnosed.
Herein, what happens in stage 5 of Parkinsons disease?
Stage Five of Parkinsons DiseaseStage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking.
What do Parkinsons patients usually die from?
But the most common cause of death in those with Parkinsons is pneumonia, because the disease impairs patients ability to swallow, putting them at risk for inhaling or aspirating food or liquids into their lungs, leading to aspiration pneumonia.
Recommended Reading: Is Thumb Twitching A Sign Of Parkinsons
Recommended Reading: How To Detect Parkinson’s Disease Early
The Progression Of Parkinsons Disease
Parkinsons develops differently in each patient. Some deteriorate to the end stage of Parkinsons rapidly, while others remain strong and active for years, and theres no clear explanation for why.
While exercise and physical therapy can slow disease progression, theres no known cure. Even the healthiest patients will eventually decline until the end stage of Parkinsons, when they are left completely dependent on family and caretakers.
For those with loved ones whove been diagnosed with Parkinsons, it helps to know the road ahead. An awareness of whats to come makes it easier to offer help as conditions decline, and ask for help when they become too much to manage alone.
Symptom Burden In Advanced Pd
There are established guidelines in management of motor and non-motor symptoms in PD. However, symptom burden in advanced PD is still high, and it has been reported to be of similar degree as in metastatic cancer .
The motor symptoms of PD progress over years and the Hoehn and Yahr scale is a commonly used system for describing this . After the honeymoon period in early years of PD when antiparkinsonian drugs usually provide excellent control over the motor symptoms of bradykinesia and rigidity, majority of patients begin to experience less reliable drug response upon disease progression. Patient would experience complications from the long-term drug treatment, including motor fluctuations and dyskinesia. In advanced PD, prominent motor symptoms, as reported in a cohort of 50 patients with stage 4 or 5 of Hoehn and Yahr, include severe akinesia, postural instability, freezing of gait, dysarthria and dysphagia .
Table 2
From the patients perspective, there is a recent questionnaire survey which included 814 PD patients who felt subjectively severely affected by their illness. The commonest reasons for feeling severely affected were mobility impairment , coordination problems , speech problems , and limited day-to-day activities , e.g., getting dressed and personal hygiene. Significant associations were observed between subjectively felt severe affectedness and Hoehn and Yahr, poorer health, higher nursing care level, and having no children .
Also Check: Should Parkinson’s Patients Drink Alcohol
Depression May Be An Early Symptom Of Parkinsons
Depression is one of the most common, and most disabling, non-motor symptoms of Parkinsons disease. As many as 50 per cent of people with Parkinsons experience the symptoms of clinical depression at some stage of the disease. Some people experience depression up to a decade or more before experiencing any motor symptoms of Parkinsons.
Clinical depression and anxiety are underdiagnosed symptoms of Parkinsons. Researchers believe that depression and anxiety in Parkinsons disease may be due to chemical and physical changes in the area of the brain that affect mood as well as movement. These changes are caused by the disease itself.
Here are some suggestions to help identify depression in Parkinsons:
- Mention changes in mood to your physician if they do not ask you about these conditions.
- Complete our Geriatric Depression Scale-15 to record your feelings so you can discuss symptoms with your doctor. Download the answer key and compare your responses.
- delusions and impulse control disorders
Developing A Holistic Approach
Utilising the principles of end of life care highlighted earlier in section 2.4 of this course, we will examine how to effectively manage and guide the person with Parkinsons, and those closest to them, through this end stage with the minimum of distress.
Promoting holistic assessment which respects the autonomy and choice of the person with Parkinsons is important and involves them in planning their end of life care through early discussions about advance care planning and Advance Decision to Refuse Treatment , as discussed in section 3.3
Holistic assessment in the end of life stage focuses on the physical, psychological, social and spiritual aspects of care for the person with Parkinsons. We will examine these in greater depth.
Read Also: What Causes Tremors Besides Parkinson’s
How Can Friends And Carers Of People With Parkinsons Disease Better Cope With End Of Life
Grief is always stressful for friends and family. But preparing for end of life can help them to cope with sorrow and mourning. It helps when the wishes of our beloved family members have been discussed and taken into account, and there has been some relief in their last days and passing.
Attention must be paid to carers problems and needs, as well. Supporting a person at the end of life can be complex. Carers are part of the team supporting a person with Parkinsons disease but on the other hand, they may need support themselves. Thats why end of life management should involve caregivers, to help improve quality of life and satisfaction of the whole family.
When saying goodbye to a close family member, it is important to feel that everything was done in their favour in the last days and years.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Recommended Reading: Is There A Treatment For Parkinson’s Disease
Why Is It Important To Apply These Principles Early In The Trajectory Of Parkinsons
As we have worked our way through section 2 we have made several references to the need for palliative care principles to be introduced early in the trajectory of Parkinsons. The key reasons for early introduction are summarised below:
- Research has highlighted the benefits of early introduction of palliative care principles in management of Parkinsons .
- It encourages professionals to have open and honest conversations about the advanced phase of Parkinsons and to have early discussions about the clients preferences and wishes for their care and management in the advanced and end of life stages.
- It supports the benefits of advance care planning and allows the client to discuss issues around lasting power of attorney, Advance Decision to Refuse Treatment and decisions around resuscitation.
- Empowering the health professional to have these conversations earlier with clients promotes person-centred care and a holistic approach to end of life care.
- There is a high incidence of cognitive impairment and dementia in Parkinsons as the condition progresses. Therefore the early introduction of the principles of palliative care, which allows them to discuss wishes, fears and concerns for their future, will provide the client with a sense of control and ownership of their future care.
What To Expect In The Late Stages Of Parkinsons Disease
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinsons Disease In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinsons Disease Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
Recommended Reading: Weighted Silverware For Parkinsons
Also Check: What Is The Latest Medicine For Parkinson
Days Before Death Symptoms
In the days before death, a series of physiological changes will occur. Their pulmonary system will start to degrade and the will become congested, leading to a tell-tale death rattle. Their breathing will also exhibit fluctuations, as they may begin to respirate up to 50 times per minute or as little as six. When exhaling, they may puff their lips. They may also begin to cough more frequently, but in general, the congestion itself is painless.
During their last days, your loved one may begin to experience hallucinations in which they talk to people who arent there or who have also died. It is important to maintain a close eye on your loved one if they begin exhibiting these symptoms. There is no guarantee for how long they may have left, and some people pass through this process faster than others.
Some common symptoms those a few days from death experience include:
- A drop in blood pressure
- The body temperature changes frequently
- Skin changing color or becoming blotchy
- Erratic sleeping patterns
How Hospice Care Can Help In End
Parkinsons hospice care is an added assistance for patients and their loved ones dealing with end-stage Parkinsons disease. The care can offer added support and ease in taking care of the patient until the last stages of Parkinsons before death.
Here are more of the benefits hospice care can provide to a Parkinsons disease patient:
- Comprehensive programs are included that can help in physical, emotional, and spiritual aid from therapists, volunteers, and other counselors.
- The nurse can orient families on end-stage Parkinsons disease and what to expect for the coming days as the disease progresses.
- The nurse can also monitor pain and other symptoms experienced by the patient and give the necessary treatments.
- Families will have peace of mind as the hospice team will provide aid 24 hours a day.
Also Check: How Does Stress Affect Parkinson’s Patients
When Should You Start Palliative Care For Parkinsons
You can start palliative care for Parkinsons at any time. Palliative care can help anyone who has a complex and progressive condition like Parkisons.
Although many people wait until their condition has progressed or until they are in the later stages of Parkinsons to seek out an option such as palliative care, you might get more benefit from starting this care earlier.
That way, youll have a supportive team with you over the years that can help you manage your diagnosis.
End Of Life Care Can Be A Difficult Topic To Discuss Do You Have Any Advice On Starting Or Having Conversations On This Subject
I agree, end of life discussions are not easy. We are often not used to thinking about death.
Conversations about end of life must respect patients readiness to discuss these delicate topics, step by step. There should be a choice to make, or not to make, decisions. After identifying care needs in a person with Parkinsons disease and providing suggestions for their management, healthcare professionals can share how the condition may progress when the patient is ready. This conversation might be about complications of late stages of the condition, and how specific palliative applications can help manage these problems.
Conversations might involve identifying the persons wishes about medical and non-medical aspects of end of life preferences for living at home or being cared for in a care home treatment preferences, including resuscitation wishes for the last moments of life and even funeral wishes. There might be a need to appoint a personal representative to the person with Parkinsons disease.
Don’t Miss: How To Improve Walking With Parkinson’s
What Makes Pd Hard To Predict
Parkinsonâs comes with two main buckets of possible symptoms. One affects your ability to move and leads to motor issues like tremors and rigid muscles. The other bucket has non-motor symptoms, like pain, loss of smell, and dementia.
You may not get all the symptoms. And you canât predict how bad theyâll be, or how fast theyâll get worse. One person may have slight tremors but severe dementia. Another might have major tremors but no issues with thinking or memory. And someone else may have severe symptoms all around.
On top of that, the drugs that treat Parkinsonâs work better for some people than others. All that adds up to a disease thatâs very hard to predict.
