What Medications Are Used To Treat Parkinsons Symptoms
Since many of the motor symptoms of Parkinsons are the result of a lack of dopamine in the brain, most drugs used to treat Parkinsons are aimed at temporarily replenishing or imitating dopamine. The following list is a guide to medications approved by Health Canada to treat symptoms of Parkinsons1. Speak to your doctor for detailed information regarding effectiveness and side effects of a particular drug.
Levodopa
- Converted into dopamine in the brain and stored in nerve cells to replace depleted dopamine
- Combined with another drug, carbidopa or benzerazide, allows more levodopa to get to the brain and reduces side effects
- Helps improve muscle rigidity and movement
- Side effects include dyskinesias
- Over years of use, may be associated with wearing off
Dopamine Agonists
- Mimics or imitates action of dopamine
- Can be used as initial treatment or with levodopa in advanced stages
- Side effects include sleepiness, hallucinations, leg swelling and obsessions with food, sex and activities such as shopping, gambling and Internet use Amantadine
- Enhances dopamine release and blocks glutamate, a brain transmitter
- Used to treat early symptoms
- Can reduce dyskinesias and improve wearing off
Dopamine Agonist
Progress In The Treatment Of Parkinsons Disease
Despite the fact that 200 years passed since the discovery of PD, it was not until later in the 20th century that progress in the treatment of PD was achieved, predominantly due to the limited understanding of PD pathophysiology. Given Carlssons discoveries of DAs involvement in the 1950s, it became clear that PD development involved dopaminergic cell death and a decrease of DA in the striatum and other structures of the forebrain. The first steps towards treatment were made by Carlsson , who proposed targeting this DA deficiency to facilitate symptom reduction.
Causes Of Parkinsons Disease
At present, we do not know the cause of Parkinsons disease. In most people there is no family history of Parkinsons Researchers worldwide are investigating possible causes, including:
- environmental triggers, pesticides, toxins, chemicals
- genetic factors
- combinations of environment and genetic factors
Don’t Miss: Parkinson’s Disease Latest News
Deep Brain Stimulation Dbs
Benabid et Al.46 were the first to propose that chronic high-frequency deep brain stimulation could simulate the effects of a lesion and avoid the need to make a destructive brain lesion and might be a useful treatment in PD. They proposed that chronic stimulation could be accomplished by connecting an electrode implanted into a specific brain target to a programmable stimulator. Optimal stimulation parameters could be determined by varying the electrode configuration , and the stimulation voltage, pulse width, and frequency. DBS had previously been employed as a therapy for intractable pain and dyskinesia 47,48 and was shown to be well tolerated. The principal advantage of DBS is its capacity to provide functional benefits without the necessity of creating a destructive brain lesion, thereby avoiding adverse events caused by damage to neighboring structures. This is a particular advantage if bilateral procedures need to be performed. It also permits targeting regions in the brain that one might be unwilling to lesion such as the subthalamic nucleus or the GPi bilaterally. Other advantages of DBS include the potential to adjust the stimulator at any time after surgery in order to maximize benefits and minimize adversity.
Further, the procedure does not mitigate against the introduction of a more effective therapy in the future that requires the integrity of the basal ganglia system.
Diagnosis Of Parkinson’s Disease

The diagnosis of PD is clinical and requires bradykinesia, defined as slowness of movement and decrement in amplitude or speed, usually assessed using finger tapping, foot tapping or pronationsupination hand movements. In addition, rest tremor or rigidity is required to confirm a parkinsonian syndrome. Tremor was absent at presentation in 30% in one series of pathologically proven PD. Patients with suspected PD should be referred quickly and untreated to a specialist in movement disorders for evaluation. Key points for discussion at diagnosis include the need to inform vehicle licensing agencies and insurers, signposting to written or web-based information on newly diagnosed PD, and provision of contact details for the local PD nurse specialist .
Current International Parkinson and Movement Disorder Society diagnostic criteria for Parkinson’s disease adapted from Postuma RB, Berg D, Stern M et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 2015 30:1591601. At least two supportive criteria and no red flags required for a diagnosis of clinically established Parkinson’s disease. Conditions in italics should be considered if the corresponding exclusion criteria or red flags are present.
Also Check: Best Diet For Parkinson’s Patients
Symptomatic Treatment Of Motor Symptoms
Levodopa
A majority of patients with PD require levodopa therapy within 2 years of symptom onset. Levodopa, the most effective drug in the treatment of PD, is almost always combined with carbidopa or benserazide, aromatic acid decarboxylase inhibitors that prevent its peripheral metabolism and markedly reduce the risk of nausea. Increasing the ratio of carbidopa:levodopa from the current standard 1:4 has been shown to increase on time without dyskinesia and reduce off time.
The global antiparkinsonian efficacy of levodopa is so predictable that a positive therapeutic response is used to support the diagnosis of PD. Adverse effects of levodopa include nausea and vomiting, orthostatic hypotension, sedation, confusion, sleep disturbance, hallucinations and dyskinesias. There are many different types of dyskinesia but peak-dose chorea or stereotypy and wearing off dystonia are most common. About half of the patients experience wearing off, and a third experience dyskinesias within 2 years after initiation of levodopa therapy. Latency from ingestion of levodopa to observable therapeutic benefit can be shortened by taking levodopa on an empty stomach , avoiding or reducing protein intake, or by crushing the levodopa tablet and mixing it with a carbonated beverage.
Other drugs
Besides levodopa, there are many other types of medications available for the treatment of PD-related motor symptoms: anticholinergics, amantadine, MAOIs, COMTIs, dopamine agonists and istradefylline.
Physical Occupational And Speech Therapy
Physical, occupational and speech therapists can be important partners in the treatment of Parkinsons disease. Physical therapy can improve your gait and direct you to the right exercise regimen. Occupational therapy can be helpful to maximize your fine motor skills. Speech therapy can be useful to address speech and language barriers that may arise with Parkinsons disease.
Read Also: What Medications Are Used To Treat Parkinson’s Disease
Dietary Considerations With Medications
Treatments are only effective in moderating the symptoms of the disease, mainly with drugs including levodopa and dopamine agonists. Once too many dopamine producing cells have been lost however, the effects of L-DOPA become less effective. Once this occurs, a complication known as dyskenesia commonly occurs in which subjects undergo involuntary writhing movements despite the use of L-DOPA. The effects of dyskenesia vary between periods of high symptoms and low symptoms. In order to limit the onset of dyskenesia, typical L-DOPA dosages are kept as low as possible while still achieving desired results. Lastly, in cases in which drugs are ineffective, deep brain stimulation and surgery can be used to reduce symptoms.
Levodopa is taken orally and is absorbed through the small intestines into the blood, competing for access with natural proteins. Additionally, once the drug has entered the blood stream, L-DOPA utilizes the same pathways to cross the blood brain barrier as natural protein. Only about 5 10% of levodopa crosses the blood brain barrier, while the remaining is metabolized elsewhere in the body. The metabolism of medications elsewhere is known to cause side effects such as nausea, dsykinesias, and stiffness.
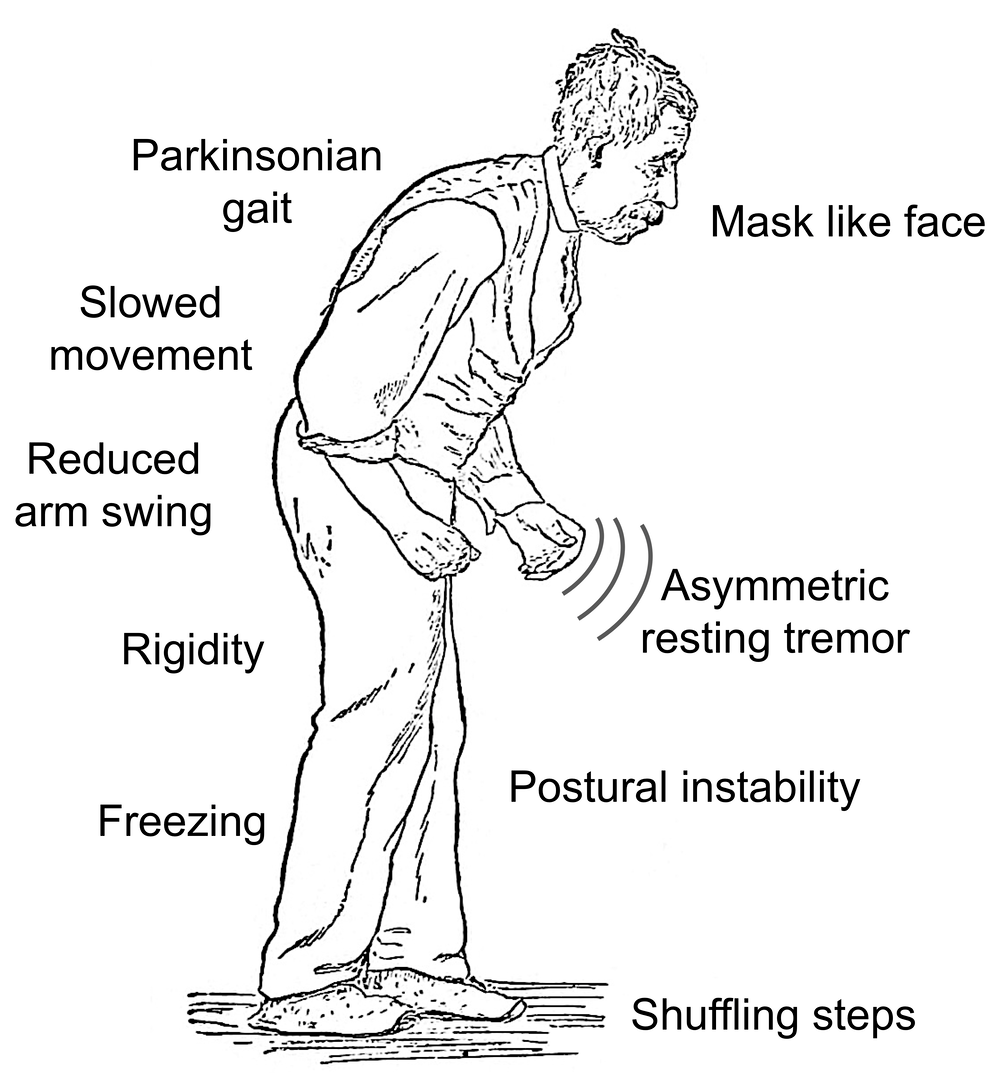
What Are The Symptoms
The best-known symptoms of Parkinson’s disease involve loss of muscle control. However, experts now know that muscle control-related issues aren’t the only possible symptoms of Parkinson’s disease.
Motor-related symptoms
Motor symptoms which means movement-related symptoms of Parkinsons disease include the following:
Additional motor symptoms can include:
- Blinking less often than usual. This is also a symptom of reduced control of facial muscles.
- Cramped or small handwriting. Known as micrographia, this happens because of muscle control problems.
- Drooling. Another symptom that happens because of loss of facial muscle control.
- Mask-like facial expression. Known as hypomimia, this means facial expressions change very little or not at all.
- Trouble swallowing . This happens with reduced throat muscle control. It increases the risk of problems like pneumonia or choking.
- Unusually soft speaking voice . This happens because of reduced muscle control in the throat and chest.
Non-motor symptoms
Several symptoms are possible that aren’t connected to movement and muscle control. In years past, experts believed non-motor symptoms were risk factors for this disease when seen before motor symptoms. However, theres a growing amount of evidence that these symptoms can appear in the earliest stages of the disease. That means these symptoms might be warning signs that start years or even decades before motor symptoms.
Non-motor symptoms include:
Stages of Parkinsons disease
Read Also: Does A Neurologist Treat Parkinson’s
Encouragingthe Use Of Assistive Devices
An electric warming tray keeps food hot and permits thepatient to rest during the prolonged time that it takes to eat. Specialuten-sils also assist at mealtime. A plate that is stabilized, a nonspill cup,and eating utensils with built-up handles are useful self-help devices. Theoccupational therapist can assist in identifying appropriate adaptive devices.
Progression Of Parkinsons Disease
The disease progression of PD from diagnosis has been conceptualised into four stages . It is also important to recognise a prodromal phase in which non-motor symptoms, such as anosmia, constipation and rapid-eye-movement sleep behaviour disorder may predict the development of motor PD. Motor complications are more common as PD progresses, and typify transition to the complex phase. Many so-called axial symptoms of later stage PD, such as dysphagia, gait disturbance and falls, do not respond to levodopa, but may be helped by multidisciplinary team input. Dementia occurs in up to 80% of people with PD after 20 years disease duration. The rate of PD progression is heterogeneous and is generally more rapid in those with older age and more severe motor impairment at onset.
Stages of Parkinsons disease. RBD = rapid eye movement sleep behaviour disorder.
You May Like: How Early Can You Get Parkinson’s
Parkinson’s Disease Nurse Specialists
The development of specialist peripatetic nurses for Parkinson’s disease has been led by the Parkinson’s Disease Society in the UK. From small beginnings, around 100 are now funded from various sources including the NHS. The nurses have a number of roles but they primarily act as a key worker for the patient with Parkinson’s disease, liaising with therapists, social services, the primary and secondary care teams, etc. They serve to educate the patient, relatives, and members of the medical and allied professions about the condition. Their ability to help the patient with complex changes in medication, including apomorphine infusions, within set limits can be invaluable. Parkinson’s disease nurse specialists have been the subject of a recent large RCT which showed significant improvements in an open label patient global impression scale at no additional cost to the NHS. No advantages in quality of life or mortality were found, but the study was confounded by selegiline withdrawal.
Who Does It Affect

The risk of developing Parkinsons disease naturally increases with age, and the average age at which it starts is 60 years old. Its slightly more common in men or people designated male at birth than in women or people designated female at birth .
While Parkinsons disease is usually age-related, it can happen in adults as young as 20 .
Don’t Miss: Essential Oils Treatment For Parkinson’s
What Is Parkinsons Disease
Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
Recommended Reading: Parkinsons And Bad Taste In Mouth
Dysfunctional Protein Clearance Systems
There are two central protein clearance systems within cells responsible for the removal of dysfunctional proteins: the ubiquitin-proteasome system and the autophagy-lysosome pathway. The UPS is primarily responsible for breaking down abnormal proteins, and it does so by tagging them with ubiquitin and transporting them to the proteasome for degradation. The autophagy-lysosome pathway is divided into three constituents: macroautophagy, microautophagy, and chaperone-mediated autophagy . Briefly, in macroautophagy, intracellular components, including cytosolic proteins, are engulfed by the autophagosome, which then fuses with the lysosome, leading to the breakdown of its contents. On the other hand, in microautophagy, the lysosome alone engulfs and destroys cytoplasmic components. CMA is a more selective process, whereby molecular chaperones target specific proteins and transport them to the lysosome for degradation . Monomeric -synuclein is generally cleared by both the UPS and the autophagy-lysosome pathway , and damage in either of their machineries is implicated in the pathogenesis of PD by contributing to the accumulation of defective proteins, in particular soluble misfolded -synuclein .
You May Like: What Tests Are Done To Diagnose Parkinson’s
When To Start Treatment
Deciding when to start drug therapy for Parkinsons disease should be individually tailored to a patients symptoms, circumstances and comorbidities. Treatment is indicated when symptoms impact on quality of life. When treatment is needed there is no evidence to support undue delay because of concerns about levodopa toxicity or the development of treatment resistance.3 The aim is to control symptoms and maintain an on state.
Some drugs with good symptomatic benefit are speculated to have a role in neuroprotection and some specialists advocate their use from the time of diagnosis.4 Delayed start trials have been used to try and differentiate symptomatic from disease-modifying effects. A recent delayed start study of rasagiline, a monoamine oxidase B inhibitor, in treatment-naïve patients with mild Parkinsons disease showed a small benefit in the low-dose treatment group. This was not seen with the 2 mg dose and a clear explanation for this has not been established.5 Further studies are needed before such treatments are considered truly disease modifying. Until a drug is unequivocally proven to slow disease progression, the time to commence treatment will remain contentious.
Parkinsons Disease: Symptoms Treatment Options And Nursing Care
Phil Cotterell Parkinsons disease nurse specialist, Community Neurological Rehabilitation Team, Sussex Community NHS Foundation Trust, Worthing, England
Why you should read this article:
-
» To understand your role in supporting and improving the quality of life of patients with Parkinsons disease and their family and carers
-
» To recognise motor and non-motor symptoms of Parkinsons disease and potential treatment options
-
» To ensure the care you provide to patients is holistic and considers not only the physical effect of Parkinsons disease, but also the psychological and emotional effects that individuals may experience
Idiopathic Parkinsons disease is a progressive neurodegenerative condition that causes various motor and non-motor symptoms and will often have life-changing effects for those with the condition, as well as for their family and carers. Nurses can make a significant difference to the lives of those affected by Parkinsons disease, whether in the acute setting, community setting or in care homes. This article explores the causes and progressive clinical pathway of IPD using an evidence-based approach. It emphasises the valuable role of the multidisciplinary team and of the nurse, in particular, in monitoring and improving the quality of life of those with the condition and their family and carers.
Nursing Standard. doi: 10.7748/ns.2018.e11207
Don’t Miss: Is Restless Leg Syndrome A Precursor To Parkinson’s
What Causes The Condition
Although there are several recognized risk factors for Parkinsons disease, such as exposure to pesticides, for now, the only confirmed causes of Parkinsons disease are genetic. When Parkinsons disease isnt genetic, experts classify it as idiopathic . That means they dont know exactly why it happens.
Many conditions look like Parkinson’s disease but are instead parkinsonism from a specific cause like some psychiatric medications.
Familial Parkinsons disease
Parkinsons disease can have a familial cause, which means you can inherit it from one or both of your parents. However, this only makes up about 10% of all cases.
Experts have linked at least seven different genes to Parkinson’s disease. They’ve linked three of those to early-onset of the condition . Some genetic mutations also cause unique, distinguishing features.
Idiopathic Parkinsons disease
Experts believe idiopathic Parkinsons disease happens because of problems with how your body uses a protein called -synuclein . Proteins are chemical molecules that have a very specific shape. When some proteins dont have the correct shape a problem known as protein misfolding your body cant use them and can’t break them down.
With nowhere to go, the proteins build up in various places or in certain cells . The buildup of these Lewy bodies causes toxic effects and cell damage.
Induced Parkinsonism
The possible causes are:
How Is It Diagnosed
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking you questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes. However, most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
Don’t Miss: What Is Parkinson Like Syndrome
Rapid Eye Movement Sleep Behaviour Disorder
REM sleep behaviour is associated with PD and is a prodromal symptom in many cases. Patients with REM sleep disorder often physically act out vivid dreams during REM sleep, which can affect their quality of life and that of their family and carers. NICE recommends the off-label use of clonazepam or melatonin . Benzodiazepines are cautioned in the elderly population therefore, this patient cohort must be monitored closely by their care team if started on clonazepam.
How Does This Condition Affect My Body
Parkinsons disease causes a specific area of your brain, the basal ganglia, to deteriorate. As this area deteriorates, you lose the abilities those areas once controlled. Researchers have uncovered that Parkinsons disease causes a major shift in your brain chemistry.
Under normal circumstances, your brain uses chemicals known as neurotransmitters to control how your brain cells communicate with each other. When you have Parkinsons disease, you dont have enough dopamine, one of the most important neurotransmitters.
When your brain sends activation signals that tell your muscles to move, it fine-tunes your movements using cells that require dopamine. Thats why lack of dopamine causes the slowed movements and tremors symptoms of Parkinson’s disease.
As Parkinson’s disease progresses, the symptoms expand and intensify. Later stages of the disease often affect how your brain functions, causing dementia-like symptoms and depression.
Also Check: Is Dementia With Lewy Bodies Similar To Parkinson’s
