Diagnosis Of Rbd In Pd
The diagnosis of RBD can be based on a questionnaire or clinical manifestations without confirmation by polysomnography .Therefore, a detailed history of complex motor behaviors and vocalizations during REM sleep is very important for a clinical diagnosis of RBD. However, for the objective diagnosis of RBD, complex motor behaviors during REM sleep and the presence of REM sleep without atonia should be confirmed by PSG . Additionally, this sleep disturbance should not be better explained by another disorder . PSG can detect increased chin muscle tone by the submental EMG or increased phasic muscle activity by the limb EMG during REM sleep . Thus, PSG is not required for the clinical diagnosis of RBD . It has been reported that a total score of 6 or higher obtained from the RBD screening questionnaire used for the clinical diagnosis of RBD may strongly support the diagnosis .
Parkinsons Disease And Sleep
Reviewed by David Rye, MD, and Mark Mahowald, MD. Published by the National Sleep Foundation
This web article offers a detailed description of Parkinsons disease and the challenges it presents to restorative rest and recuperation. Some suggestions are included for improving sleep and the environment around sleeping.
How To Get Better Sleep With Parkinson’s
Although there is no cure for Parkinson’s, there is a way to live with it. In order to get better sleep, there are certain things you can do to maximize your sleep. Tips for better sleep include:
- Keeping a regular sleep schedule
- Choosing a bedtime on when you want to get up
- Make a bedtime routine
- Sleep in a cool place
- Don’t do anything in bed besides sleep and sex
- Use the bathroom before going to bed
- Use satin sheets and pajamas to make moving in bed easier
Read Also: What Is The Outcome Of Parkinson’s Disease
Good Night: Sleep And Parkinsons Disease
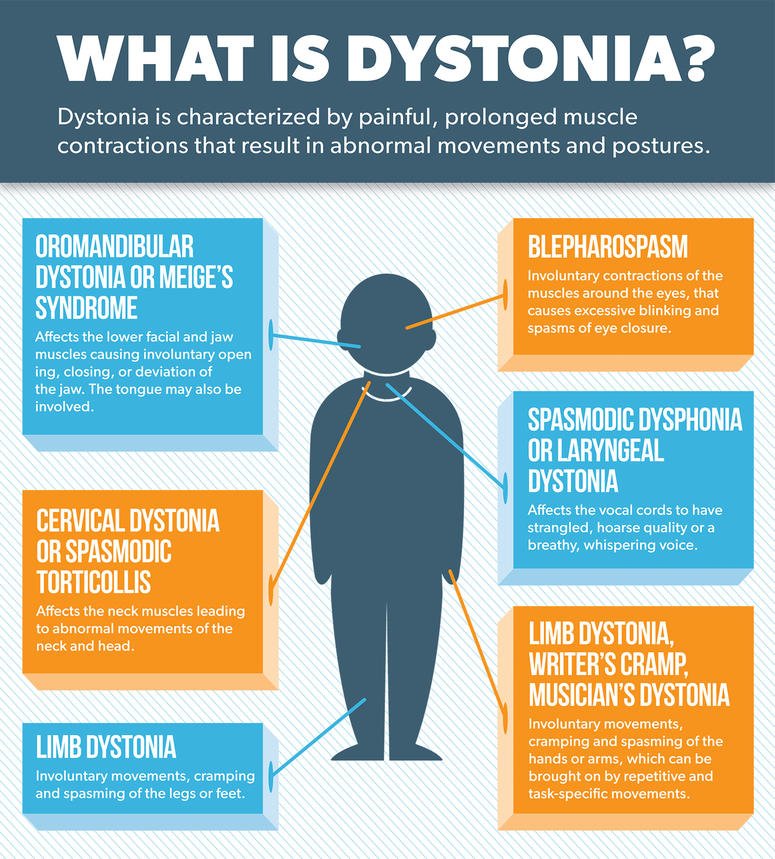
Lack of good sleep can worsen Parkinsons symptoms. In this 45-minute lecture, Dr. Rafael Zuzuárregui addresses causes of sleep loss and the latest treatments for: insomnia, restless leg syndrome, REM sleep behavior disorder, nocturnal urination, hallucinations, wearing off of medication, dystonia and sleep apnea.
Other Aspects Associated With Sleep Disruption In Pd
However, discrepancies between subjective and objective measures of sleep quality are well documented even in primary sleep disorders and might be influenced by mood disorders such as depression complicating management of sleep disorders even further . This is underlined by a study showing a close correlation between subjective sleep quality and neuropsychiatric symptoms such as anxiety with daytime functioning, while objective sleep quality assessed by actigraphy did not predict daytime functioning . It is of great importance to take sleep discrepancy into account in regard to initiating diagnostic and therapeutic measures.
Autonomic NMS, particularly in the advanced stages of PD, such as constipation, gastroesophageal reflux, and nocturia may also contribute or cause sleep fragmentation . Briefly, the management of these conditions includes behavioral and pharmacological approaches. Bladder dysfunction should be approached by establishing behavioral treatment, e.g., bladder training, restriction of fluid intake in the evenings, pelvic floor exercises, application of pads as well as introduction of specific medication such as solifenacin . In case of constipation, probiotics, macrogol, and lubiprostone are likely efficacious . In conclusion, motor symptoms as well NMS should be evaluated regarding their impact on sleep and daytime functioning and treated adequately.
Also Check: What Foods Should Be Avoided If You Have Parkinson’s Disease
Deep Brain Stimulation In The Treatment Of Sleep Disorders In Pd
Studies investigating the effect of DBS in the treatment of sleep disorders in PD patients showed that DBS improved the sleep scales and quality . Baumann-Vogel et al. found that subthalamic nucleus DBS-enhanced subjective sleep quality, reduced sleepiness measured by the Epworth sleepiness scale, and reduced sleep fragmentation shown by actigraphy recordings. However, the authors observed that subthalamic DBS was not improved REM sleep features . Similarly, Cicolin et al. reported that RBD symptoms did not benefit from STN DBS. On the other hand, Chahine et al. reported that STN DBS improved significantly symptoms of RLS in PD patients. The effect of PPN DBS on sleep disorders in PD has been investigated in several studies . One study showed that PPN DBS improved sleep quality and reduced EDS however, it caused a reduction in REM latency and a relevant increase in REM sleep . In another study, it has been reported that PPN DBS improved the total duration and rate of REM sleep . As a result, DBS seems to be beneficial in the treatment of sleep disorders in PD because it seems to be useful in improving sleep quality. However, large-scale prospective studies are needed to understand the benefits of DBS in the treatment of sleep disorders in PD.
Clinical Features Of Insomnia
Insomnia is defined as difficulties initiating sleep , sleep maintenance problem or early awakening . In studies, it has been reported that the frequency of insomnia in patients with PD varies from 27 to 80% . It has been reported that the most common types of insomnia in PD patients are sleep fragmentation , and early awakenings . It has been reported that insomnia may occur alone or accompany comorbid mental or systemic illnesses, and it is associated with disease duration and female gender . Sleep fragmentation is defined as a deterioration of sleep integrity , and it leads to a lighter sleep or wakefulness . In studies, it has been reported that sleep fragmentation is the most common sleep disorder in patients with PD .
Recommended Reading: What Area Of The Brain Does Parkinson’s Disease Affect
What Else Can I Do To Sleep Better With Parkinsons Disease
Practicing healthy sleep hygiene habits may also promote more restful sleep.
- Get outside during the day. Bright light tells your body its time to be awake.
- Keep your body moving during the day. Even if all you feel up to is a short walk or two, all physical activity offers benefits.
- Try at-home remedies, such as massage or a warm bath. Relaxing your mind may help your body fall asleep.
Dont:
- Take long naps during the day.
- Use stimulants, such as caffeine, within six hours of bedtime.
- Use your bedroom for activities other than sleeping. Go to another room to read, watch TV or work.
How Does Parkinsons Disease Cause Sleep Problems
Researchers have yet to uncover every nuance of the Parkinsons and sleep connection. So far, medical experts believe several causes may contribute:
- Chemical changes in the brain: Ongoing research shows that Parkinsons disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinsons to get less sleep.
- Medication: Some drugs that treat Parkinsons disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinsons commonly deal with mood disorders, such as anxiety or depression. Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinsons symptoms: Pain, waking up at night to pee or other Parkinsons symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Don’t Miss: Is Parkinson’s A Mental Illness
Why Is It So Hard To Sleep Now That I Have Parkinsons
Parkinsons can impact sleep in a number of ways, ranging from trouble falling or staying asleep at night to excessive sleepiness during the day. A good sleep boosts everything from your mood to your ability to think and process to your physical movement. Understanding sleep problems and Parkinsons is often the first step you can take to enhance your sleep.
In this post, we help you learn more about sleep problems in Parkinsons and how you can improve your quality of sleep.
Parkinsons can affect sleep in many different ways, including trouble falling or staying asleep, vivid dreams, waking up frequently during the night and excessive sleepiness during the day. Like other non-motor symptoms, sleep problems can appear before the more recognized motor symptoms, like tremor or stiffness.
People with Parkinsons typically experience some combination of insomnia and sleep fragmentation . Studies have shown people with Parkinsons have different sleep patterns and that their deepest periods of sleep during the night are shorter and interrupted more often than people without Parkinsons. Often this is made worse by medications that may wear off during the night, causing painful stiffness, difficulty moving in bed or other symptoms to return and disrupt sleep.
Parkinsons Symptoms Including Pain And Frequent Urination
Pain is a common cause of sleep disturbances in Parkinsons, says Horvat. A study published in June 2019 in the Journal of Pain Research found that about one-third of people with Parkinsons had clinically relevant sleep disturbances, and that central parkinsonian pain was the pain subtype that was most often associated with sleep issues.
Central pain can vary widely from person to person. It can feel like a constant burning or tingling that affects the whole body or it can be an intermittent sharp episode of pain, according to the Parkinsons Foundation.
You should definitely talk to your doctor if pain or Parkinsons symptoms are waking you up or keeping you up at night, to see what your treatment options may be, says Horvat.
Frequent urination can be a sign of several different things, and so its important to pay attention to any other symptoms you may also be having, she says.
Autonomic instability is often present in Parkinsons disease, which basically means the autonomic system is not firing regularly, as it should be, says Horvat. The autonomic system controls functions that keep you alive, including your heartbeat, breathing, and digestion.
This condition can lead to incontinence or urinary retention, she says. This is something to talk with your doctor about there are some medications that can be helpful.
You May Like: What Helps Parkinson’s Disease
Why Do Parkinsons Patients Have Trouble Sleeping
Despite having daytime tremors, Parkinsons patients do not shake in their sleep. However, both Parkinsons disease itself and the medications used to treat it can give rise to a number of sleep problems that lead to insomnia and excessive daytime sleepiness.
Patients with motor symptoms may have trouble adjusting sleeping positions to get comfortable. Others may experience distressing nocturnal hallucinations when trying to fall asleep. These may be a result of medications or cognitive impairment.
In turn, excessive daytime sleepiness may occur as a consequence of sleeping poorly at night. It may also be triggered by medications. Parkinsons patients who suffer from EDS may be at a higher risk of accidents and unable to safely carry out activities such as operating a motor vehicle.
Since insomnia frequently goes hand-in-hand with anxiety and depression, it may be a contributing factor to sleep problems in people with Parkinsons disease. For that reason, doctors often look for mental health disorders in people with Parkinsons disease who have sleep problems.
Parkinsons Disease Sleep Disorders: Treatment And Tips
If youre experiencing sleep problems in Parkinsons disease, your doctor may suggest changing or altering your medication. Some medications act as stimulants and can keep you awake. Others may wear off at night and cause a worsening of PD symptoms. If this happens, your doctor may suggest switching you to a drug thats delivered to your body continuously, such as skin patches or levodopa infusions.
If changing your medication doesnt help, you may be referred to a specialized sleep clinic. You may also need certain breathing equipment during the night if your sleep apnea is severe.
There is plenty you can do to improve your sleep health. Here are some tips to overcoming sleep disturbances in Parkinsons disease:
- Dont drink water for a couple of hours before bed
- Create a relaxing night-time routine that doesnt involve talking about heavy topics before sleep, watching TV or eating a heavy meal before you lie down
- Enjoy a warm bath in the evening before you go to bed
- Do something relaxing before sleep, such as reading or listening to an audiobook
- Get plenty of fresh air and exercise throughout the day, though you should avoid activity at least 2 hours before bed
- If possible, make sure your bedroom temperature is between 60-65 degrees Fahrenheit
- Reduce noise and light in the bedroom
You May Like: What Is The Medicine For Parkinson’s Disease
Sleep Related Movement Disorders
Restless legs syndrome
Clinical presentation and pathophysiology RLS, also known as Willis-Ekbom-Syndrome, is defined by unpleasant sensations, usually of the legs, but sometimes also arms or other body parts, with an uncontrollable urge to move. Symptoms occur primarily at rest in a circadian pattern, preferably in the evenings or at nighttime, and are at least temporarily relieved by movements as defined by the International Restless legs study group criteria . The estimated prevalence of RLS varies widely depending on the selected study population between 1% and 24% . Whether the prevalence of RLS is elevated in PD compared to the general population still needs to be finally determined . However, current evidence suggests a similar prevalence of RLS in de novo PD patients compared to the general population with increasing numbers associated with dopaminergic treatment and disease progression as well as age and female sex . However, other symptoms such as akinesia, NMS, and limb motor restlessness resulting in unspecific distress and unpleasant feelings at nighttime, but not fulfilling the strict criteria for RLS, might be confused with RLS, thus leading to overestimation of RLS prevalence in PD .
Diagnostic workup
Therapeutic options
Nighttime Trips To The Bathroom
Waking up frequently during the night to use the toilet is called nocturia and is common among people with Parkinsons. These interruptions in the sleep cycle can have a significant impact on your overall quality of sleep.
If you find yourself getting up more than once during the night to use the toilet, discuss with your doctor to see if there are certain medications that might be helpful. Sometimes this can be corrected by working with an incontinence specialist . Limiting the amount of liquid you drink a couple of hours before bed may help with nocturia as well.
Don’t Miss: How Quickly Does Parkinson’s Progress
Conflict Of Interest Statement
GL received honoraria for participation in clinical trial as sub-investigator from UCB Pharma PC received honoraria for speaking engagements or consulting activities from Allergan Italia, Lundbeck Italy, UCB Pharma S.p.A, Chiesi Farmaceutici, AbbVie srl, Eli Lilly and Company, Zambon FP received honoraria for speaking engagements or consulting activities from Sanofi and Bial. The other authors declare no conflict of interest.
Insomnia And Parkinsons Disease
Parkinsons disease comes with its fair share of challenges. Among the most frustrating symptoms of Parkinsons is insomnia, or difficulty sleeping. Research has found that the majority of people with PD experience trouble sleeping, and more than 3,000 members of MyParkinsonsTeam report difficulty sleeping as a symptom. Lack of regular sleep can have tremendous impacts on a persons quality of life. In fact, dealing with a sleep deficit can cause anyone to experience problems with memory and thinking.
Good, restful sleep is vital for people with Parkinsons, but it isnt always easy to get quality sleep. Luckily, there are some ways you can work toward combating insomnia with Parkinsons.
Read Also: Fibromyalgia And Parkinson’s Disease
Everyday Life And Quality Of Life
Insomnia can have serious effects on a persons quality of life. One MyParkinsonsTeam member shared their experience with insomnia. I usually sleep for four hours, wake up, toss in bed for an hour, and sleep for two, usually maxing out at six total, they wrote. Im a mess the next day after 1 p.m. or so. I dont know what PD fatigue is like compared to sleepless fatigue because I cant tell which I am affected by. Likewise, I dont know what my new normal is because I seem to always be tired.
Another member reported having a similar experience. If I do get sleep, its only for a few hours, and then Im up for the rest of the day, they posted. They continued, and wrote their insomnia even affected their ability to hold their job. I had to stop work a few years ago, and that is tough, they shared.
Insomnia can also affect more than just the person with PD. Caregivers, family members, and bed partners can all suffer from the effects of insomnia and related sleep dysfunction. Treating this problem is important not just for you but also for your loved ones.
Drugs Used To Treat Parkinsons Disease
The common Parkinsons disease medication of carbidopa and levodopa can contribute to insomnia for some people, says Horvat. Thats because its replacing the dopamine that youve lost in Parkinsons disease, she says. Research has shown that dopamine receptors play a role in wakefulness.
Sometimes when people are first started on this medication, they will take a dose right before bed rather than closer to their dinner, says Horvat. Then theyre not able to get to sleep because the dopamine affects the reward center in the brain and gives people a high, she says.
Besides timing the medication further from bedtime, your doctor may suggest taking an extended-release capsule of carbidopa and levodopa, says Horvat. That has a lower peak dose effect, so the stimulation is milder, and it lasts a little longer. It can allow patients to have more of a baseline rather than a peak at night, which can cause the insomnia, she says.
If you suspect your medication is making sleep difficult, tell your doctor dont stop taking the medicine as prescribed, says Horvat. Sometimes we can time the medication in a different way or in some cases we do change the medication but this is not something to try to figure out on your own.
Don’t Miss: What Causes Parkinson’s Dementia
