Is Parkinsons Disease Fatal
Parkinsons disease itself doesnt cause death. However, symptoms related to Parkinsons can be fatal. For example, injuries that occur because of a fall or problems associated with dementia can be fatal.
Some people with Parkinsons experience difficulty swallowing. This can lead to aspiration pneumonia. This condition is caused when foods, or other foreign objects, are inhaled into the lungs.
What Symptoms Can Be Expected In Advanced Pd
- Shortness of breath 54%
- Problems in swallowing 40%14
In an analysis of 339 death certificates and medical notes in the UK, pneumonia was found to be a terminal event in 45%.13
Caregiver distress with choking and the risk of choking to death is also mentioned in a separate study in to experiences regarding all stages of PD.4
In a survey of symptoms and their association with quality of life, in those patients with advanced disease, uncontrolled pain, anxiety and hallucinations were significantly associated with poor quality of life.9
Seizures are also noted in a description of the last phase of Parkinsonian syndromes,15 and in retrospective studies of PD patients overall.16,17
These above symptoms often occur on the background of weight loss, pain, and cognitive impairment. It is important therefore to note which medications given at the end of life may exacerbate these symptoms, and which should be considered in anticipation of them.
Interacting With Parkinsons Disease
Here are a few simple, but effective strategies to employ when faced with understandably uncomfortable scenarios:
- Change the subject. When symptoms manifest, sometimes talking about something else can help calm patients down. Whether its a recollection from their past or just a different topic, changing the conversation can turn chaos into calm.
- Take it outside. Fresh air and sunlight can help improve oxygen flow and trigger mood stabilizers in the brain.
- Get busy. Having an activity, especially something patients find meaningful, can help set them on a more even keel. Old hobbies or household tasks generally work best in these instances.
- Have a snack. Most of us get cranky when were hungry or thirsty patients with Parkinsons are no different. A light snack, some water or juice can help stabilize behaviors.
- Adjust the ambience. Sometimes, something as simple as a rooms brightness or temperature can contribute to a patients acting out. Too much noise can overstimulate too little light can cause anxiety excessive heat or cold can trigger anger. Adjusting lighting and temperatures, turning the volume down on the TV or the radio, or simply offering a cozy blanket may help restore the peace.
- Ask for help. Looping in a patients doctor may reveal underlying medical conditions, like urinary tract infections, behind the sudden shifts in behavior.
Also Check: Does Parkinson’s Affect The Eyes
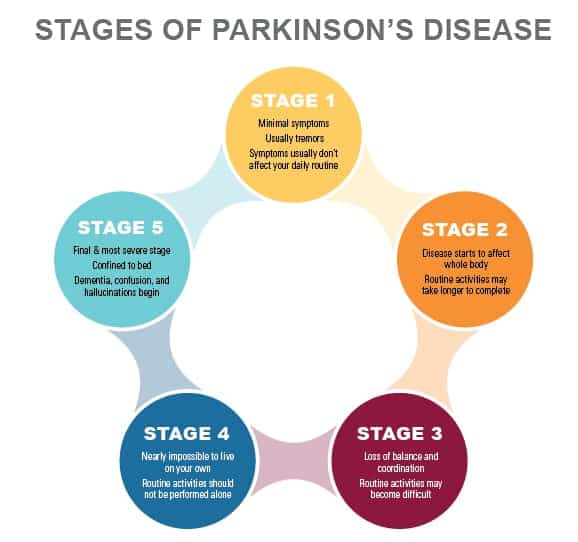
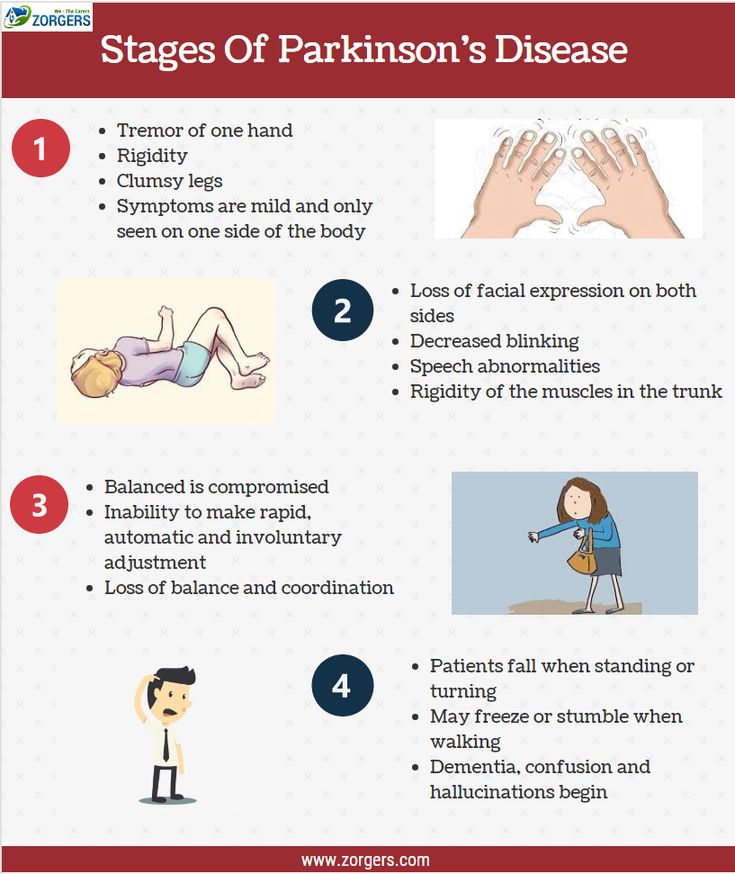
Stages Of Parkinsons Disease
While there may be no cure, Parkinsons follows a predictable path. In the early stages, symptoms are mild and inconvenient by the end stages, symptoms are incapacitating.
- Stage One: Patients begin to experience tremors on one side of the body. One arm or leg will feel heavy, but not to the point it interferes with daily life. Symptoms may be so slight, they can be sometimes overlooked.
- Stage Two: Symptoms are clearly visible and affect both sides of the body. Patients become stooped as tremors grow more pronounced. Muscles are rigid, making it difficult to bend their trunk, arms, and legs facial muscles begin to freeze at this stage, creating an almost mask-like appearance. At this stage, however, balance is not yet impaired, so most patients continue to live independently.
- Stage Three: Balance becomes increasingly compromised, and reflexes and coordination deteriorate, elevating serious risks of falling. Muscles grow so stiff that patients can only take short, shuffling steps. Tremors become more serious, and yet most patients can still complete daily tasks, though it requires more time and greater effort.
- Stage 4: Patients can no longer live on their own. Balance is so weak that while it may be possible for them to stand, they will not be able to move without a walker. Some freeze periodically, unable to move for short periods of time.
- Stage 5: Patients cannot walk or stand without assistance and require round-the-clock care.
How Is Parkinson Disease Treated
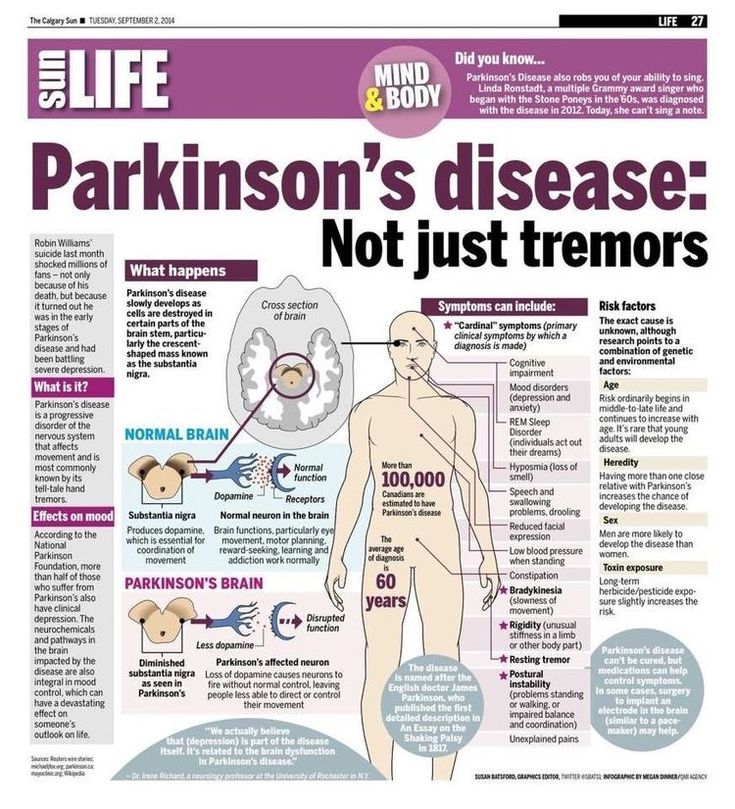
Parkinson disease can’t be cured. But there are different therapies that can help control symptoms. Many of the medicines used to treat Parkinson disease help to offset the loss of the chemical dopamine in the brain. Most of these medicines help manage symptoms quite successfully.
A procedure called deep brain stimulation may also be used to treat Parkinson disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Also Check: Does Physical Therapy Help Parkinson’s Disease
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinsons disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinsons disease.
The overlap in symptoms between Lewy body dementia and Parkinsons disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinsons disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinsons disease itself isnt fatal, but complications can be.
Research has shown a median survival rate of about
Hospice Eligibility Of End
Since Parkinsons disease is progressive, patients need hospice care. If your family member or any loved one has been diagnosed with Parkinsons disease, expect that there will be a decline in their motor abilities. They will need professional nursing care to attend to their needs because it will be harder for them to speak and express their struggles.
Here are the things you need to observe to determine if the patient already needs hospice care:
- Difficulty in breathing and oxygen supply is necessary
- Difficulty in walking where a wheelchair is already needed
- Hard to understand speech
- Difficulty in eating and drinking
- More complications occur, such as pneumonia, sepsis, pyelonephritis, decubitus ulcers, and other comorbidities
Recommended Reading: What Disease Is Like Parkinson’s
What Are The Stages Of Parkinson Dementia
- depression and anxiety
- mild cognitive impairment slight memory problems and problems with activities that require planning and organisation
- dementia a group of symptoms, including more severe memory problems, personality changes, seeing things that are not there and believing things that are not true
End Stage Of Dementia
The end stage of dementia is the most difficult stage for those suffering from the disease, and also for family members, caregivers, and healthcare professionals. Victims lose what is left of their intellectual and physical capabilities and become completely dependent on others. The model is still shifting in considering end stage dementia an end of life condition experts are pushing this model in order to advocate for better pain and distress management for those suffering at their end.
Don’t Miss: What Part Of The Body Does Parkinson’s Affect
Motor Symptoms And Global Disability
Motor symptoms, as measured using the Unified Parkinsons Disease Rating Scale , Hoehn and Yahr Scale and the Progressive Supranuclear Palsy Rating Scale , were significant predictors of mortality in patients with PDRD. Beyer et al found higher mean UPDRS scores, 65 versus 42 , suggesting that greater motor impairment predicted death. Studies with median follow-up times ranging from 4 to 8 years estimated the association of 10-unit increases in baseline motor UPDRS Score on mortality and found statistically significant increased HRs for mortality of 1.17 up to 1.4 for each 10-unit increase in UPDRS Score. Baseline H& Y staging was significantly higher among those who died ) compared with those who survived ). Posada et al went further by splitting H& Y into early and later progression stages at baseline as a predictor for mortality and found that HRs increased by stage, from 1.5 for H& Y stages 1 and 2 to 2.3 for H& Y stages 35, both compared with patients with no PD and after controlling for comorbidities and demographic characteristics. Oosterveld et al stratified UPDRS total motor scores by greater than or equal to 30 compared with less than 30 and found an HR of 1.63 . Chiu et al compared the association of PSPRS scores on mortality and found increased HRs of 1.96 for 3548 on the PSPRS, 2.99 for 4862 and 8.55 for greater than 62 when compared with scores of 034.
What Are The 5 Stages Of Parkinsons Disease
Parkinsons disease is a neurological movement disorder thats progressive, meaning symptoms worsen over time. According to the Parkinsons Foundation, most people move through the stages of Parkinsons disease gradually .
Theres no lab test that can tell a person which stage their disease is in. Instead, its based on how severe a persons movement symptoms are, and how much the disease impacts their ability to go about daily life.
While the stages of Parkinsons disease can look a little different for everyone, heres a typical pattern of the disease, per the Parkinsons Foundation:
Recommended Reading: What Type Of Doctor Treats Parkinson’s Disease
What To Expect In The Late Stages Of Parkinsons Disease
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinsons Disease In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinsons Disease Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
Stage : Mild Dementia
At this stage, individuals may start to become socially withdrawn and show changes in personality and mood. Denial of symptoms as a defense mechanism is commonly seen in stage 4. Behaviors to look for include:
- Difficulty remembering things about ones personal history
- Difficulty recognizing faces and people
In stage 4 dementia, individuals have no trouble recognizing familiar faces or traveling to familiar locations. However, patients in this stage will often avoid challenging situations in order to hide symptoms or prevent stress or anxiety.
You May Like: Is Thumb Twitching A Sign Of Parkinsons
Also Check: Things To Help Parkinson’s
The Progression Pf Parkinsons Disease
Parkinsons develops differently in each patient. Some deteriorate to the end stage of Parkinsons rapidly, while others remain strong and active for years, and theres no clear explanation for why.
While exercise and physical therapy can slow disease progression, theres no known cure. Even the healthiest patients will eventually decline until the end stage of Parkinsons, when they are left completely dependent on family and caretakers.
For those with loved ones whove been diagnosed with Parkinsons, it helps to know the road ahead. An awareness of whats to come makes it easier to offer help as conditions decline, and ask for help when they become too much to manage alone.
Parkinsons Disease: When Is It Time For Hospice
Knowing when its time for hospice care when living with Parkinsons Disease can be difficult as the disease may take many years to progress and each person with the disease may also exhibit a range of different symptoms. However, entering the end-stages of the disease , patients will have symptoms that will indicate that it is time to seek hospice assistance:
Recommended Reading: Latuda And Parkinson’s Disease
Study Designs And Descriptions Of Included Studies
The 42 studies were published until February 2020. The study designs were: retrospective cohort studies, prospective cohort and longitudinal studies, casecontrol studies and cross-sectional studies. Predictors of mortality included demographic and clinical markers, medical events, medication changes, disease-specific symptoms and patient and caregivers ratings of health-related quality of life. Eight studies described both predictors of mortality and causes of death.
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
Don’t Miss: 7 Helpful Hand Exercises For Parkinson’s
How Is Parkinson’s Managed
There is currently no cure for Parkinsons but there are medications and therapies that can help to manage Parkinsons symptoms.
Medicines that increase the level of dopamine in the brain are the main treatment used to manage the symptoms of Parkinson’s. Medicines are tailored to each individuals needs.
Symptoms will get worse when someones Parkinsons medicines are wearing off and improve again after Parkinsons medicines are taken. If people with Parkinsons do not get their medication at the right time, it leads to their motor symptoms becoming uncontrolled. It can take some time to get their symptoms under control again. If you work in a hospital or care home, it is important to be aware that medicine timings will vary from person to person and may be different to ward medicine rounds.
As well as medicines, surgical options are available for some people with Parkinson’s, depending on their symptoms.
Treatments can help to manage the symptoms, but may become less effective in the later stages of the condition.
Parkinsons UK has more information on how Parkinsons affects people and how it can be managed.
Causes Of Parkinsons Disease
Parkinsons disease is caused by a loss of nerve cells in part of the brain called the substantia nigra. This leads to a reduction in a chemical called dopamine in the brain.
Dopamine plays a vital role in regulating the movement of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinsons disease.
Exactly what causes the loss of nerve cells is unclear. Most experts think that a combination of genetic and environmental factors is responsible.
Don’t Miss: Does Viagra Help Parkinson’s
Palliative Care Management Of Non
Patients with PD can develop non-motor manifestations, categorized into autonomic dysfunction, cognitive impairment, neuropsychiatric disorders, and sleep disturbances. At the end-stage of PD, non-motor symptoms become more common and can become the most prominent medical problem, leading to increasing decline in quality of life both for patient as well as increasing caregiver burden . Non-motor symptoms occur in up to 50% of PD patients especially in association with the medication off state and may become worse by anti-PD medications . Almost one third of patients reports their non-motor symptoms to be at least as debilitating as their motor symptoms .
All patients with motor fluctuations face at least one non-motor problem during the off phase . In end-stage of PD, dementia, psychosis, and falls become more complex to manage than the motor complications as a result, managing non-motor aspects is important to increase quality of life and decrease the burden of illness . Chaudhuri and co-workers, using a new 30-item non-motor symptom screening questionnaire , found noticeably high scores among PD patients for impaired taste/smell, impaired swallowing, weight loss, constipation, urinary urgency, forgetfulness, dribbling, sadness, hallucinations, anxiety, sexual dysfunction, falling, reduced concentration, daytime sleepiness, vivid dreams, and sweating .
What You Can Expect
Parkinson does follow a broad pattern. While it moves at different paces for different people, changes tend to come on slowly. Symptoms usually get worse over time, and new ones probably will pop up along the way.
Parkinsonâs doesnât always affect how long you live. But it can change your quality of life in a major way. After about 10 years, most people will have at least one major issue, like dementia or a physical disability.
Recommended Reading: Can Medication Cause Parkinson’s
