How Can Hallucinations Be Treated
Drug treatments are often not that helpful for people with dementia. However hallucinations, particularly in people with dementia with Lewy bodies, may respond to anti-dementia drugs.
Antipsychotic medication can sometimes help to reduce severe or distressing hallucinations. They should only be used when other treatments have not worked, as they can cause unpleasant or dangerous side-effects. This medication should be regularly reviewed.
People with dementia with Lewy bodies are at particular risk of severe harmful reactions to antipsychotic medication. For more information see Non-drug approaches to changes in mood and behaviour.
How Commonly Do Parkinsons Disease Patients Develop Psychosis
Psychosis in Parkinsons disease generally comes in two forms: hallucinations or delusions . When hallucinations occur, they are mostly visual . Sometimes, they can be threatening, but this is less common. Auditory hallucinations are rare in Parkinsons disease and if they do occur, they are usually accompanied by visual hallucinations.
Delusions are usually of a common theme, typically of spousal infidelity. Other themes are often paranoid in nature Because they are paranoid in nature, they can be more threatening and more immediate action is often necessary, compared to visual hallucinations . It is not uncommon that patients actually call 9-1-1 or the police to report a burglary or a plot to hurt them.
Unfortunately, psychosis occurs in up to 40% of Parkinsons disease patients . In the early stage of Parkinsons disease psychosis, the patient often still has a clear understanding and retains their insight, but this tends to worsen over time and insight may eventually be lost. At later stages, patients may be confused and have impaired reality testing that is, they are unable to distinguish personal, subjective experiences from the reality of the external world. Psychosis in Parkinsons disease patients frequently occurs initially in the evening, then later on spills into the rest of the day.
Changes In Nerve Network Of Brain May Cause Presence Hallucinations
My first experience with hallucinations was terrifying not for me at first, but for my husband, who watched it happen.
We were on a cruise, and my anti-nausea medications interacted with my Parkinsons medications, resulting in two episodes. The first occurred in the middle of the ship around tons of people. I was sitting in the theater waiting for a show to start when my husband walked up and asked me to scoot over a seat. I told him that my mom was sitting there and had just walked over to the bar to get a drink. He was very confused because my mom was not with us on the trip.
Later that night, I had another episode. While my husband was sleeping, I tore apart our room, thinking I was packing. He woke up and asked, What are you doing? I told him that we had to go pick up our dog from doggy day care. After a few moments of total confusion, he reminded me that it was the middle of the night and we were in the middle of the ocean. He also told me that our dog was safe at my parents house and not at day care.
To learn more about Parkinsons hallucinations, I spoke with Andrea Frost, whose brother has the disease. She shared the following story with me:
I also talked with Alan Tobey, a 77-year-old living with Parkinsons, who said:
You May Like: Coconut Oil And Parkinson Disease
How To Care For Someone Who Experiences Hallucinations
If the person you care for experiences a hallucination, there are a few things youll want to do in the moment and others youll want to do when the moment passes.
The most important thing to remember is to never try and talk the person with Parkinsons out of their hallucination. They are actively experiencing it and by trying to talk them out of it, they may either feel like they arent being heard or that their experience is being diminished.
What matters in the moment is their safety and your reassurance that theyre going to be okay. You might calmly say, I understand that youre seeing X. Im not having that experience, and I just want you to know that everything is going to be okay, theres nothing dangerous happening here and youre safe.
Other strategies Dr. Joanne Hamilton, PhD, ABPP-CN of Advanced Neurobehavioral Health of Southern California, shared with us are to:
Here are a few actions you can take once the hallucination has passed:
Demystifying Hallucinations Night Terrors And Dementia In Parkinsons
This two-hour webinar includes extensive discussion about hallucinations, delusions, illusions and other examples of Parkinsons psychosis in Parkinson’s. Presenters: Rohit Dhall, MD, MSPH and Vergilio Gerald H. Evidente, Director, Movement Disorders Center of Arizona in Scottsdale. Pay particular attention to Dr. Rohit Dhalls description of the causes of PD psychosis as well as treatment options and what to discuss with your movement disorder specialist. Dr. Evidente gives a clear description on differences in PD dementia, Alzheimer’s and other dementias.
Also Check: What Are The Plaques Called That Cause Parkinson’s Disease
Hallucinations And Rem Sleep Disorders In Parkinsons Disease
At timestamp 1:58 in this recording of Thrive: HAPS 2020 Caregiver Conference, you will find a one hour talk by neurologist Joohi Jimenez-Shahed, MD. In it she delves into what REM sleep behavior disorder is and is not, and the distinctions between hallucinations, delusions, and delirium. Managment options for RBD and hallucinations are included.
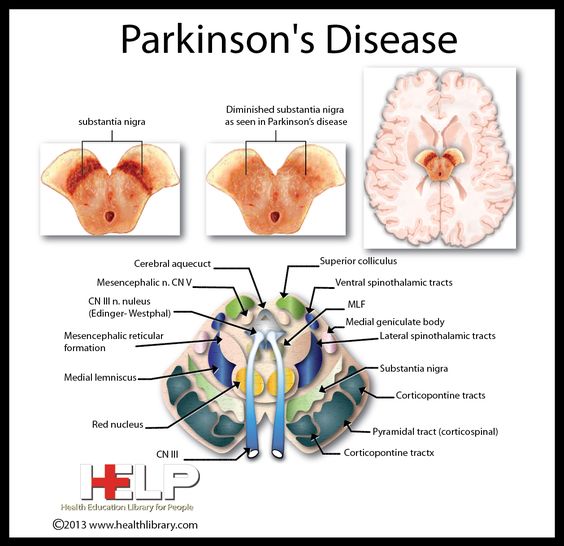
What Causes Psychosis In Parkinsons
Currently, there is not a clear understanding of the exact cause of Parkinsons disease psychosis, although certain brain chemicals and receptors are believed to play a role. In general, the condition is believed to be caused by either one of the following:
Side effect of dopamine therapy:
Although an exact causal relationship has not been established, some believe that this condition may be a side effect of dopaminergic therapy .2Dopaminergic therapy increases dopamine levels, helping improve motor symptoms in patients with Parkinsons disease. However, increasing dopamine levels can also cause chemical and physical changes in the brain that inadvertently lead to symptoms such as hallucinations or delusions.
Natural outcome of the disease:
This condition can be triggered by changes in the brain that occur regardless of taking dopamine enhancing medication. Some of these changes occur naturally as Parkinsons disease progresses.2
Don’t Miss: How Do You Diagnose Parkinson’s
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinsons report the experience of hallucinations or delusions.
When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of people with PD. However, it is important to note that these statistics sometimes include delirium, in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and isolated minor symptoms or minor hallucinations, including illusions, where instead of seeing things that are not there , people misinterpret things that are really there.
These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinsons. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinsons not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinsons is a complex disease and as it progresses the percentages and risk of symptoms will change.
What Should I Do When My Loved One Is Experiencing A Hallucination
Most importantly, dont try to convince your loved one that what theyre experiencing isnt real. Theyll feel like youre putting down an experience that seems authentic to them.
Once a person has lost insight, itll be very difficult to convince them that what theyre experiencing isnt happening. Trying to argue with them may agitate and even enrage the person. Making them anxious could cause their hallucinations to get worse.
Instead, talk to the person gently and reassuringly. You might say something like, I understand that you see a dog in the corner of the room. Everything is going to be OK. Youre safe. You might even say that the dog must have left already.
Remember that the person cant control what theyre experiencing. Try to be as sympathetic as you can when you talk to them.
One approach that can help is to turn on all the lights in the room. Hallucinations are more likely to happen in dimly lit areas, and this can be caused by disease-related changes that affect the eyes.
Then, have the person really focus on what theyre seeing. That may reset their brain and help them see whats actually in front of them.
If the person doesnt have insight, try a distraction. Move them to a different room. Turn on the TV or play a game they like.
Try to keep your loved one as calm as possible. If they become very agitated or violent, call their doctor or 911.
Also Check: Can You Take Viagra If You Have Parkinson’s
How To Treat Parkinsons Psychosis
Parkinsons psychosis can be caused by changes in the brain chemistry caused by Parkinsons disease. But it can also be caused by the medications that treat Parkinsons disease. Because of this, treatment for psychosis will begin with adjustments to the patients current medications to find a combination that improves movement without causing symptoms of psychosis.
If this adjustment in medication doesnt work, an antipsychotic medication may be added.
Examples Of Delusions In Pd
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression.
Read Also: What Is Dyskinesia In Parkinson’s
Caring For A Loved One With Parkinsons Psychosis
When a loved one is experiencing psychosis, it is important to be patient and avoid arguing with them.
In some cases, your loved one may still have the insight to recognize that these thoughts and feelings are not real. If so, you can explain the reality to them. If they do not have this insight, it is not productive to try to convince them otherwise instead, you should try to remain reassuring and calm.
Be sure that your loved one cannot access anything dangerous when experiencing psychosis and keep the home free of clutter to prevent triggers, falls, and injuries.
Work closely with your loved ones doctors to adjust medications as needed. It can also be helpful to check if eyeglasses or hearing aids are needed and to keep the home well-lit at night. Difficulty in vision and hearing can sometimes trigger hallucinations.
Palliative care can provide added support to family caregivers caring for a loved one with Parkinsons disease. To learn more about how Crossroads Hospice & Palliative Care supports patients with Parkinsons disease, please call 1-888-564-3405.
How Can You Tell If Someone Is Hallucinating
Sometimes the person may appear to be hallucinating, but there is another cause . The following tips can help to identify hallucinations:
- Hallucinations differ from misperceptions or misidentifications. Listen to what the person is describing, and check if anything could be causing what they are experiencing. For example, if they describe a swarm of insects, and there is a busy pattern on a carpet, it may be a misperception. By changing or covering the carpet, the misperception may stop.
- If the person seems to be having auditory hallucinations , arrange to have their hearing checked. If the person wears a hearing aid, check that it is working properly at the right setting, and encourage them to wear it. The person may be having problems with their hearing, rather than hallucinating.
- If the person seems to be having gustatory hallucinations , make sure they are getting regular dental check-ups to rule out other causes such as tooth decay or denture cream. For more information see Dental care and oral health.
You May Like: Why Does Parkinson’s Cause Orthostatic Hypotension
Who Is At Risk For Psychosis
Theres no predicting with certainty which patients with Parkinsons disease will go on to develop symptoms like hallucinations or delusions. A number of risk factors both internal and external- are associated with the condition.Some of these risk factors include: age, duration and severity of Parkinsons disease and the taking of dopamine therapy.3-6
Predictive Factors And Pathophysiology
Minor hallucinations/illusions
Patients with isolated minor hallucinations/illusions differed from patients without hallucinations only by the presence of more depressive symptoms on the CES-D rating scale, suggesting that depressive symptoms are a facilitating factor. Indeed, depression may sometimes trigger or aggravate hallucinations associated with deafness or ocular pathology . However, when we analysed depression according to CES-D cut-off scores, the difference between the Parkinsons disease patients with minor hallucinations/illusions and those with no hallucinations was not significant. Interestingly, hallucinations involving the deceased spouse have been reported in up to half of widowed persons, with a higher frequency in the elderly . In the present study, the `presence was that of a deceased relative in only three cases bereavement cannot therefore explain the bulk of the cases.
Dopaminergic agents and other treatments
In the present study, non-hallucinators were more likely to be on anticholinergics or selegiline than patients with hallucinations. A similar paradoxical, negative association between anticholinergics and hallucinations was found by Sanchez-Ramos and colleagues . This reflects the recommendation whereby the use of these drugs in patients with cognitive impairment is avoided because of the well-known risk of cognitive worsening and/or hallucinations in this population.
Cognitive impairment
Read Also: Parkinsons Bike Therapy
Don’t Miss: Can Parkinson’s Happen Suddenly
Section Header Managing Psychosis With Medication
Dont keep hallucinations or delusions a secret from your doctor. Medications — or changes to the medications you take — can help manage Parkinsons psychosis.
Streamlining your meds. The first thing your doctor may want to do is stop or lower your Parkinsons medication dose. They may boost dopamine levels in your brain. That improves motor symptoms but can also cause changes in your emotions or the way you act.
Antipsychotics. These medications balance your brain chemicals. Only a few are considered safe for people with Parkinsons disease. These include quetiapine and clozapine .
Pimavanserin . Another antipsychotic, this first-in-class drug was approved by the FDA in 2016 to treat hallucinations and delusions in Parkinsons disease linked with psychosis.
If you see a doctor who isnt part of your usual care team — say, in the emergency room or an urgent care setting — tell them you have Parkinsons disease and what medications you take for it.
Medications Used For Treating Psychosis
Antipsychotic agents are designed to balance abnormal chemical levels in the brain. Up until the 1990s, the use of antipsychotics in PD was controversial because the drugs used until that time work by reducing excess dopamine. This alleviated psychosis but caused dramatic worsening of PD motor symptoms.Fortunately, medications that are better tolerated by people with PD are now available. Today, there are three antipsychotic medications considered relatively safe for people with PD. They cause limited worsening of PD while treating hallucinations and delusions.
Read Also: What Are The Effects From Having Parkinson’s Disease
Other Symptoms Of Parkinsons Disease
There are numerous Parkinsons disease symptoms, some related to movement and some unrelated. In addition to hallucinations and delusions, people may experience other non-motor symptoms, such as poor sleep and vision problems, which often contribute to the development of hallucinations.
Other non-motor Parkinsons disease symptoms include:
Vision Problems Are Common In Parkinsons
Research has shown that visual symptoms are extraordinarily common in people living with Parkinsons. Visual symptoms may occur due to changes in the front of the eye due to dry eye, changes in the retina , or changes in how our eyes move together. At the same time, many other things can affect vision, including diseases such as age-related macular degeneration, glaucoma, and cataracts, which increase with age. Distinguishing between visual symptoms caused directly by Parkinsons versus one of these other conditions can be difficult.
Visual symptoms related to Parkinsons can be specific: eyes can feel dry, gritty/sandy, and may burn or have redness. You may experience crusting on the lashes, lids that stick together in the morning, sensitivity to light, or dry eye. On the other hand, symptoms can be non- specific: you may notice your vision just isnt what it used to be, and you have difficulty seeing on a rainy night, in dim lighting, or while reading, etc.
Recommended Reading: How Does Parkinson’s Disease Affect Mobility
Why Hallucinations Happen
According to Alzheimers Association, Hallucinations are false perceptions of objects or events involving the senses. These false perceptions are caused by changes within the brain that result from Alzheimers So it is the very underpinnings of the disease, mainly memory and cognitive function loss, that are to blame for the hallucinations in most cases. There are other possible culprits that are worth investigation with your loved ones primary care physician. Those include:
- Alcohol or drug abuse
- Physical issues, including kidney or bladder infections, dehydration, and intense pain
No matter the suspected cause, it is necessary to schedule an appointment with the patients physician immediately after the onset of hallucinations. While non-drug approaches are always the preferred method of treatment, it may be necessary to pursue a course of medication, in order to keep the patient calm during this potentially traumatic experience.
