Inconsistency Or Lack Of Exercise Program
- Are you challenging your movement patterns and elevating your heart rate on a regular basis?
- Ill often speak about the imaginary fence line and giving up territory or PD.
- The less we challenge this boundary which are your personal limits, the more likely youre to give up movement independence.
Exercise And Physical Therapy Can Be Game Changers
Joining a Parkinsons-specific fitness program like Rock Steady Boxing helps you to strengthen your motor functions. This ultimately allows you to stabilize with more ease. Since Parkinsons patients often see a decline in motor skills, exercise can offer a good option for strengthening those skills. Rock Steady also uses portions of the class to teach Parkinsons patients how to fall.
According to Dad, About once a month or so, theyll put mats on the floor and show you proper falling and rolling technique. They try to do things in boxing thatll help people with different stages of Parkinsons.
While the exercise portion of Rock Steady Boxing is valuable in itself, learning how to fall helps mitigate risk as much as possible.
Freezing is a frightening phenomenon, but there are ways you can manage this symptom. Stay positive! Try to find Parkinsons fitness classes or challenge yourself with rhythmic solutions to freezing. Other patients have found that these strategies can assist in the management of motor-related functions.
What Are Freezing Triggers
Many people tell us that they can walk OK in a straight pathway, but freeze when something in the environment changes. These changes are known as Freezing triggers. For many people, they may include:
- Turning a corner
- Going through a narrow space
- Navigating a crowded space
- Going through doorways
- Doing two things at once, such as someone coming alongside of them and initiating a conversation
- Approaching a chair
Some people also experience something called start hesitation, which means there is a delay when they try to initiate movement. This happens BEFORE a person even takes their first step. For most people, this is a momentary paralysis of movement that they overcome in 1-2 seconds.
We also know that freezing becomes worse when a person feels stressed out or are rushing.
You May Like: Is There A Treatment For Parkinson’s Disease
Predictors Of Freezing: When Are People Living With Parkinsons Most Likely To Freeze
Freezing is common among Parkinsons patients, and is most often seen in those with long-standing symptoms.
A survey of 6,620 people living with Parkinsons disease found that 47% reported experiencing freezing regularly. Further analysis of people who reported freezing showed
- It was significantly associated with a longer disease duration and a more advanced stage of the disease.
- Episodes were more likely in men than in women and
- Finally, people who reported tremor as their main symptom were likely to also report freezing less frequently.
The results underline the necessity to develop appropriate countermeasures against this phenomenon, which is widely known to cause significant impairment of patients quality of life and as our data also showed may cause traffic accidents in licensed patients.
Source:
A previous study in 2001 has also established
- Risk factors associated with freezing where found to be at the early stages of the disease 1. the absence of tremor and 2. PD symptoms being mostly as a gait disorder early in the disease experience.
- The development of freezing over the course of the illness was also strongly associated with the development of balance and speech problems and less so with the worsening of bradykinesia , and was not associated with the progression of rigidity .
A current study rigorously compared studies and found that strong evidence supports the following risk factors for freezing
The Route To Better Walking
The good news for people with PD is that with exercise and physical therapy it is possible to cope better with freezing, turn and walk more normally and improve balance. Through practice and sessions, a physical therapist can help people with PD avoid tripping by helping them learn to take larger steps. Additionally, joining an exercise class tailored to people with PD can help. If you take levodopa, be sure to exercise while it is working the drug helps your body learn and remember motor skills.
Tricks that can help overcome freezing:
- Walk to a regular beat to help prevent freezing. Try a metronome.
- Take large, voluntary marching steps.
- Step over an imaginary line or laser pointer.
- Work with a therapist to find the solution that works best for you.
People respond differently to audio, visual or sensory cues. Dr. Horak and her team are testing a device that provides sensory feedback vibration on the foot to stimulate automatic stepping.
Another consideration for people who have freezing is anxiety, a common PD symptom. People who have anxiety experience freezing more often. It is a vicious circle being anxious about freezing can trigger it. Treating anxiety may help freezing.
Read Also: How To Fight Parkinson’s Disease
Treating Freezing Of Gait For People With Parkinsons
Freezing of gait episodes often occur when a person is under-medicated and can improve with increased amounts of their PD meds, usually carbidopa/levodopa. However, as mentioned earlier, the brain abnormalities that lead to freezing of gait are very complex, so giving more dopaminergic medication is only part of the solution. In fact, some people have what is referred to as ON freezing. This means that freezing of gait episodes occur even when other PD symptoms are well treated with their medication regimen.
Cueing, or the introduction of an external sensory stimulus to facilitate movement, has been identified as a way to break a freezing episode. Terry Ellis, PhD, PT, NCS, Director of the APDA National Rehabilitation Resource Center at Boston University, and Tami DeAngelis, PT, GCS, compiled this list of cues that can be used to get out of a freezing episode:
What Freezing Is Like For My Dad
Like many Parkinsons patients, my dad notices that he usually only freezes when hes not on his medication. It usually happens while hes moving through doors: When you pivot youre worried about losing your balance. Thats why we shuffle our feet and take baby steps initially. Once Im moving Im fine, he says.
Since hes worried about maintaining balance while navigating, its possible that theres a connection between fear and freezing. Continuous motion seems to bypass the risk of freezing, while shifting motion types can present challenges.
Recommended Reading: How Do Parkinson’s Patients Die
Subthalamic Oscillatory Activity And Connectivity During Gait Freezing
To investigate the role of the STN neural activity in gait freezing we compared the STN oscillations between walking and ongoing freezing episodes. We first studied power changes in low frequency and in the -frequency band of the two STN and did not find any differences during gait freezing in comparison to walking . We also assessed the duration of -burst and did not find a difference between walking and gait freezing . We finally investigated the subthalamic interhemispheric coupling in the -band and showed an increase of -coupling followed by a reduction in the synchronization between the two STN during gait freezing. However, this change did not reach statistical significance .
What Is Dystonia And Freezing In Parkinsons Disease
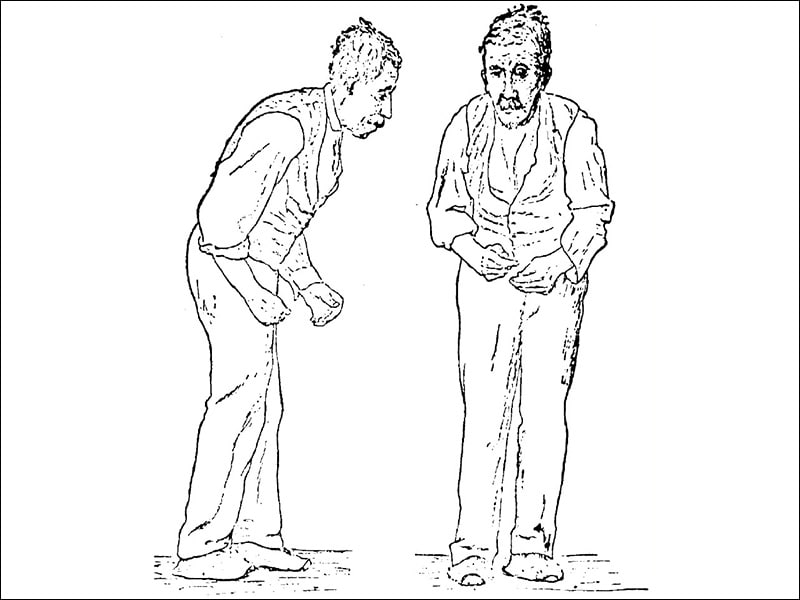
Along with motor fluctuations and dyskinesia, some people with Parkinsons disease experience problems with muscle contractions called dystonia and freezing.
Dystonia is the involuntary, continuous contractions of muscles that result in repetitive movements, such as twisting or curling of one or more body parts.
Dystonia may occur at various times, including:
- When the medication is working at its full potential
- When dopamine levels are the lowest
- When the medication has just begun to exert its effect
Freezing is the temporary and involuntary inability to move. People feel as if their feet are stuck to the ground. This can happen for several seconds to minutes. The phenomenon results from decreased levels of dopamine.
Don’t Miss: What Is Lewy Body Parkinson’s Disease
Negative Consequences Of Freezing
Freezing episodes limit the mobility of a person with PD and may contribute to reduced socialization and a lower quality of life. In addition, freezing can be dangerous and is associated with falls in people with PD. Approximately 38% of people with PD fall each year, and freezing increases the risk of falls as freezing occurs without warning. Falls can cause additional health problems, including broken bones or head injury.1,2
Other Relevant Information Pages
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category “Analytics”. |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category “Functional”. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category “Necessary”. |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category “Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category “Performance”. |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
Also Check: What Is The Best Mattress For Parkinson Patients
Noninvasive Vagus Nerve Stimulation
Recently, it has been reported that VNS administered for 10days improved locomotion in a rodent model of PD . Thus, an observational, open-label, pilot study explored the effect of single-dose, noninvasive VNS on gait pattern and FOG in 12 patients with FOG. A total of 2 VNS treatments were applied to the left vagus nerve in left side of the neck below the mandibular angle, medial to the sternocleidomastoid muscle and lateral to the larynx, with an interval of 15min between 2 VNS treatments. Each VNS treatment consisted of 120s of stimulation. Assessments were performed just before and 15min after the application of VNS. Video analysis showed that VNS significantly improved the number of steps taken while turning . The mechanism was still unknown. One possibility is that locus coeruleus noradrenergic neurons degenerate prior to substantia nigra dopaminergic neurons in PD, and VNS may activate locus coeruleus neurons . A multicenter, double-blind, placebo/sham-controlled randomized trial of noninvasive VNS in patients with PD are needed.
Summary Of Pharmacological Treatments For Fog

Continuous subcutaneous apomorphine infusion is reversible and more convenient than LCIG, but the result of one small study was disappointing. The efficiency of subcutaneous apomorphine infusion on FOG needs to be tested in future studies. It is worth noting that several studies supported that the DA increased the risk for FOG , physicians should take caution while prescribing DA for PD patients with FOG. There was lack of strong evidence that oral amantadine can improve FOG and two double-blind, randomized, placebo-controlled studies found that intravenous amantadine had no beneficial effect on FOG . L-DOPS plus entacapone were shown to be effective in improving FOG, but whether L-DOPS alone could improve FOG needed further studies . An underlying loss of cholinergic function contributes to freezing, but the recently double blind placebo-controlled study did not find FOG improvement after acetylcholinesterase inhibitor rivastigmine treatment , although a previous open label controlled study showed positive results under another acetylcholinesterase inhibitor galantamine treatment. Botulinum toxin and Atomoxetine are ineffective according to the clinical evidence.
Also Check: When Should Parkinson’s Patients Stop Driving
How Are Motor Fluctuations Treated
Motor fluctuations affect the quality of life of people with Parkinsons significantly by limiting their activities of daily living, mobility, and social interaction. The treatment aims to keep the person moving and make them carry their daily activities independently.
Doctors can use any of the following strategies to help the affected people to minimize or avoid motor fluctuations:
- Adjusting the dose of levodopa: The doctor can either increase the dose or change the number of times the drug is taken in a day.
- Introducing different medications: Adding different medications to the current medication can help maintain consistent levels of dopamine and thus, prevent off-times.
- These medications include
The 5s Method Consists Of The Following 5 Sequential Steps:
If you are a Thrive patient, be sure to ask your therapist for your 5S magnet if you dont already have one.
Recommended Reading: Does Parkinson’s Cause Dizziness
Strategies To Combat Freezing In Parkinsons Patients
Freezing is when an individual suddenly feels like theyre glued to the ground. Parkinsons disease patients often experience freezing during the late stages of the disease. It can occur while the person is in motion or after theyve been stationary and then attempt to move. Its associated with complicated movements like dodging obstacles or getting up from a chair.
The loss of automatic motor skills affects ones sense of control and even their safety, as about 38 percent of Parkinsons patients fall each year. Tracking when your struggles occur can help you to manage them, allowing you to challenge how frequently freezing occurs.
What Does Freezing Of Gait Look Like In Daily Life
If youre scratching your head about what freezing of gait means, youre not alone. In fact most health professionals need to google it.
When it comes to walking, some people living with PD experience this sense of being stuck, or my feet are stuck to the floor which describes the disrupted gait in patients living with PD.
- Freezing: These are brief or prolonged episodic phenomena of not being able able to step, or move your feet forward despite the mind being willing and having the conscious intention to walk.
- Gait: Refers to the pattern of walking.
Whatever your experience of FoG is, there are some common features of this gait pattern.
- Firstly, FoG is defined as a brief episodic absence or marked reduction of forward progression of the feet despite the intention to walk .
- Freezing of gait is a major disabling motor symptom that affects the daily quality of life of Parkinsons disease patients.
- FoG appears commonly at advanced or later stages of the disease experience: Prevalence of FoG increases with longer disease duration. It has been reported that 81% of PD patients experienced FOG after a disease duration of 20 years.
- BUT a mild form can be seen in the early stages.
- Moreover, clinical features cited are: motor dysfunction, sleepiness, fatigue, and cognitive dysfunction
- And this differs to what the patient reports such as postural instability and walking pattern difficulty.
Read Also: What Part Of The Brain Is Affected By Parkinson’s Disease
What To Do When You Freeze Or Cant Get Started
If a movement isnt flowing well, making the effort to think about each separate part of a familiar or simple movement can help you get going.
If your feet freeze you may fall over so make sure that any family, friends and carers know about your freezing and know how to help when it happens.
The first thing to do when you feel yourself freeze is to stop moving, or to slow down. This gives you time to refocus on balance, think about your next move and prepare your body to start again, which can reduce any risk of falling.
The plan method
- STOP: calm yourself and take a breath.
- THINK: what do you want to do?
- PLAN: how are you going to do it?
- DO: complete the task or movement.
The weight shift method
- When you freeze, dont try to move forward straight away. Instead, gently move most of your weight to one leg . Shifting your weight to your one supporting leg like this will let you step forward with the opposite foot. To help with this count one, two, three, step or say ready, steady, go to yourself to get moving again.
- You may be able to re-start walking again by gently rocking your head and shoulders from side to side. This rocking can help you shift your body weight to your supporting leg.
- It may help to say something to yourself as you do this, like move my weight to left leg, then step with right . You may have to rock from leg to leg to release the weight on each foot before stepping off.
Sound and vision cueing methods
Using your imagination
Floor strips
Techniques To Overcome Freezing
Physical therapy and occupational therapy can be helpful to reduce or overcome freezing episodes. Physical therapy focuses on the physical rehabilitation of people recovering from injuries or disease with the goal of restoring mobility, as well as educating patients on managing their condition to maintain long-term benefits. Occupational therapy also deals with rehabilitation and motion but is focused more on enabling the person to engage in daily activities as seamlessly as possible. Occupational therapists also suggest adaptations and modifications to the persons environment.3
There are several techniques that can help people with PD overcome freezing, including:
As with any symptom, patients who experience freezing episodes should mention this to their neurologist who is managing their care. The neurologist may make changes to medication or provide a referral to a physical or occupational therapist.
Read Also: What Is The Typical Treatment For Parkinson’s Disease
Transcranial Direct Current Stimulation
In general, anodal tDCS facilitates cortical excitability. In a crossover, double-blind, randomized, sham-controlled study including 10 PD patients with levodopa-resistant FOG, five sessions of 2mA anodal tDCS on primary motor cortex showed benefits on FOG and motor performance after tDCS . However, another crossover double-blind, randomized, sham-controlled study applied one session multibipolar tDCS electrodes stimulating only primary motor cortex in PD patients with FOG didnt improve FOG. But after stimulating both primary motor cortex and left dorsolateral prefrontal cortex, the performance in gait-provoking test, stroop, and time up and go tests were improved . Besides, another double-blinded crossover randomized, sham-controlled study including 10 PD with FOG showed a single dose of anodal tDCS over the SMAs did not improve self-initiated gait in PD and FOG .
