Diagnosis: Parkinsons Dementia Or Dementia With Lewy Bodies
During assessment, a specialist may look at when the dementia symptoms first appeared before reaching a diagnosis of Parkinsons dementia or dementia with Lewy bodies.
If there have been motor symptoms for at least one year before dementia symptoms occur, specialists will often give a diagnosis of Parkinsons dementia.
If dementia symptoms occur before or at the same time as motor symptoms, specialists will usually give a diagnosis of dementia with Lewy bodies.
However, it should be noted that in some cases of dementia with Lewy bodies, no motor symptoms develop at all.
Theres no single test diagnosis is made through several different assessments, usually starting with an appointment with your GP or Parkinsons nurse.
Some people find it helps to go to the appointment with someone who knows them well, who can give the GP or Parkinsons nurse information about changes theyve noticed.
Your GP can discuss your symptoms with you and carry out a physical examination, including blood and urine tests, to rule out other potential causes of the symptoms .
Your GP may also review your medication, in case your symptoms are side effects.
If your GP thinks you have dementia, they can refer you to a specialist, such as a neurologist, psychiatrist or geriatrician.
You might be referred to a memory clinic or memory service. In some areas of the country, you can refer yourself to these services.
But if you feel you need to see the specialist again, you can ask to be referred back.
Diagnosis Of Parkinsons Disease
There are currently no blood or laboratory tests to diagnose non-genetic cases of Parkinsons. Doctors usually diagnose the disease by taking a persons medical history and performing a neurological examination. If symptoms improve after starting to take medication, its another indicator that the person has Parkinsons.
A number of disorders can cause symptoms similar to those of Parkinsons disease. People with Parkinsons-like symptoms that result from other causes, such as multiple system atrophy and dementia with Lewy bodies, are sometimes said to have parkinsonism. While these disorders initially may be misdiagnosed as Parkinsons, certain medical tests, as well as response to drug treatment, may help to better evaluate the cause. Many other diseases have similar features but require different treatments, so it is important to get an accurate diagnosis as soon as possible.
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
Also Check: Hypothyroidism Misdiagnosed As Parkinsons
Also Check: Exercise For Parkinson’s Disease Video
Alzheimers And Parkinsons Disease: Similarities And Differences
James M. Ellison, MD, MPH
Swank Center for Memory Care and Geriatric Consultation, ChristianaCare Configure
Explore the similarities and differences between two common degenerative brain disorders.
Ron brings his 78-year-old wife, Sara, to the Memory Clinic, with a pressing concern. Sara is forgetting things more often even though her Parkinsons disease symptoms appear to be under good control with standard medications, healthy diet, and plenty of physical activity. She is losing her train of thought mid-sentence and she became very confused about where she was while driving the well-traveled route to her daughters home. Is she developing dementia? Is that a part of Parkinsons disease? Or is she developing Alzheimers disease? And what are the differences between Alzheimers and Parkinsons?
What Causes Lewy Body Dementia
The causes of LBD are not yet well understood, but research is ongoing in this area. There are probably multiple factors involved, including genetic and environmental risk factors that combine with natural aging processes to make someone susceptible to LBD.
For more information, visit www.lbda.org.
Modified with permission from the Lewy Body Dementia Association
To learn more about motor symptoms related to Parkinsons, visit here.
To learn more about non-motor symptoms related to Parkinsons, visit here.
You May Like: Parkinson Foundation Of The National Capital Area
You May Like: How To Stop Dyskinesia In Parkinson’s
Do Treatments Add Time To Life Expectancy
Experts simply dont know whether treatments help a person live longer with Alzheimers disease. AD and other similar dementias progress no matter what. Treatments like medications and therapies have been conclusively shown to help manage symptoms, meaning they make it easier to live with the disease, but they do not reverse symptoms. The memory of a person with dementia who takes medications like cholinesterase inhibitors, for example, will be slightly better than the memory of someone who is not on medication. Quality of life therefore improves with treatment. This means better years with dementia, but probably not more years.
Pd Dementia And Safety Concerns
Safety issues should be considered and monitored from the time of diagnosis. As PDD progresses, ensure that your loved one is not left alone and try to:
- Evaluate driving privileges before safety is a concern. Your doctor can make a driving evaluation referral.
- Work out legal and financial issues and safeguard finances. People with dementia are at greater risk of falling victim to scams and fraud.
- Minimize prescription risks. Confirm with the doctor the medication names and doses of the person with PD. If the person is in dementias early stages and capable, fill up their weekly pill box together and monitor use.
- Look into medical alert systems. These systems can be critical in the event of a fall or if your loved one wanders outside of the home. Many types of systems are available, from bracelets and pendants to smartwatches with fall detection and one-button connections to 911.
- Evaluate gun safety. If your loved one owns a firearm or has one in the home, consider bringing it up with their doctor and taking additional safety precautions.
Don’t Miss: Does Parkinson’s Cause Tremors
What To Know About Taking These Drugs
The medications work by blocking acetylcholine, a chemical that helps relax and contract your muscles.
When this chemical is blocked, peoples memory and attention can become impaired which is the reason so many people complain of acute confusion and memory loss while taking these medications.
Its thought that over time anticholinergics can inhibit these cognitive functions and eventually make certain people more vulnerable to the type of degeneration that occurs in dementia.
Long-term blockage of the transmitter may lead to an acceleration of memory loss or even potentially degeneration of these types of cells in the brain, Dr. David Merrill, a neurologist and geriatric psychiatrist at Providence Saint Johns Health Center in Santa Monica, told Healthline.
Still, more research is needed to better understand exactly why anticholinergic drugs may increase peoples risk of dementia.
While there may be other factors at play, the researchers suspect that anticholinergics may cause about 10 percent of all new dementia cases.
If youre on any anticholinergics drugs, you may want to check in with your doctors about these risks, health experts warn.
What Happens In Pdd
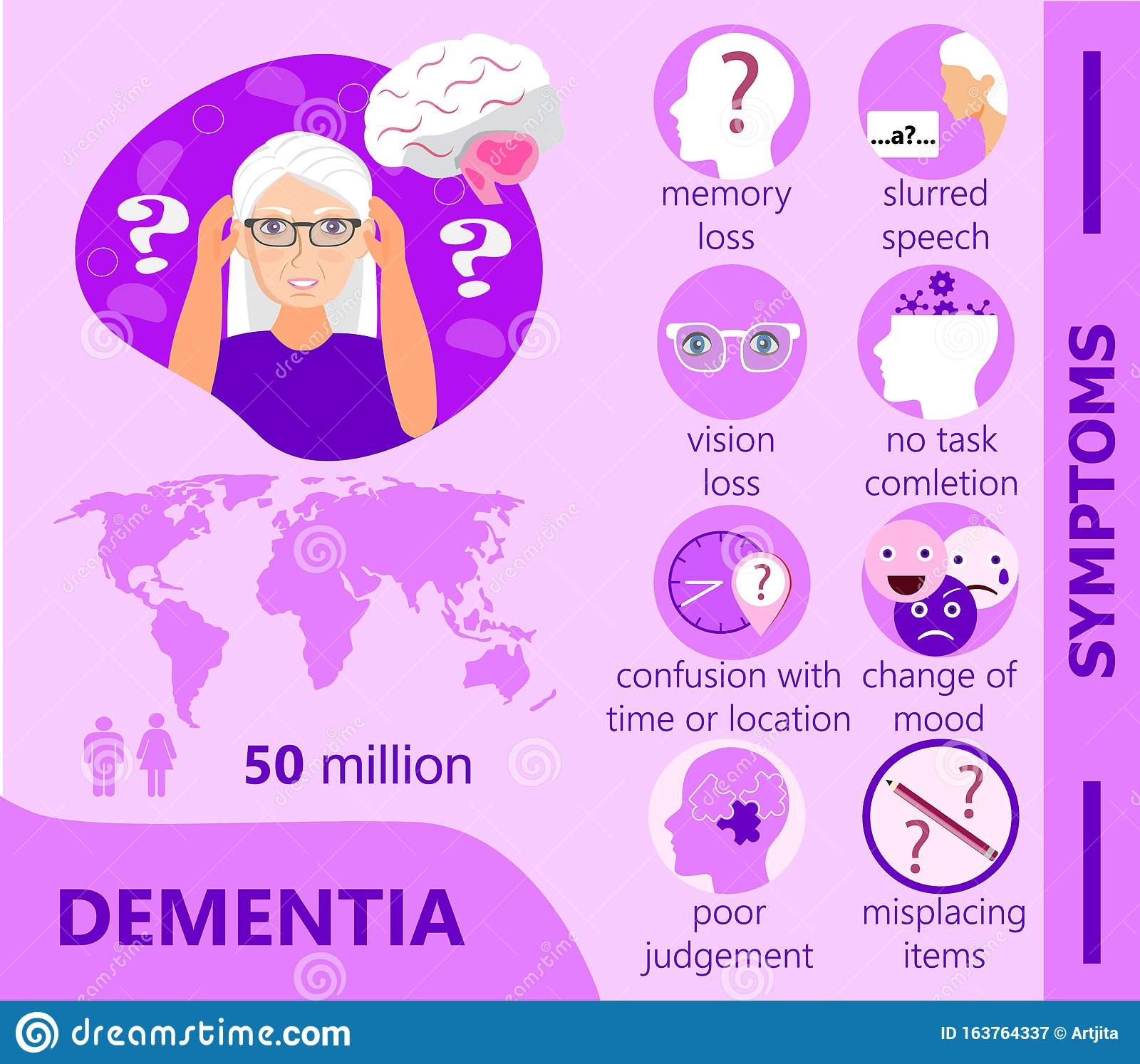
People with PDD may have trouble focusing, remembering things or making sound judgments. They may develop depression, anxiety or irritability. They may also hallucinate and see people, objects or animals that are not there. Sleep disturbances are common in PDD and can include difficulties with sleep/wake cycle or REM behavior disorder, which involves acting out dreams.
PDD is a disease that changes with time. A person with PDD can live many years with the disease. Research suggests that a person with PDD may live an average of 57 years with the disease, although this can vary from person to person.
Also Check: Is Neuropathy A Sign Of Parkinson’s
Alzheimers Vs Parkinsons Disease Dementia
The dementia of Parkinsons disease has some similarities to the dementia of Alzheimers disease. And there are some differences, too. Alzheimers disease causes dementia slowly over time, while the dementia of Parkinsons disease often develops more quickly and dramatically.
The symptoms of Parkinsons dementia can come and go from day to day, while the symptoms of Alzheimers dementia will not go away.
Protein Mutation That Causes Parkinson’s May Prevent Another Neurodegenerative Disease
by University of Massachusetts Amherst
A University of Massachusetts Amherst scientist has discovered that a mutation in the misfolding protein that causes Parkinson’s disease offers protection against another fatal neurodegenerative disordermultiple system atrophy , which is caused by the same misfolding protein.
The research findings, published today, Dec. 1, in PLOS Pathogens, move lead author Amanda Woerman one step closer toward her goal of using a personalized medicine approach to help people suffering from one of these devastating, difficult-to-diagnose diseases, for which fewif anyeffective treatments currently exist.
“This lays the groundwork for our gene therapy strategy,” says Woerman, assistant professor of biology in the UMass Amherst College of Natural Sciences. “Our results tell us that a single change in the genome can have a protective effect against MSA.”
Woerman has not previously seen a genetic mutation with this “interesting dichotomyit’s protective against one disorder and causative of another.”
The Woerman Lab is focused on studying the misfolding and aggregation of alpha-synuclein and several other proteins. The researchers work under the prion hypothesisthat a misfolded protein propagates throughout the body to cause neurodegenerative diseases, including Alzheimer’s, progressive supranuclear palsy and dementia with Lewy bodies , in addition to Parkinson’s and MSA.
More information:PLOS Pathogens
Also Check: Parkinson’s Leg Pain Treatment
How Can We Manage Hallucinations
It may not be necessary to treat all hallucinations of a person with PDD. Hallucinations are often harmless, and it is okay to allow them to happen, as long as they are not disruptive or upsetting to the person or surroundings. Sometimes, recognizing the hallucination and then switching the topic might be an efficient way of handling frustrations that occur because of a hallucination. If hallucinations need medical treatment, your provider may be able to discuss and suggest some options. However, many of the medications used to treat hallucinations may make movement symptoms worse.
Ad Patients Are At Higher Risk Of Covid
Although our results show that patients with AD, PD and vascular dementia are at increased risk of contracting COVID-19, it remains unclear whether the presence of neurodegenerative disorders may exacerbate the risk of mortality in COVID-19 patients. To address this issue, we examined the characteristics and outcomes of all COVID-19 patients in the cohort using a binary multivariable regression model . In terms of neurodegenerative diseases, a diagnosis of frontotemporal dementia was associated with the largest risk of COVID-19 death, but this observation suffers from a small sample size , so we did not explore frontotemporal dementia further in our analysis. We observed that diagnoses of AD were associated with COVID-19 death but not diagnoses of PD or vascular dementia. In our model, a pre-existing diagnosis of cancer was negatively associated with COVID-19 death , and no significant association was found with diabetes, C-reactive protein levels or ethnicity and COVID-19 death . We also found that a higher TSDI increased the risk of COVID-19 adverse outcomes , while an increased waist-to-hip ratio or male sex were positively associated with COVID-19 death, but this relationship did not reach statistical significance.
Also Check: What’s The Difference Between Alzheimer’s And Parkinson’s
What Is Parkinson Disease
Parkinson disease is a movement disorder. It can cause the muscles to tighten and become rigid This makes it hard to walk and do other daily activities. People with Parkinsons disease also have tremors and may develop cognitive problems, including memory loss and dementia.
Parkinson disease is most common in people who are older than 50. The average age at which it occurs is 60. But some younger people may also get Parkinson disease. When it affects someone younger than age 50, it’s called early-onset Parkinson disease. You may be more likely to get early-onset Parkinson disease if someone in your family has it. The older you are, the greater your risk of developing Parkinson disease. It’s also much more common in men than in women.
Parkinson disease is a chronic and progressive disease. It doesn’t go away and continues to get worse over time.
Advances In Alzheimers Therapy
Recent studies indicating that therappeutic drugs and gene therapy are advanced techniques to control alzheimers diseaseGenomics therapy is most recent advances in AD research, when the disease was first described. Researchers are looking for new therapy treatments for dementia. Currently, there is no cure for Alzheimers But these alzheimers products may show a good results to cure memory loss.
Related Journals of Advances in Alzheimers Therapy
Journal of Dementia & Mental health, Rehabilitation in Movement Disorders, Stress Alzheimers, Neuron, American Journal of Occupational Therapy, Journal of Alzheimers & Dementia, Journal of the Alzheimers Association, Journal of Alzheimers Disease, Alzheimers Research & Therapy, Journal of Alzheimers Disease and Other Dementias, International journal of Alzheimers Disease & associated disorders, International Journal of Alzheimers Disease, Advances in Alzheimers Disease, American Journal of Alzheimers Disease, Current Alzheimer Research.
Also Check: Does Michael J Fox Have Parkinson’s Disease
How Is Parkinson Disease Diagnosed
Parkinson disease can be hard to diagnose. No single test can identify it. Parkinson can be easily mistaken for another health condition. A healthcare provider will usually take a medical history, including a family history to find out if anyone else in your family has Parkinson’s disease. He or she will also do a neurological exam. Sometimes, an MRI or CT scan, or some other imaging scan of the brain can identify other problems or rule out other diseases.
Causes Of Parkinsons Disease With Dementia
Experts do not know what causes Parkinsons disease. Genetic and environmental factors may play a role. Someone who has family members with the disease is slightly more likely to develop Parkinsons. It has also been linked with exposure to pesticides and to head injuries. There is some evidence that having never smoked or drank caffeinated beverages like coffee and tea actually increases a persons chance of developing Parkinsons.
Between 50 and 80 percent of people with Parkinsons Disease will develop dementia because of the spreading deterioration of brain cells over time. Motor skills and movement are affected first causing shaking, rigidity, and slowness but after enough time the brains structure changes to the point where problem solving and memory become affected.
Risk factors for someone who has Parkinsons to develop PDD are: Old age Gender Long duration of Parkinsons Family history of dementia Hallucinations before other dementia symptoms Movement problems that are beyond typical for Parkinsons
How PDD Compares to Dementia with Lewy Bodies
How PDD Compares to Alzheimers Disease
You May Like: Is Parkinson’s Disease Rare
Parkinsons Disease Dementia And Life Expectancy
Okay so I googled this today with a mixture of guilt and curiosity. In watching Anthonys physical and mental abilities diminish over the last year, I have become increasingly concerned that he will become very depressed his confusion will cause him anxiety and he will suffer physical pain.
Some of these things are already happening of course but, so far, he is not in physical pain and remarkably, in my opinion, is not depressed in any clinical sense. He is plagued by bouts of immobility and incontinence but we have both accepted these aspects of PD. Recently, however, the confusion of dementia has caused us both anxiety. For example, if he is home for the day, he will often talk to Ming and me even when we arent in the room. And sometimes, in the nursing home, he will think we are all home on the farm, and cant understand where Ming and I are going when we leave him.
It is over seven years now since Antonys PD diagnosis, and just over two years since he has lived in the nursing home. He is sad a lot of the time, mainly because he misses me, Ming and home, but mostly he is resigned and heroic in the way he has accepted now that he is too heavy for a single person to lift
My grief and love for Anthony are in equal proportions and every single day its as if they draw straws to see which one will win usually love, but not always.
Parkinsons Disease: Symptoms Stages And Treatment
Parkinson’s disease usually begins after age 60, gradually progressing over the years. Some people can have early-onset Parkinson’s disease, starting in their 30s or 40s. It is primarily a movement disorder characterized by resting tremors and slowness and stiffness of movement.
In the late stages of the disease, Parkinson’s dementia can develop. But most people who have Parkinson’s disease do not develop dementia as a part of the condition.
Read Also: Parkinson’s Dbs Surgery Video
Changes In Cognition And Parkinsons Disease
Some people with Parkinsons may experience changes in their cognitive function, including problems with memory, attention, and the ability to plan and accomplish tasks. Stress, depression, and some medications may also contribute to these changes in cognition.
Over time, as the disease progresses, some people may develop dementia and be diagnosed with Parkinsons dementia, a type of Lewy body dementia. People with Parkinsons dementia may have severe memory and thinking problems that affect daily living.
Talk with your doctor if you or a loved one is diagnosed with Parkinsons disease and is experiencing problems with thinking or memory.
