Normal Ans Response To Standing
Postural change induces gravitational redistribution of blood volume, leading to changes in blood pressure. Upon standing, pooling of venous blood in the legs is countered by the normal sympathetic ANS to maintain standing blood pressure. Lying supine also causes gravitational redistribution of blood volume, and the normal ANS minimizes blood pressure from rising too high. Norepinephrine is the major neurotransmitter in the ANS regulation of blood pressure in response to postural changes. Sympathetic activation in response to standing leads to: venoconstriction with increased venous return an increase in heart rate and myocardial contractility with increased cardiac output and vasoconstriction with increased blood pressure. Normal activation of the intact ANS, along with sufficient circulating blood volume, prevents the gravity-induced fall in standing systolic blood pressure , maintaining cerebral perfusion and of other vital organs.
Low Blood Pressure In Parkinson’s Disease
This 2-page article discusses the frequency of orthostatic hypotension in those with PD, the cause, symptoms and several simple measures that can be used to restore normal blood pressure regulation, including medication evaluation, increase of fluids and salty foods, caffeine, frequent small meals, environment, clothing, slow position change, bed position and medication options.
Postural Changes In Hemodynamics
Two parkinsonian patients were unable to stand up within 15 seconds and remain standing without help and without disturbing the BP measurements. Therefore, the standing test was performed for 15 parkinsonian patients and for 17 healthy subjects.
One healthy subject and two parkinsonian patients showed OH . The maximum individual SBP decrease after at least 1 minute of standing was 7.9 ± 6.6 mm Hg for the parkinsonian patients and 0.2 ± 3.4 mm Hg for the healthy subjects . The parkinsonian group showed a seemingly different initial response of SBP, HR, and SV, but the difference was only significant for HR . Nine patients had mild to severe symptoms during standing: 3 experienced dizziness or restlessness 4 felt weak, unsteady, or miserable, or had nausea or vision changes and 2 felt unable to stand or had a decline in the level of consciousness . These 2 patients had to sit down after 4 and 6 minutes of standing, although OH was not present in one of them at that time. Only 2 healthy subjects had mild symptoms they felt tired upon standing . The symptom score was not significantly related to the BP changes for either group.
A subanalysis, separating the patients in a group with idiopathic Parkinson’s disease and a group with parkinsonism , showed that the orthostatic BP responses were not different between these patient groups either before therapy or during the cross-over trial.
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Symptoms Of Orthostatic Hypotension
Symptoms of orthostatic hypotension include lightheadedness, weakness, dizziness, difficulty thinking, feeling faint, and headache. Orthostatic hypotension is generally evaluated by measuring the blood pressure of a patient while sitting, or lying down, and again while standing. Currently, a person whose blood pressure drops more than 20 mm Hg in systolic pressure or more than 10 mm Hg in diastolic pressure is considered to have orthostatic hypotension. A new research study suggests a more accurate way to diagnose orthostatic hypotension is using a calculation called upright mean arterial blood pressure, which takes into account both the systolic and diastolic blood pressures. When this number is under 75 mm Hg, it indicates orthostatic hypotension.1
Stay Informed On Your Parkinsons Journey
Would you like to learn more about nOH and living well with Parkinsons?
Our Every Victory Counts® manual gives people living with Parkinsons, their care partners and their family members the tools they need to take control of their own Parkinsons treatment through a proactive approach to self-care.
a powerful new print edition
Its jam-packed with up-to-date information about everything Parkinsons, plus an expanded worksheets and resources section to help you put what youve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
Dr. Jose-Alberto Palma is Assistant Professor of Neurology and Assistant Director of the Dysautonomia Center at New York University. His work over the past years has been focused on the diagnosis, management and understanding on autonomic disorders in patients with autonomic synucleinopathies, such as Parkinson disease and multiple system atrophy, as well as in the search for biomarkers for early diagnosis of these disorders. He has been involved in several studies and clinical trials to develop new treatments for autonomic dysfunction, and to describe the premotor phase of Parkinson disease.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Full Financial Disclosures For The Last 12 Months
Alessandra Fanciulli: Dr. Fanciulli reports royalties from Springer Nature Publishing Group, speaker fees and honoraria from the Austrian Autonomic Society, Austrian Parkinson Society, Ordensklinikum Linz, International Parkinson Disease and Movement Disorders Society and Theravance Biopharma and research grants from the Stichting ParkinsonFond and the Österreichischer Austausch Dienst, outside of the submitted work.
Fabian Leys: Dr. Leys reports no disclosures.
Cristian Falup-Pecurariu: Dr. Falup-Pecurariu reports royalties from Springer Nature Publishing Group, speaker fees and honoraria from the International Parkinson and Movement Disorders Society, outside of the submitted work.
Roland Thijs: Dr. Thijs reports speaker fees from Novartis, consultancy fees from Theravance Biopharma and research support from the Dutch Epilepsy Foundation Dutch, the Netherlands Organization for Health Research and Development and De Christelijke Vereniging voor de Verpleging van Lijders aan Epilepsie, outside of the submitted work.
Gregor K. Wenning: Dr. Wenning reports consultancy fees from Biogen, Biohaven, Lundbeck, Minoryx, Takeda, Theravance and research support from the Austrian Science Fund, International Parkinson Disease and Movement Disorders Society and the Medical University Innsbruck, outside of the submitted work.
Management Of Orthostatic Hypotension In Parkinsons Disease
Issue title: Special Issue: Clinical management of Parkinsons disease: Essentials and new developments
Guest editors: Bastiaan R. Bloem and Patrik Brundin
Article type: Review Article
Authors: Fanciulli, Alessandraa * | Leys, Fabiana | Falup-Pecurariu, Cristianb | Thijs, Rolandc d | Wenning, Gregor K.a
Affiliations: Department of Neurology, Medical University of Innsbruck Innsbruck, Austria | Department of Neurology, Transilvania University, Faculty of Medicine Brasov, Romania | Department of Neurology, Leiden University Medical Centre, Leiden, The Netherlands | Stichting Epilepsie Instellingen Nederland , Heemstede, The Netherlands
Correspondence: Correspondence to: Alessandra Fanciulli, MD, PhD, Department of Neurology, Medical University of Innsbruck, Anichstraße 35, A-6020 Innsbruck, Austria. Tel.: +43 512 504 83238 E-mail: .
Keywords: Parkinsons disease, orthostatic hypotension, post-prandial hypotension, supine hypertension, nocturnal hypertension
DOI: 10.3233/JPD-202036
Journal: Journal of Parkinson’s Disease, vol. 10, no. s1, pp. S57-S64, 2020
Abstract
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Monitor Your Blood Pressure
You may find it useful to keep a diary of what triggers your symptoms and what makes them better or worse. This will help manage the problem.
If you have low blood pressure, you may need to tell the relevant driving authority, depending on what you drive.
At the time of printing, the government website states that you need to tell the DVLA in England Scotland and Wales or the DVA in Northern Ireland, if treatment for blood pressure causes side effects that could affect your ability to drive.
Please check with your relevant authority if you have problems with your blood pressure, as the rules may have recently changed.
Remember that you must contact your relevant driving licensing agency when you are diagnosed with Parkinsons.
Postural Adjustments And Countermeasures
- Avoid rising to a standing position too quickly.
- When getting out of bed, start by moving to a seated position first. Wait some period of time before slowly leaning into a stand.
- Similarly, when getting out of a car, keep your body supported and slowly rise out of the car.
- Many sources recommend elevating the head of your bed by 10 to 20 degrees or 4 inches to decrease nighttime hypertension , which should reduce the degree of blood pressure drop when rising.
- Physical countermeasures are techniques to contract the muscles below the waist for about 30 seconds at a time, which reduces blood volume in lower body peripheral vessels and encourages blood flow return to the heart. These countermeasures can help maintain blood pressure during daily activities and should be considered at the first symptoms of orthostatic hypotension symptoms or when standing for prolonged periods of time:
- Toe-raising
- Bending at the waist
- Slow marching in place
- Leg elevation
Also Check: What Essential Oils Are Good For Parkinson’s Disease
Tips: Avoiding Neurogenic Orthostatic Hypotension
- Drink lots of water and other fluids, at least one cup with meals and two more at other times of the day.
- Regularly practice gentle exercise and avoid long periods of inactivity.
- Eat small, frequent meals. Reduce alcohol intake and avoid hot drinks and hot foods.
- After consulting your doctor, increase your salt intake by eating prepared soups or pretzels. Note: for people with heart disease, this should be avoided.
- If you expect to be standing for a long period of time, quickly drinking two eight-ounce glasses of cold water will increase blood volume and causes blood pressure to go up for several hours.
- Try wearing compression garments such as anti-gravity stockings.
- Do isometric exercises, like marching your legs slowly in place, before getting up.
- Shift slowly from lying to sitting and then standing.
Printing made possible with a grant from Theravance. Content created independently by the Parkinsons Foundation.
For more insights on this topic, listen to our podcast episode Understanding Neurogenic Orthostatic Hypotension.
Data Analysis And Statistics
Autonomic function was determined on the basis of HR variability during Valsalva’s maneuver, and HR variability and BP changes during standing. The HR variability in the Valsalva tests was expressed as the ratio of the maximum tachycardia to the maximum bradycardia induced by the maneuver during the 30 seconds following the release of the strain . The highest Valsalva ratio was accepted. HR variability after standing was expressed as the ratio of the 30th and 15th interbeat intervals after standing . The BP responses after standing were defined as the SBP and DBP changes in the first and third minute of standing versus baseline .
During the standing tests, 1-minute averages of changes in BP, HR, and SV were calculated. Baseline values were defined as the last 1-minute averages before the posture change from a supine to upright position. OH was defined as a drop in SBP of 20 mm Hg after at least 1 minute of standing, as recommended by the American Autonomic Society and American Academy of Neurology . During the meal tests, 5-minute averages of the variable changes were calculated and baseline values were defined as the last 5-minute average values before the meal ingestion. PPH was defined as a drop in SBP of 20 mm Hg within 75 minutes after the start of meal ingestion .
Recommended Reading: Parkinsons Genetic Link
Managing Orthostatic Hypotension In Parkinsons Disease
Sometimes, orthostatic hypotension can be avoided with lifestyle approaches, including:
- Drinking lots of water and other fluids to stay hydrated, especially during warm weather months
- Avoiding abrupt changes in position
- Shifting slowly from lying to sitting and then standing
- Avoiding prolonged standing
- Limiting or reducing alcohol intake
- Increasing salt intake
- Eating small, frequent meals
- Avoiding hot drinks and hot foods1
Things that may worsen orthostatic hypotension, include:
- Fevers
- Straining when going to the bathroom
- Vigorous exercise
- Meals high in carbohydrates1
People with PD who have orthostatic hypotension may need changes in their medications, if their doctor determines their medications may be contributing to their symptoms. Physicians, specifically movement disorders specialists, are trained to know the best treatments for hypotension for PD patients and whether treatments for PD symptoms are causing hypotension. Other medications that may help manage orthostatic hypotension include Northera , ProAmatine® , Forinef® or Mestinon® . One potential side effect of these medications that raise low blood pressure when a person is standing is that they may cause high blood pressure when the person is lying down.1
How Common Is Noh In People With Parkinsons
An estimated 30 to 50% of people with Parkinsons experience nOH. The prevalence of nOH increases with both age and number of years of living with Parkinsons. Although nOH in Parkinsons is relatively common, not everyone will experience symptoms. For that reason, people with Parkinsons should be screened for nOH, even if they have no symptoms.
Conversely, nOH can be one of the earliest symptoms of Parkinsons and can appear several years even decades before the onset of motor problems like tremor or stiffness. Therefore, people who have nOH, but do not have any significant motor or cognitive symptoms, should also be monitored closely to watch for early signs or symptoms of Parkinsons.
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Supine Hypertension As A Treatment Consideration In Parkinsondisease
Because supine hypertension is another manifestation of thecardiovascular autonomic dysfunction that also causes nOH, it can occur inpatients with nOH regardless of treatment. To complicate matters, the treatmentsthat raise orthostatic BP may also increase BP when supine . Asdescribed in the preceding text, the risk of supine hypertension associated withindividual pressor agents used in the treatment of nOH may vary. In addition tothe appropriate selection of nOH treatment based on the supine hypertension riskprofile, 24-h ambulatory BP monitoring can provide the patient and clinicianwith information on when and under what circumstances the patient experiencesnOH symptoms and supine hypertension, and this information should be consideredwhen initiating or adjusting nOH pharmacotherapy .
Given that both nOH and supine hypertension pose risks to patientsafety, balanced management of the two conditions is often required. Todetermine the best treatment approach for the individual patient, healthcareproviders should consider factors such as comorbidities, concomitantmedications, and prognosis, as well as discuss the benefits and short- andlong-term risks with each patient .
How Is Blood Pressure Controlled
Blood pressure is changing up and down naturally during the day. It is higher if you are stressed or doing physical activity and lower when you are resting.
There are sensors in the main artery in the neck that report your blood pressure to the brain. This is part of the autonomic nervous system , which includes the brain, nerves and spinal cord. The ANS controls a number of automatic or autonomic functions , including the heart rate and blood pressure. As there is only a certain amount of blood in our body, the supply has to be managed so our brain monitors the blood pressure and sends messages to our heart and blood vessels to adjust it as needed.
During certain activities, some parts of the body need more blood than others. For example, during exercise your blood pressure increases so that your muscles can get more oxygen. Or, if you have eaten recently, more blood goes to your stomach to allow it to digest food, reducing blood pressure elsewhere .
Your body also senses when you stand up and stops blood pooling in your legs . It does this by increasing your heart rate and squeezing or contracting your blood vessels, to move blood around your body.
If blood does pool in your veins when you stand, less blood returns to the heart and as a result, less blood reaches the brain. This can cause dizziness or fainting. This is called postural hypotension and can be a problem for people with Parkinsons.
Read Also: Is Parkinson’s Disease Genetic Or Hereditary
Understanding The Neurologic Control Of The Cardiac System
Before we explore this issue, lets first learn a bit about the autonomic nervous system and about the cardiac systems place within it. The ANS is part of the peripheral nervous system, a network of nerves throughout the body. The ANS exerts control over functions that are not under conscious direction such as respiration, heart function, blood pressure, digestion, urination, sexual function, pupillary response, and much more. The ANS is further subdivided into the parasympathetic nervous system and the sympathetic nervous system. Both the parasympathetic and sympathetic nervous systems regulate most major organs. Often, they have opposite effects, with the sympathetic nervous system activating a system and the parasympathetic system calming it down.
One of the systems controlled by the ANS is cardiac regulation. Blood pressure sensors, known as baroreceptors, reside in the heart as well as in the carotid artery, the major artery in the neck. If the baroreceptors sense a change in the blood pressure, a signal is sent to particular areas in the brain. From there, the autonomic nervous system sends signals to the heart to control heart rate and cardiac output. Signals are also sent to the blood vessels to change the size of their diameter, thereby regulating blood pressure.
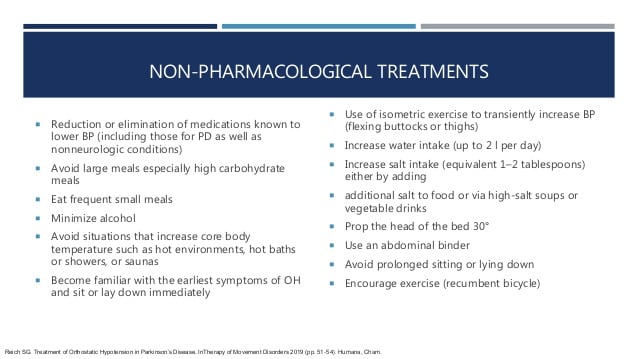
Preventing And Treating Orthostatic Hypotension: As Easy As A B C
Drug therapy alone is never adequate to treat orthostatic hypotension. A patient-oriented approach that emphasizes education and nonpharmacologic strategies is critical. This article provides easy-to-remember management recommendations, using a combination of drug and non-drug treatments that have proven effective.
You May Like: Parkinson Life Expectancy Early Onset
Improvement In Severe Orthostatic Hypotension Following Carbidopa Dose Reduction
Published online by Cambridge University Press: 21 December 2017
- Pharmacist Department of Pharmacy Surrey Memorial Hospital Fraser Health Authority Surrey, BC, Canada
- John L. Diggle
- Affiliation:Neurologist and Regional Medical Director and Head Regional Department of Medicine Fraser Health Authority Surrey, BC, CanadaClinical Assitant Professor Faculty of Medicine University of British Columbia Vancouver, BC, Canada
- Penny P. Bring
- Affiliation:Clinical Pharmacy Specialist Neurology Department of Pharmacy Surrey Memorial Hospital Fraser Health Authority Surrey, BC, CanadaClinical Instructor Faculty of Pharmaceutical Sciences University of British Columbia Vancouver, BC, Canada
- *
- Correspondence to: A.C.W. Lau, BSc , Pharmacist, Surrey Memorial Hospital Pharmacy Department, Fraser Health Authority, 13750 96 Avenue, Surrey, BC, Canada V3V 1Z2. Email:
