Symptoms Of Parkinsons Disease
Parkinsons has four main symptoms:
- Tremor in hands, arms, legs, jaw, or head
- Muscle stiffness, where muscle remains contracted for a long time
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include:
The symptoms of Parkinsons and the rate of progression differ among individuals. Early symptoms of this disease are subtle and occur gradually. For example, people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly, or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinsons. They may see that the persons face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinson’s disease often develop a parkinsonian gait that includes a tendency to lean forward take small, quick steps and reduce swinging their arms. They also may have trouble initiating or continuing movement.
Symptoms often begin on one side of the body or even in one limb on one side of the body. As the disease progresses, it eventually affects both sides. However, the symptoms may still be more severe on one side than on the other.
Medications And Parkinson’s Symptoms
Taking certain medicationsspecifically ones that block the action of dopaminecould cause Parkinson’s disease symptoms. It’s a condition called drug-induced parkinsonism, and while it isn’t Parkinson’s disease itself, it can look and feel a lot like it.
Here are some of the drugs that can cause Parkinson’s disease symptoms:
- Anti-nausea medications
- Drugs that treat hyperkinetic movement disorders
Keep in mind that even though these medications could cause symptoms similar to Parkinson’s, they don’t cause the disease itself. And most of the time, the symptoms go away within hours or days once you stop taking that drug, per the Parkinson’s Disease Society.
In some cases, the Parkinson’s symptoms don’t go away after a person stops taking the medication that led to them, and they’re eventually diagnosed with Parkinson’s disease.
Researchers don’t think that the medication was the cause of Parkinson’s in those cases, but that those individuals’ dopamine levels were already depleted, and the side effects of the drugs revealed their underlying Parkinson’s disease. Put another way, the medication was the “straw that broke the camel’s back,” according to the American Parkinson Disease Association.
Research on what causes Parkinson’s disease continues to grow. If you experience symptoms of Parkinson’s, such as a hand tremor, slowed movement, balance problems, or changes in your speech or writing, connect with a doctor to diagnose the condition.
Statins And Parkinsons Disease
In October 2016, a study abstract was presented at the American Neurological Association Conference that negated presumed beliefs about Parkinsons disease and statin use. The senior author, Dr. Xuemei Huang, MD, PhD, vice chair for research at Penn State College of Medicine, Hershey, had done multiple studies looking at the relationship between statin use and Parkinsons risk.1 Statins were thought be protective against neurodegenerative disease, but the study of 20,000 patients did not endorse this assumption. MarketScan Commercial Claims and Encounter databases from 2008 to 2012 were searched for patients between age 40 and 65 who were identified as having PD on diagnosis codes, anti-Parkinsons medication use, or having Deep Brain Stimulation surgery. These patients were then cross-referenced with cholesterol lowering medication use in the hopes to find evidence that supported prior smaller studies showing a protective effect. However, researchers found a statistically significant higher prevalence of Parkinsons disease after adjusting for confounders and comorbidities. To see if this was true for other neurodegenerative disease, data on Alzheimers patients was also pooled but this did not show any significant association.
Recommended Reading: Can Agent Orange Cause Parkinson’s Disease
What Medications And Treatments Are Used
Medication treatments for Parkinsons disease fall into two categories: Direct treatments and symptom treatments. Direct treatments target Parkinsons itself. Symptom treatments only treat certain effects of the disease.
Medications
Medications that treat Parkinsons disease do so in multiple ways. Because of that, drugs that do one or more of the following are most likely:
Several medications treat specific symptoms of Parkinson’s disease. Symptoms treated often include the following:
- Erectile and sexual dysfunction.
- Hallucinations and other psychosis symptoms.
Deep brain stimulation
In years past, surgery was an option to intentionally damage and scar a part of your brain that was malfunctioning because of Parkinsons disease. Today, that same effect is possible using deep-brain stimulation, which uses an implanted device to deliver a mild electrical current to those same areas.
The major advantage is that deep-brain stimulation is reversible, while intentional scarring damage is not. This treatment approach is almost always an option in later stages of Parkinson’s disease when levodopa therapy becomes less effective, and in people who have tremor that doesnt seem to respond to the usual medications.
Experimental treatments
Researchers are exploring other possible treatments that could help with Parkinsons disease. While these arent widely available, they do offer hope to people with this condition. Some of the experimental treatment approaches include:
Caveats And Technical Issues
The conclusions drawn from our observations must be evaluated in the context of the source material: tissue from non-human primates. Monkeys are not humans, and Parkinsons disease is a human condition. What cannot be disputed is that monkeys represent the closest phylogenetic model to humans when compared with other models commonly used in CNS research. Although in our opinion the analogy of non-human primate biology to human biology is a model that has yielded valuable insights, the limitations of the model must be acknowledged, and opinions on the value of the comparison vary widely. In the present context, several recent studies indicate that ageing humans, like ageing monkeys, exhibit little or no overt loss of substantia nigra dopamine neurons6466. Accordingly, this disparity between ageing and Parkinsons disease is shared by monkeys and humans. Furthermore, reports characterizing the motor behaviours of ageing monkeys indicate that aged monkeys exhibit behavioural signs that are consistent with the early stages of parkinsonism16,17,67.
Another caveat is that the tissue used in these studies was paraformaldehyde fixed and therefore could not be subjected to many common biochemical and molecular analyses. Future studies of these mechanisms are warranted and will be of great interest.
Don’t Miss: How To Treat Hallucinations In Parkinson Disease
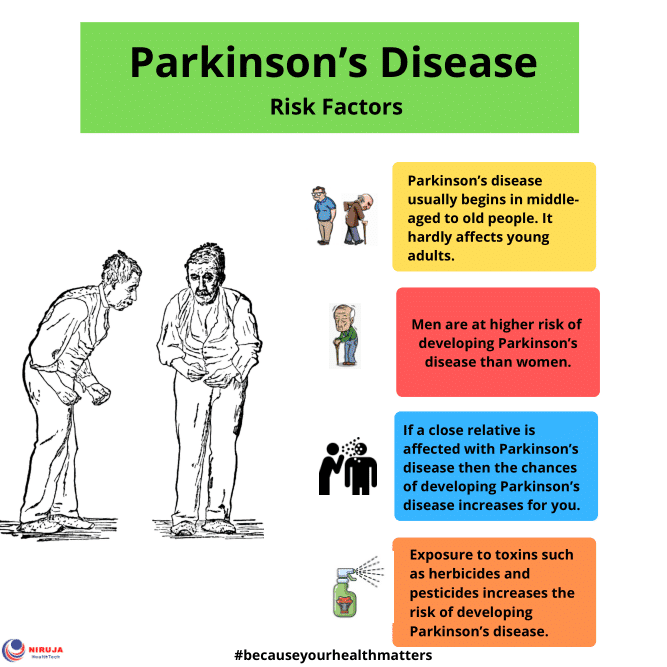
Parkinson’s Disease Risk Factors
Although a primary cause for Parkinson’s disease is yet to be identified, a number of risk factors are clearly evident.
Advancing age– Although there is the occasional case of the disease being developed as a young adult, it generally manifests itself in the middle to late years of life. The risk continues to increase the older one gets. Some researchers assume that people with Parkinson’s have neural damage from genetic or environmental factors that get worse as they age.
Sex- Males are more likely to get Parkinson’s than females. Possible reasons for this may be that males have greater exposure to other risk factors such as toxin exposure or head trauma. It has been theorised that oestrogen may have neuro-protective effects. Or, in the case of genetic predisposition, a gene predisposing someone to Parkinson’s may be linked to the X chromosome.
Family history– Having one or more close relatives with the disease increases the likelihood that you will get it, but to a minimal degree. This lends support to the idea that there is a genetic link in developing Parkinson’s.
– Post menopausal who do not use hormone replacement therapy are at greater risk, as are those who have had hysterectomies.
Low levels of B vitamin folate– Researchers discovered that mice with a deficiency of this vitamin developed severe Parkinson’s symptoms, while those with normal levels did not.
2002-2012©Parkinson’s Disease Information.
Medicines For Parkinsons Disease
Medicines can help treat the symptoms of Parkinsons by:
- Increasing the level of dopamine in the brain
- Having an effect on other brain chemicals, such as neurotransmitters, which transfer information between brain cells
- Helping control non-movement symptoms
The main therapy for Parkinsons is levodopa. Nerve cells use levodopa to make dopamine to replenish the brains dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapy such as nausea, vomiting, low blood pressure, and restlessness and reduces the amount of levodopa needed to improve symptoms.
People living with Parkinsons disease should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, like being unable to move or having difficulty breathing.
The doctor may prescribe other medicines to treat Parkinsons symptoms, including:
- Dopamine agonists to stimulate the production of dopamine in the brain
- Enzyme inhibitors to increase the amount of dopamine by slowing down the enzymes that break down dopamine in the brain
- Amantadine to help reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
Don’t Miss: Does Parkinson’s Come And Go
Ological Quality Of Included Systematic Reviews
Overall, none of the included SRs were judged to be of high or moderate quality with the AMSTAR-2. Seven SRs were judged to be of low methodological quality, while the remaining 39 were judged to be of critically low quality. Details regarding the methodological quality of the included SRs are shown in Fig. 2. The included SRs had relatively better performance on two out of the seven critical items, with more than 60%of the SRs rated positive for the following: used appropriate methods for statistical combination of the results , carried out an adequate investigation of publication bias and discussed its likely impact on the results of the SRs . The included SRs generally had poor performance for the remaining five critical items, with less than 30%of SRs rated positive for the following: only 2 provided a list of excluded studies, justified the exclusions, and used a satisfactory technique to assess the risk of bias in individual studies included in the review 4 registered a protocol and used a comprehensive literature search strategy, and 11 accounted for the risk of bias of individual studies when interpreting or discussing the results of the 1ptreview.
Fig. 2
The methodological quality of the 46 included systematic reviews based on AMSTAR-2 tool.
Note: AMSTAR-2 tool: Assessing the Methodological Quality of Systematic Reviews 2 tool.
Item 1: Did the research questions and inclusion criteria for the review include the components of PICO?
What Are The Early Warning Signs Of Parkinson’s Disease
Parkinsons warning signs can be motor symptoms like slow movements, tremors or stiffness. However, they can also be non-motor symptoms. Many of the possible non-motor symptoms can appear years or even decades ahead of motor symptoms. However, non-motor symptoms can also be vague, making it difficult to connect them to Parkinson’s disease.
Non-motor symptoms that might be early warning signs include:
- Sleep problems such as periodic limb movement disorder , rapid eye movement behavior disorder and restless legs syndrome.
Also Check: How To Deal With Parkinson’s
How Do I Take Care Of Myself
If you have Parkinsons disease, the best thing you can do is follow the guidance of your healthcare provider on how to take care of yourself.
- Take your medication as prescribed. Taking your medications can make a huge difference in the symptoms of Parkinson’s disease. You should take your medications as prescribed and talk to your provider if you notice side effects or start to feel like your medications aren’t as effective.
- See your provider as recommended. Your healthcare provider will set up a schedule for you to see them. These visits are especially important to help with managing your conditions and finding the right medications and dosages.
- Dont ignore or avoid symptoms. Parkinsons disease can cause a wide range of symptoms, many of which are treatable by treating the condition or the symptoms themselves. Treatment can make a major difference in keeping symptoms from having worse effects.
Leading Possible Risk Factors For Parkinsons
Genetic factors
Scientists estimate that less than 10% of cases of Parkinsons disease are primarily due to genetic causes. The most common genetic effect that triggers Parkinsons disease is mutation in a gene called LRRK2. The LRRK2 defect is particularly frequent in families of North African or Jewish descent. Mutations in alpha-synuclein have also been found to trigger Parkinsons, but these are quite rare. In most cases, no primary genetic cause can be found.
Other risk factors
There are other things that put an individual at higher risk for developing Parkinsons. The main risk factor is age, because Parkinsons disease is most commonly found in adults over the age of 50 . Men also have a higher risk of Parkinsons disease than women. The actual links between any of these factors and Parkinsons disease are not completely understood.
Recommended Reading: Does Dbs Work For Parkinson’s
Monitor Your Brain Health With Altoida
At Altoida, we are dedicated to providing a reliable, affordable, and highly accurate way to measure and monitor your brain health. We are building the worlds-first Precision Neurology platform and app-based medical devicebacked by 11 years of clinical validationto accelerate and improve drug development, neurological disease research, and patient care.
By completing a 10-minute series of and motor activities designed to simulate complex Activities of Daily Living on a smartphone or tablet, Altoidas device extracts and provides robust measurements of neurocognitive function across 13 neurocognitive domains. Our device measures and analyzes nearly 800 multimodal cognitive and functional digital biomarkers. Through the collection of highly granular data from integrated smartphone or tablet sensors, Altoidas device produces comprehensive neurocognitive domain scores. This data can be tracked longitudinally to reveal trends and patterns while flagging concerning ones.
This method, along with our innovative artificial intelligence, will pioneer fully digital predictive neurological disease diagnosis. In 2021, our device received Breakthrough Device designation by the FDA. Altoida’s platform has demonstrated the ability to predict conversion from Mild Cognitive Impairment to Alzheimer’s disease with a high degree of accuracy.
A Stochastic Acceleration Hypothesis
The clinically silent, presymptomatic progression of Parkinsons disease makes it difficult to study pathogenic mechanisms of dopamine neuron degeneration in the disease. Ageing is the strongest risk factor for developing Parkinsons disease, and by inference this suggests that changes in nigrostriatal dopamine neurons during normal ageing are related to those contributing to the pathogenesis of Parkinsons disease91,92. However, the association between ageing and Parkinsons disease has largely been based on increased incidence of Parkinsons disease diagnosis with advancing age, a finding that is consistent across geographic, cultural and ethnic boundaries13. Now, an increasing number of commonalities, ranging from molecular to functional, have been identified for changes in dopamine neurons that occur in normal ageing and those that occur in Parkinsons disease . It is our contention that the combined analysis of changes occurring in dopamine systems during normal ageing specifically those that vary between midbrain dopamine neurons that are vulnerable versus those that are resistant to degeneration in a species closely related to humans can provide meaningful insights into the pathogenesis of Parkinsons disease.
Don’t Miss: Does Having Parkinson’s Qualify For Disability
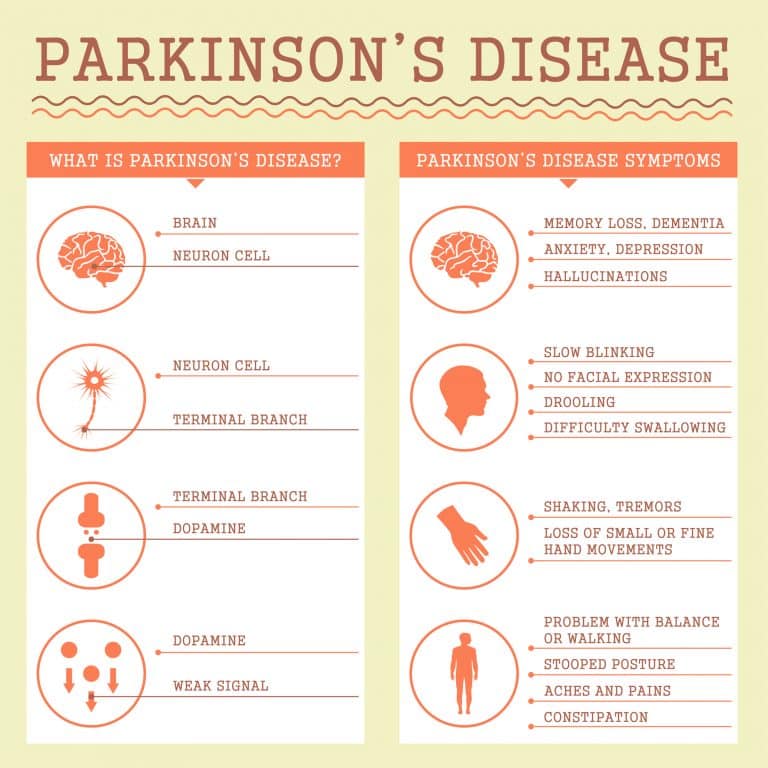
What Are The Symptoms
The best-known symptoms of Parkinson’s disease involve loss of muscle control. However, experts now know that muscle control-related issues aren’t the only possible symptoms of Parkinson’s disease.
Motor-related symptoms
Motor symptoms which means movement-related symptoms of Parkinsons disease include the following:
Additional motor symptoms can include:
- Blinking less often than usual. This is also a symptom of reduced control of facial muscles.
- Cramped or small handwriting. Known as micrographia, this happens because of muscle control problems.
- Drooling. Another symptom that happens because of loss of facial muscle control.
- Mask-like facial expression. Known as hypomimia, this means facial expressions change very little or not at all.
- Trouble swallowing . This happens with reduced throat muscle control. It increases the risk of problems like pneumonia or choking.
- Unusually soft speaking voice . This happens because of reduced muscle control in the throat and chest.
Non-motor symptoms
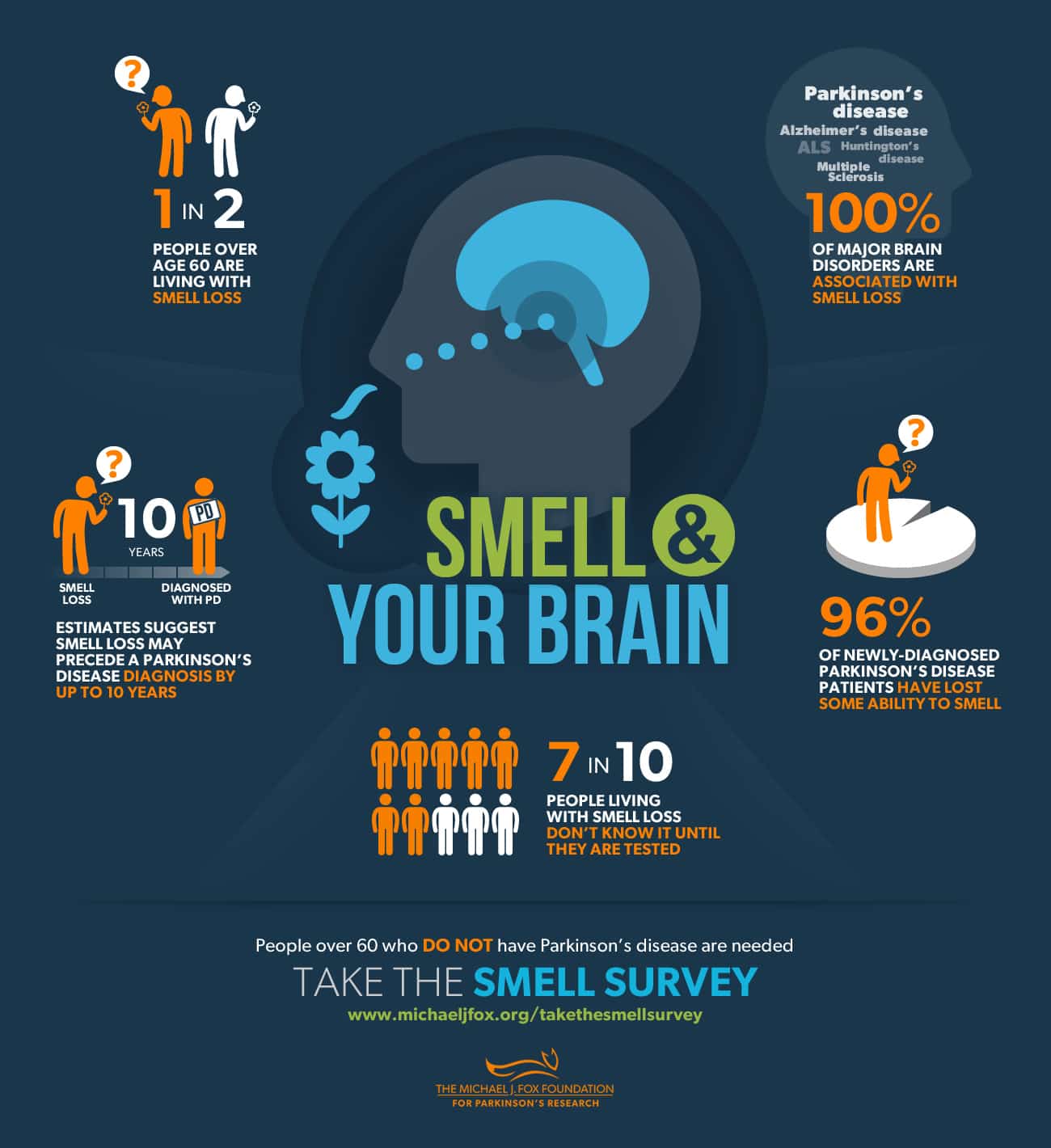
Several symptoms are possible that aren’t connected to movement and muscle control. In years past, experts believed non-motor symptoms were risk factors for this disease when seen before motor symptoms. However, theres a growing amount of evidence that these symptoms can appear in the earliest stages of the disease. That means these symptoms might be warning signs that start years or even decades before motor symptoms.
Non-motor symptoms include:
Stages of Parkinsons disease
Lewy Bodies And Alpha
In addition to the dopamine deficiency and neuronal loss, PD is also associated with a buildup of intracellular inclusions inside the neurons, called Lewy bodies. Studies have shown that the Lewy bodies are made mainly of a protein called alpha-synuclein.
They are not seen in brain imaging studies but have been detected in research studies that examine the brains of people who had PD and donated their own brains to science for the purpose of research. There is no known treatment or method of removing the Lewy bodies at this time.
In PD, Lewy bodies are found in the substantia nigra as well as other areas, including the amygdala and locus coeruleus , the raphe nucleus , and the olfactory nerve . The functions controlled by these regions can be impaired in PD, although the symptoms arent as noticeable as the tremors and muscle stiffness.
Lewy bodies are also present in the brains of people who have Alzheimers disease and other types of dementia, and they are considered a sign of neurodegeneration.
Read Also: Does Pot Help Parkinson’s
Burden Of Cardiometabolic Risk Factors Differs Between Women Men With T1d
Women with type 1 diabetes had a better cardiometabolic risk factor profile but did not have a significantly lower cardiovascular disease event burden compared with their male counterparts.
Women living with type 1 diabetes have a lower burden of cardiometabolic risk factors compared with men with T1D, and women in the general population have a lower absolute risk of cardiovascular disease .
However, women with T1D do not have a significantly lower CVD event burden than men with T1D, according to research published in JAMA Network Open.
These findings suggest a greater clinical impact of cardiometabolic risk factors in women with T1D compared with their male counterparts, and further stress the need for optimized CVD risk factor management in women with T1D.
While the protection for CVD in women vs men in the general population is reduced in the presence of diabetes, several studies have found that the absolute risk of CVD remains similar or lower in women with diabetes compared with men with diabetes, the study authors wrote. However, several meta-analyses of prospective cohort studies have shown that the relative risk of CVD mortality and morbidity associated with type 2 diabetes is higher in women than in men, suggesting that the increase in risk associated with type 2 diabetes is higher in women than in men.
- waist circumference
- triglyceride levels
Women with T1D also experienced significantly higher pulse rates and hemoglobin A1c levels.
Reference