Identifying Potential Best Practices For Treating Parkinson’s: A Mixed Methods Approach
Researchers used Parkinsons Outcomes Project data to better identify specific care approaches associated with better outcomes across patients who seek expert care at a Center of Excellence. Best practices included:
- Early referral to physical therapy
- Encouragement of exercise as part of treatment
- Availability of a psychiatrist on the team
- Communication with patients in between visits
- Focus on early patient and caregiver education
The study concluded that patients at some centers see superior outcomes. Studying these centers, the foundation can test best practices and turn them into evidence-based care recommendations that can help the entire PD health professional community, making life better for people with Parkinsons.
In 2015, the Parkinsons Foundation shared these findings at the American Academy of Neurology and presented them at the 2015 International Parkinson and Movement Disorders Society Congress.
Stage Four Of Parkinsons Disease
In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them.
At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as stage three.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Recommended Reading: Does Parkinson’s Cause Memory Issues
Effectiveness Of Multidisciplinary Interventions For The Axial Symptoms Associated With Pd
Currently, while there are high-quality research programs studying the pharmacological treatment of the different axial symptoms in PD, there continues to be a lack of evidence on the efficacy of multidisciplinary interventions . Axial symptoms respond poorly to dopamine replacement therapy, and their satisfactory symptomatic control remains challenging . Given their notable clinical importancereduced mobility, loss of independence, recurrent falls, and subsequent injuriesnew methodologies need to be explored .
Although this was not a trial intended to study efficacy and we cannot make conclusions on this topic, a medium to large effect size was found on more than one measure, and patients and health professionals perceived a benefit. We believe that our data provide information about and reinforce the importance of exploring this potentially interesting path for improving the management of axial symptoms in PD. Our results are supported by a 2005 study on the efficacy of a multidisciplinary treatment program on PD patients’ long-term outcomes. The authors reported the positive effects of a multidisciplinary approach in improving and maintaining PD patients’ axial motor symptoms.
Regular Exercise Is Associated With Better Quality Of Life And Mobility In People With Pd
This study examined the associations between exercise and change in quality of life and mobility over two years. The study compared those who exercise and those who did not. Improved mobility and a better quality of life were seen in those who:
- Consistently exercised
- Started exercising after their first center visit
Presented at the International Parkinson and Movement Disorders Society Congress in 2016.
You May Like: What Is Wolf Parkinson’s White
What Is Parkinson’s Disease
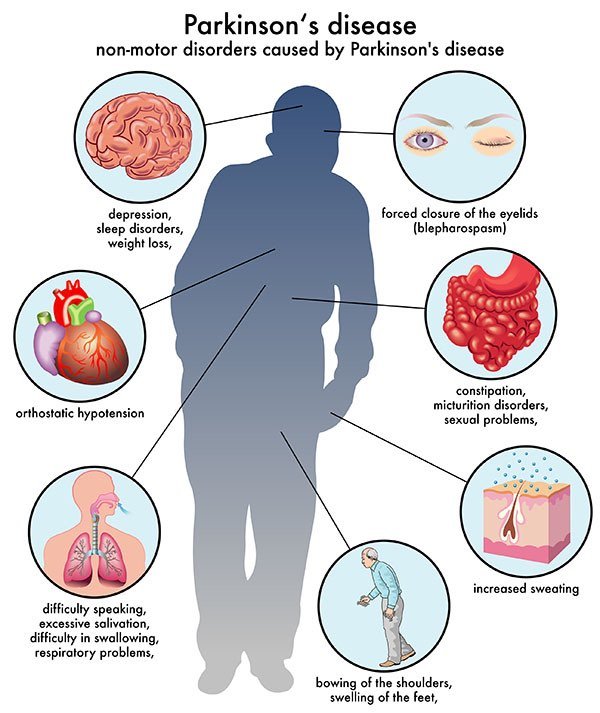
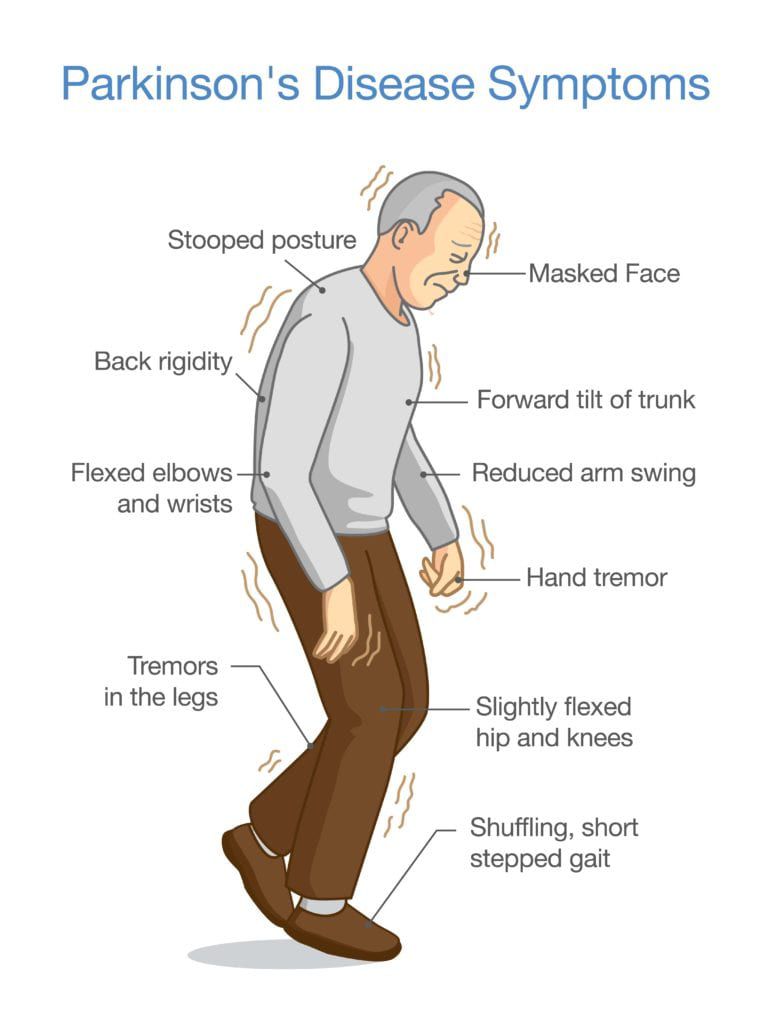
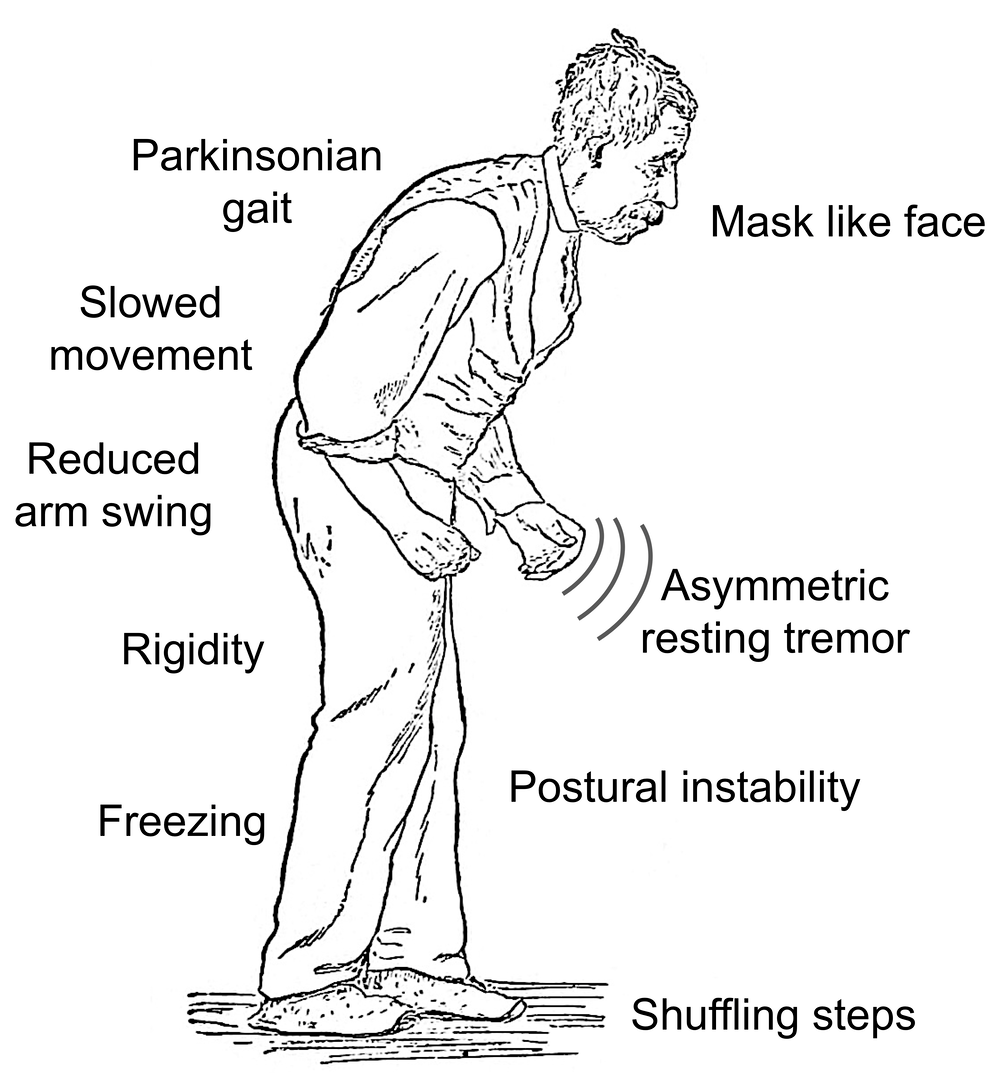
Parkinson’s disease is the second most common neurodegenerative disorder and the most common movement disorder. Characteristics of Parkinsons disease are progressive loss of muscle control, which leads to trembling of the limbs and head while at rest, stiffness, slowness, and impaired balance. As symptoms worsen, it may become difficult to walk, talk, and complete simple tasks.
The progression of Parkinson’s disease and the degree of impairment vary from person to person. Many people with Parkinson’s disease live long productive lives, whereas others become disabled much more quickly. Complications of Parkinsons such as falling-related injuries or pneumonia. However, studies of patent populations with and without Parkinsons Disease suggest the life expectancy for people with the disease is about the same as the general population.
Most people who develop Parkinson’s disease are 60 years of age or older. Since overall life expectancy is rising, the number of individuals with Parkinson’s disease will increase in the future. Adult-onset Parkinson’s disease is most common, but early-onset Parkinson’s disease , and juvenile-onset Parkinson’s disease can occur.
Injury Rates For People With Pd Predicted By Parkinsons Severity
This study researched falls among people with PD. The study proved that the rate of injury increases with Parkinsons severity independently of a persons age or PD stage. The study showed that those with the highest fall risk are men with rapid rate of progression and a comorbidity .
Presented at the World Parkinsons Congress in 2016.
Also Check: Does Senator Susan Collins Have Parkinsons
What Are The Symptoms Of End
Stage four for Parkinsons disease is often called advanced Parkinsons disease because people in this stage experience severe and incapacitating symptoms. This is when medication doesnt help as much and serious disabilities set in.
Theres an increased severity in:
- How you speak a softer voice that trails off.
- Falling and trouble with balance and coordination.
- Freezing a sudden, but temporary inability to move, when you start to walk or change direction.
- Moving without assistance or a wheelchair.
- Other symptoms such as constipation, depression, loss of smell, low blood pressure when going to stand up, pain, and sleep issues.
Many times someone with advanced PD cant live on their own and needs help with daily tasks.
Stage five is the final stage of Parkinsons, and assistance will be needed in all areas of daily life as motor skills are seriously impaired. You may:
- Experience stiffness in your legs. It may make it impossible to walk or stand without help.
- Need a wheelchair at all times or are bedridden.
- Need round-the-clock nursing care for all activities.
- Experience hallucinations and delusions.
As Parkinsons disease progresses into these advanced stages, its symptoms can often become increasingly difficult to manage. Whether you or your loved one with end-stage Parkinsons lives at home, in an assisted living facility or a nursing home, hospice services can optimize your quality of life and that of your family members as well.
Drugs To Treat Parkinsons Disease
Study conducted by medical researchers have compared two drugs named Levodopa and Pramipexole, which is employed generally as the first treatment line associated with the parkinsons disease problem. These drugs use various mechanisms to counteract with declining in the dopamine production in human brain, which is a result of progressive cell loss to secrete neuro chemicals in human brain. Levodopa is a type of amino acid, which human body metabolizes to form dopamine. On the other side, Pramipexole is a type of dopamine agonist, which binds with dopamine receptors present on cells in human brain and mimics the molecular function associated with the chemical.
Also Read:
Don’t Miss: How Much Mucuna Pruriens To Take For Parkinson’s
Functional Mobility In Pd: Icf
In order to improve patients global health status and reduce disease burden associated with functional immobility, it is important to understand a patients personal needs, activity and environment . In this section, we present the three levels of human functioning included in the ICF framework: 1) the impairments to body structures and functions relevant to PD patients functional mobility 2) how the activities that compose functional mobility are compromised by these impairments, in a functional perspective 3) participation restrictions that PD patients may encountered, induced by functional mobility limitations 4) lastly, some examples of frequent personal and environmental factors that influence the first three domains are presented .
Human domains and contextual factors contribution to PD functional mobility.
Medication For Parkinsons Disease
Although there is currently no treatment that can slow or stop the progression of Parkinson’s disease, medication can help you manage the symptoms of Parkinsons disease. Medicines prescribed for Parkinson’s patients include:
- Carbidopa-levodopa : Levodopa is a drug that converts natural chemicals into dopamine in your brain. Carbidopa prevents the early conversion of these chemicals outside your brain, which is why it is combined with levodopa. Carbidopa also helps control the side-effects of levodopa, such as nausea and light-headedness. This medication can also be administered intravenously for patients with advanced Parkinson’s disease.
- Dopamine agonists: Instead of converting natural chemicals into dopamine, dopamine agonists mimic dopamine cells in your brain. Side-effects of this medication include compulsive behavior, sleepiness and hallucinations.
- Amantadine: This medicine can be prescribed as short-term Parkinson’s disease treatment to help ease symptoms in the early stages. It is often given alongside carbidopa-levodopa. Amantadine is also prescribed in the later stages of Parkinson’s disease to help control involuntary movements. Some patients report side effects such as mottling of the skin, swollen ankles and hallucinations.
Other medications for Parkinsons disease include MAO B inhibitors, catechol O-methyltransferase inhibitors and anticholinergics. Your doctor will explain all of these medications to you and help you decide on the best treatment option.
You May Like: How To Use Hemp Oil For Parkinson’s
Functional Mobility: Scales And Tools Available
Functional mobility is a global disease-related feature that may provide adequate information about treatment responses and disease course, as it may encompasses one of the outcomes most relevant to patients daily lives .
Due to the heterogeneity and complexity of PD, its fluctuating nature and unpredictable medication response in advanced disease stages, clinical assessment is challenging and requires continuous prolonged periods of evaluation to reach an accurate picture of symptoms and their fluctuations .
The majority of PD studies that have measured functional mobility used rating scales like the MDS-UPDRS, infrequent events or subjective reports . Objective assessments, including the five-time sit-to-stand test and the timed up-and-go test, are two of the most commonly used tools . In 2015, Parashos and colleagues validated the Ambulatory Capacity Measure. This is a measure of functional capacity, previous used in clinical trials, derived from UPDRS items related to falls, freezing, walking, gait and postural instability. It showed to be a good instrument, highly correlated with some of the most used outcome tool to assess functional capacity . However, there is still no consensus about which screening tools are preferred or which outcomes are most suitable for monitoring functional mobility .
Tango Versus Mixed Dances
There were no significant differences between groups in all outcomes estimates under this comparison, including Timed Up and Go Test, Functional Gait Assessment, Freezing Gait Questionnaire, Berg Balance Scale, disease severity , and quality of life . The certainty of evidence is low for all outcomes included in this comparison, due to serious concerns on the risk-of-bias of the included study and imprecision .
Read Also: What Are Early Warning Signs Of Parkinson’s Disease
Thanks For Signing Up
We are proud to have you as a part of our community. To ensure you receive the latest Parkinsons news, research updates and more, please check your email for a message from us. If you do not see our email, it may be in your spam folder. Just mark as not spam and you should receive our emails as expected.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
Also Check: How Long Does End Stage Parkinson’s Last
Gender Affects Caregiver Support
For the study, the foundation analyzed data on more than 7,000 men and women receiving care across our Center of Excellence network. They looked at whether patients were accompanied by a caregiver for a doctors visit and at the relationship between caregiver and patient. Study findings include:
- Compared with women, men were significantly more likely to have a regular care partner , and less likely to have a paid caregiver when they first enrolled in the study .
- Women were 26 percent less likely to have a caregiver accompany them to a regular doctors visit. And women were using a paid caregiver at a faster rate than men, which is significant because research suggests that health-related quality of life declines when a family caregiver is replaced by a paid caregiver.
Caregiving is harder on women than men , even after adjusting for potential confounders.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
Will Parkinsons Disease Treatment Affect My Prognosis
While no treatment will affect your Parkinson’s disease prognosis, many patients find that a combination of medication, physical therapy and positive lifestyle changes help them control the symptoms of Parkinson’s even in the late stages of the disease.
If you have any questions about your diagnosis or you’re concerned about your treatment options, talk to your doctor. You can also seek advice and support from the National Parkinsons Foundation Helpline by calling 1-800-4PD-INFO .
Read Also: Is Parkinsons Fatal
Home Remedies And Lifestyle Changes
In addition to exercising and taking medication, your doctor may suggest you adjust your lifestyle to help you control your symptoms, Positive lifestyle changes include healthy eating, drinking plenty of fluids and attending Parkinsons support groups. You may also want to research home remedies such as massage, tai chi and yoga all of which can be helpful to those with Parkinson’s disease.
Surgical Intervention: Deep Brain Stimulation
Surgery is sometimes offered to patients in the late stages of Parkinsons disease, or to those who dont respond well to Parkinsons medication. The procedure is called deep brain stimulation , and it involves surgeons implanting electrodes into parts of your brain and connecting them to a generator in your chest. The electrodes then send signals to your brain to help it coordinate movement.
Surgery won’t stop your Parkinson’s from progressing, but it can help you control the symptoms. However, DBS also comes with an increased risk of strokes, infections and brain hemorrhaging, which is why it is usually offered as a last resort .
Also Check: Does Parkinson’s Cause Memory Issues
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
Physical Therapy And Exercise
Doctors usually recommend exercise to Parkinsons patients as it helps improve muscle strength, balance and flexibility. Your doctor may also refer you to a physical therapist. You might also decide to try swimming, stretching or dancing. Not only do these activities have physical health benefits, but they can also help ward off depression and anxiety in Parkinsons patients. Physical activities like gardening also provide therapeutic benefits.
Also Check: Parkinson’s Disease Awareness Ribbon Color
How Is Parkinsons Disease Treated
There is no cure for Parkinsons disease. However, medications and other treatments can help relieve some of your symptoms. Exercise can help your Parkinsons symptoms significantly. In addition, physical therapy, occupational therapy and speech-language therapy can help with walking and balance problems, eating and swallowing challenges and speech problems. Surgery is an option for some patients.
