Conditions Of Muscle Inflammation
Inflammatory diseases of muscle typically affect older adults and include conditions such as polymyalgia rheumatica , polymyositis and dermatomyositis. Some of these conditions respond well to steroids . Unfortunately, as explained above, steroids also cause muscle wasting and weakness.
Conditions of generalised tissue inflammation such as systemic lupus erythematosus and rheumatoid arthritis can cause muscle weakness. In a small proportion of cases of rheumatoid arthritis, muscle weakness and tiredness may be the only sign of the disease for some considerable time.
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
Examining Muscle Weakness And Rigidity In Parkinsons Disease
The sun peeks over the horizon, and before long Dad is up and at it. Its a boxing day, and he wants to time his medications to optimize control over his Parkinsons symptoms.
The other part of his routine revolves around his morning stretches. Muscle rigidity is the first obstacle that he faces when he wakes, and he chooses to confront it with a stretching practice.
Parkinsons disease claims multiple functions as it progresses. Understanding how the disease affects the patient may help to inform treatment decisions. Im a curious person, and Dads stretching routine makes me wonder if Parkinsons disease directly affects the way muscles work. I think about how muscle rigidity and weakness are linked and how others handle these symptoms.
Don’t Miss: What Are Early Warning Signs Of Parkinson’s Disease
Parkinson’s Disease Symptoms: Life Expectancy
Even though Parkinson’s disease is a serious, progressive condition, it is not considered a fatal illness. People who have Parkinson’s disease usually have the same average life expectancy as people without the disease.
But when the disease is in its advanced stages, Parkinson’s symptoms can lead to life-threatening complications, including:
- Falls that lead to fractured bones
- Pneumonia
- Choking
Thinking about the progression of Parkinson’s disease can be frightening. But proper treatments can help you live a full, productive life for years to come. And researchers hope to one day find ways to halt the progression of Parkinson’s and restore lost functioning.
What Vitamin Is Good For Weak Legs
You know to drink milk it can help fight leg heaviness when coupled with vitamin D. Vitamin D helps your body use calcium. But when youre deficient in this vitamin, your legs may feel weak, sore and heavy. A vitamin E deficiency may be another reason your legs feel heavy after a run.
Also Check: Symptoms Of Parkinson’s Disease In Humans
Opening The Medicine Box In The Mind: The Psychology Of Pain
In this 50-minute lecture, Beth Darnall, PhD explains how our experience of pain goes beyond the physical sensation of pain. It has emotional and psychological components that affect our ability to treat pain. She cites research to demonstrate that and shares 13 specific tips to reduce the experience of pain and increase treatment effectiveness. Audience questions follow the lecture.
Pain In Parkinsons Disease
Parkinsons patients suffer from the same pain other people have, often amplified by the motor dysfunction, but they also have additional pain problems unique to PD. Lower back pain and back of he neck pain are most common. Strengthening exercises or stretching may be helpful. Identifying the cause of the pain is essential in treating the pain. Treatments include physical therapy, medications, and alternative therapies like Reiki, acupuncture and massage.
Recommended Reading: Are Weighted Blankets Good For Parkinson’s
Genetic Conditions Affecting Muscles
Muscular dystrophies: these are inherited diseases which affect muscles. They are rare disorders but the best known and most common is Duchenne muscular dystrophy. This occurs in children and leads to gradual loss of muscle power from toddler-hood.
Some rare muscular dystrophies: these can present in adulthood and include Charcot-Marie-Tooth syndrome and the facioscapulohumeral dystrophies. They also cause gradual loss of power and function in muscles. Those who have these conditions may become wheelchair-bound.
Sarcoidosis: this is a rare disease in which clumps of cells form in skin, lungs and soft tissues, including muscles. The condition usually goes away after a few years.
Amyloidosis involves deposits of an ‘unhelpful’ abnormal protein called amyloid throughout the body, including muscles and kidneys.
Other rare causes: direct damage to muscles can occur in rare inherited metabolic conditions. Examples include:
- Glycogen storage diseases .
- Even rarer, mitochondrial diseases which occur when the energy systems inside muscle cells don’t work properly.
Myotonic dystrophy: this is a rare genetic muscle disorder in which muscles become extremely tired. Myotonic dystrophies are passed down through families and they tend to occur earlier and become worse as they move through the generations.
Could Noh Be The Cause
Symptoms of nOH, including dizziness, lightheadedness, muscle weakness, and feeling faint after standing, can occur in a person who is at any stage of Parkinsons disease. People often think these symptoms are part of their Parkinsons disease and are something they must learn to live with, but these symptoms may be a sign of nOHa separate condition that can also be managed.
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Assessing Fatigue In Parkinsons Disease
There is no single standard for assessing fatigue. As a subjective experience, like the symptom of pain, the person experiencing fatigue can best describe the impact it is having on their life. Fatigue is generally discussed during a physical exam and health history. Patients experiencing fatigue should talk to their doctor about their experience of fatigue, including what times of day symptoms are worse, how long fatigue symptoms last, and how fatigue is impacting their life. The physician can discuss treatments for depression or difficulties sleeping. In addition, the physician may ask for a sleep study to analyze problems with sleep.1
Read Also: Parkinsons Dyskinesia
Fourth Type Of Leg Pain Is Radicular Pain
In this case, the pain is caused by compression of nerves in lumbar area which results in weakness, numbness and tingling, and loss of reflexes from buttocks to foot in a distribution of a nerve. It can be acute or chronic, and can be worse with standing and sitting, or better with laying down. Of note: in my experience many patients including myself have these symptoms not because of physically herniated disc but rather by the stretching of a nerve in the canal as it exists due to severe musculoskeletal rigidity and abnormal posturing.
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
Read Also: Parkinsons Dementia Life Expectancy
Origins Of Breathing Disorders
The book by Leon Chaitow and co-authors cited above explains how breathing disorders are intrinsically linked to chronic stress and anxiety. The shallow, fast chest breathing through the mouth is a hallmark of the body preparing itself for the exertion of flight or fight due to a stress response. While this adaptive in acute stress situations, when stress is chronic and the body is spending a lot of time in fight or flight, the associated pattern of breathing becomes habitual, and eventually the system gets stuck in the new equilibrium of the CO2 intolerant state. However, the vicious circle work both ways, because overbreathing itself puts the body into a stress response state and feeds anxiety. A very good tutorial about the two way links between anxiety and breathing patterns is given by Robert Litman in the video below.
It is not surprising therefore that people with PD can present with disordered breathing associated with chronic stress and anxiety, since there are very significant overlaps between the other symptoms of chronic stress and those of Parkinsons Diseases, and ingrained fight or flight behaviours are common to the pre-diagnosis background histories of people with PD. Conversely, it is important to note that techniques which have been developed to treat breathing disorders should also help to decrease the symptoms of PD, including reduction of anxiety and increasing resilience to stress.
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
Don’t Miss: Freddy Roach Illness
Tips For Dealing With Chronic Pain
Chronic pain is one that last more than 3-6 months , or pain that extends behind the expected period of healing. This blog post explains the different types of pain caused by Parkinsons disease and how to address pain brought on by the disease, by medications, or by comorbid disease. It is always best to treat pain before it becomes chronic.
How To Deal With The 6 Common Causes Of Leg Pain In Pd
Severe leg pain is a common complaint from people with PD. Lately, it is understood that central pain is common to Parkinsons disease, and can even be the first sign of PD, usually bilaterally. This blog post lists six causes of lower limb pain, and the importance of treating it. Treatments depend on properly identifying the source of pain. Some treatment suggestions are included.
Read Also: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Primary Or True Muscle Weakness
This shows itself as an inability to perform what you want to do with a muscle, even the first time you try. There is a reduction in the force which the muscle can exert, however hard you try. The muscle is not working properly – it has become abnormal.
When this kind of weakness occurs the muscles are often floppier than usual and reduced in bulkiness. It can happen, for example, following stroke. It is also seen in a condition called muscular dystrophy . Both of these conditions result in weakened muscles which cannot move the usual load. It’s a real change in muscle power.
A Bottle Neck To Neurological Health
I have noticed that a lot of people with Parkinsons Disease, and other neurological disorders too, such as Alzheimers, suffer with severe neck pain and/or stiff, rigid necks. In terms of neurological problems, our necks can be a pinch point – a constricted passageway or tunnel, through which all the superhighways between our brain and the rest of our nervous system and organs, and from there, out into the far reaches of our fingers and toes, must pass. All of our utilities, the two-way electrical wirings, the broadband and telegraph wires of the nervous system, the water and air supplies, the chemical pipelines providing nutrients and the sewer pipes taking away the excreta of the brain, must pass through this narrow gap. This is no ordinary tunnel: to keep these utility supplies open and running, it was designed to keep on moving itself and in truly extraordinary ways of flexible motions.
Even slight damage or stiffening up of the neck can cause constrictions or interruptions of these important electrical and chemical flows. For oxygen and nutrients that enter through the mouth or nose, it is double jeopardy, as they have to pass through the bottle-neck twice, down into the lungs or to the gut, and back up again to get the brain. The neck is therefore a primary attention site for progressive symptom reduction strategies. In this article, we look at aspects of the neck and consider what we can do to improve our lot.
Read Also: Scale Of Prodromal Symptoms
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinsons disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable reducing symptoms during on periods and no longer controlling symptoms during off periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they cant. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
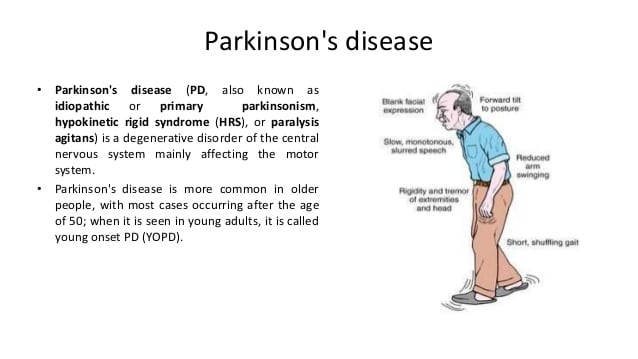
What Is Parkinsons Disease

Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
You May Like: Can Parkinson’s Run In The Family
Leg Pain And Parkinson’s
Interestingly enough, one of my early symptoms of the disease was deep searing pain in my left leg, the type of pain my grandma had complained about many times. Initially this type of pain was worst in the morning as well as at night, making me think is was some sort of fasciitis. However not only did typical anti-inflammatories and muscle relaxants not alleviate my pain but pain worsened over time to a constant burning pain that felt as if someone was tearing the muscle and pouring hot oil on it. The pain was so excruciating it was permeating into all aspects of my life. I was constantly in need of deep tissue massage asking my husband to massage my legs just as my grandmother had asked of us time and time again. This helped only temporarily.
Which brings me to the four types of leg pain in PD.
Muscle Weakness And Rigidity
As his Parkinsons progresses, Dad complains that his stiffness is slowing him down. The frequency and intensity with which it occurs seem to be increasing. To better understand the disease and how it relates to the body, I decided to explore the research.
In an abstract of a literature review published by the American Journal of Physical Medicine & Rehabilitation, the authors stated that isokinetic muscle strength was decreased in patients with Parkinsons disease and that muscle weakness was not specifically related to tremor or rigidity.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Why Do My Legs Feel Like They Are Going To Give Out
Causes of nerve damage include direct injury, tumor growth on the spine, prolonged pressure on the spine, and diabetes. A spinal cord injury. Spinal cord injuries are among the most common reasons that legs give out. These injuries vary in severity but should always be evaluated immediately by a spine specialist.