What Is The Self
Protein in the diet may affect the absorption of levodopa, the major medication used to treat Parkinson’s disease. Fluctuations in the level of levodopa may worsen some behavioral and cognitive symptoms. A low-protein diet may reduce fluctuations in dopamine levels. In some patients with these fluctuations, dietary changes can improve symptoms. However, it is important to ensure that the person is getting adequate calories and other nutrients.
People with Parkinson’s disease should remain as active as possible. Physical therapy helps the person maintain mobility.
In general, people with Parkinson’s disease plus dementia should no longer drive vehicles. Movement problems may prevent quick reactions in hazardous driving situations. Certain medications, especially those given to treat symptoms of dementia, may make them less alert. However, this should be determined on an individual basis and in compliance with the laws of the state.
YOU MAY ALSO LIKE
Slowed Cortical Rhythms On The Eeg Reflect Impaired Vigilance And Underlie Cognitive Fluctuation
As mentioned above the onset of impaired vigilance and fluctuating attention/cognition is particularly characteristic of progression to PDD . In tandem with its role in enhancing processing of salient stimuli, the NBM cholinergic network also plays a key role in the ascending arousal network. The NBM receives noradrenergic afferents from the locus coeruleus and glutamatergic afferents from the reticular formation and acts as an extra-thalamic relay to the cortex and limbic system . Its cholinergic projections can directly desynchronize the neocortical EEG, replacing slow synchronized delta waves with fast beta and gamma waves .
In addition, have shown that patients with PDD with significant cognitive fluctuations demonstrate pseudocyclic patterns of slow wave activity on the EEG in the delta-theta-pre-alpha range , whereas patients with PDD without fluctuations do not . This therefore implies that development of slow EEG rhythms cycling between relatively greater and lesser states of cortical arousal may represent the pathophysiological basis of cognitive fluctuation in PDD. However, further work is needed to establish the mechanisms underlying generation of such rhythms, and why some patients with PDD develop them while others do not.
Onset And Time Course
Mild cognitive impairment was found already at the time of diagnosis in some patients in an incident cohort of PD. There is some evidence that dementia is merely a progression of this early cognitive impairment, while other evidence suggests a different profile in PD-D and non-demented PD patients. Epidemiological studies suggest that dementia usually develops years after the onset of motor symptoms. This could be a methodological bias however, since patients with early dementia may be excluded due to subjects not fulfilling PD criteria.
The onset is insidious. In one prospective study, the mean annual decline on the MMSE during 4 years was 1 point in non-demented and 2.3 points in the PD-D group, the latter figure being similar to the decline observed in patients with AD. A similar rate of decline was reported in another longitudinal study, mean decline in MMSE over 2 years was 4.5, and comparable to that seen in patients with DLB, with a mean decline of 3.9 points.
Read Also: Parkinson’s Disease Average Age Of Death
Improved Clinical Trial Design
Clinical trials for therapies targeting cognition in PD may benefit from recent design improvements. More sensitive outcomes, including computerized cognitive testing and wearables to measure motor and other functions, together with the development of an internationally recognized set of core outcomes, as has been done for idiopathic PD, particularly focused on patients with cognitive impairment and on the effects of specific interventions , will allow the reporting and comparison of research outcomes in a standardized manner. More targeted selection criteria using current diagnostic criteria, and recommended assessments, combined with both biomarkers and genetic risk factors aiming to assign the right person to the right intervention at an early disease stage, as well as biomarkers demonstrating target involvement, will offer opportunities for improved statistical power and cheaper trials.
What Are The Symptoms Of Parkinson Disease
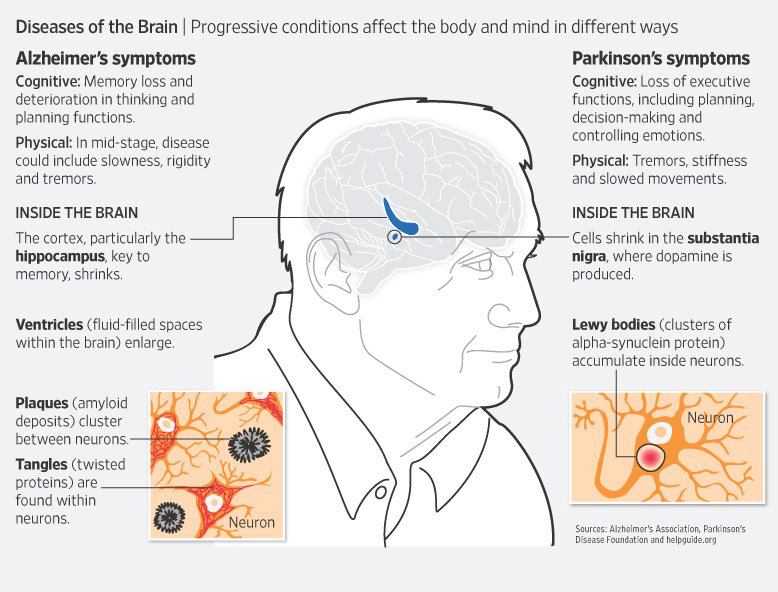
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
Read Also: What Color Is The Ribbon For Parkinson’s
Dysfunction In Cholinergic And Noradrenergic Networks Impairs Bottom
One view of automatic orienting of attention considers it to be mediated by bottom-up or stimulus-driven signals from the NBM in the basal forebrain . This nucleus consists of 90% cholinergic neurons and its widespread projection axons provide the main cholinergic innervation to the entire cortical mantle . Selective activation of the nucleus basalis of Meynert network causes an increase in acetylcholine levels in the cortical target field, which boosts the signal-to-noise ratio for salient stimuli, thereby enhancing the strength of their neural representations . In facilitating this process the NBM effectively amplifies detection of salient stimuli by posterior regions of the fronto-parietal network and ensures their attentional significance . Animal experiments have shown that this NBM-driven cortical signal enhancement is responsible for generating event-related potentials on the EEG . These can be measured on the human EEG as negative deflections occurring 80100 ms after an unpredictable stimulus , and have long been regarded as the electrophysiological correlate of orienting of attention .
Causes And Risk Factors
PD is idiopathic, meaning that a doctor does not know why a person has the condition. However, according to Johns Hopkins Medicine, early-onset Parkinsons disease has links to genetic inheritance from a parent.
Researchers have identified several risk factors that may make a person with Parkinsons disease more likely to experience dementia.
These risk factors include:
- advanced age at time of diagnosis
- experiencing excessive daytime sleepiness
- hallucinations before the onset of other dementia symptoms
- having a specific Parkinsons symptom that causes a person to have difficulty starting to take a step or to halt mid-step while walking
- a history of mild thought impairment
- more severe movement impairment symptoms than most people with Parkinsons disease
However, researchers do not know why some people with Parkinsons disease develop cognitive difficulties as well as movement problems.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
What Causes Parkinson’s Disease Dementia
Doctors don’t yet know the exact cause of Parkinson’s disease dementia, but they think it has to do with an accumulation of a protein called alpha-synuclein. When it builds up in the brain, it can create clumps called “Lewy bodies” in nerve cells, causing them to die.
The death of those cells usually results in the motor symptoms typically associated with Parkinson’s disease. As Parkinson’s disease progresses, those Lewy bodies may eventually damage the brain and cause problems with memory and thinking.
While many people with Parkinson’s disease experience cognitive changes, not all of them will go on to develop dementia. It’s estimated that between 50% and 80% of individuals with the disease eventually develop Parkinson’s disease dementia, usually in the later stages of the disease.
What Are Parkinson’s Disease Dementia Medical Treatment And Medications
There is no specific therapy for dementia in Parkinson’s disease. Although cognitive symptoms initially may appear to respond to drugs that promote dopamine production, the improvement is mild and transient in contrast to the early responses to motor control improvement with medication in patients with Parkinson’s disease.
Parkinson’s disease dementia medications
Various medications are used to treat the movement disorders of Parkinson’s disease, some may exacerbate symptoms related to dementia.
- These include dopamine given in the form of levodopa medications known as dopamine agonists that act on the dopamine receptor and medications that slow down the metabolism of dopamine. They are often used in conjunction with monoamine oxidase inhibitors such as rasagiline. In addition, anticholinergic drugs are sometimes used.
- Unfortunately, these drugs may affect cognitive symptoms and mood disorders.
- The anticholinergic drugs, for example, help balance levels of dopamine and acetylcholine, another neurotransmitter, in the brain. These drugs can improve movement disorders but often make memory loss worse.
The dementia of Parkinson’s disease may respond to drugs used in patients with Alzheimer’s disease. However, these drugs, called cholinesterase inhibitors , lead to only small and temporary improvements in cognition.
Mood disorders and psychoses are usually treated with other medication.
Read Also: Essential Oils For Parkinson Disease
Parkinson’s Disease Dementia Surgery And Gene Therapy
- Great strides have been made in the surgical treatment of Parkinson’s disease. Several different procedures are now available, and they are successful in many patients in relieving movement symptoms. Unfortunately, surgery has no effect on cognitive symptoms. In fact, most people with dementia are not candidates for surgery.
- Gene therapy is in its infancy there are ongoing human and animal trials with various methods to insert genes into neuronal cells to reduce or stop Parkinson’s disease symptoms by causing cells to produce dopamine coded by the newly inserted genes. Early results with the treatment termed ProSavin are encouraging. However, it is not clear if such therapy could prevent or reverse Parkinson’s disease dementia.
Patient And Public Involvement
In the past years, there has been growing attention on the need to include patients, their caregivers and families in all stages of the research process. The increasing contribution of patient and public involvement groups in defining research questions, designing and conducting clinical trials, disseminating outcomes, and shaping research roadmaps reflects the concept of research as a shared effort among all stakeholders. Although in PD research this concept is increasingly being recognized, further involvement of patients and families, also inclusive of diverse patient populations, in research focused on PD-associated cognitive impairment is needed.
Also Check: What Is The Life Expectancy Of Someone With Parkinson’s Disease
The Task Force Composition And Procedure
The MDS Task Force comprised 23 members with different areas of expertise in the field. They were invited to join the Task Force because of their interest and track records in diverse aspects of the disease including epidemiology, clinical aspects, ancillary methods, and pathology, and representing various disciplines to include neurology, geriatric psychiatry, neuropscyhology, and pathology as well as different geographical regions with differing medical traditions. The group was divided into five sub-committees, each in charge of systematically reviewing the literature related to epidemiology, cognitive and neuropsychiatric features, motor and other clinical features, ancillary examinations, and clinico-pathological correlations, based on pre-defined criteria for selection of publications to be included . To exclude cases with Dementia with Lewy Bodies , those papers which used the 1-year rule with regard to the onset of dementia were grouped together and constituted the primary source, whereas those which did not use the 1-year rule or did not indicate if this rule was applied were considered as secondary. Findings and typical features emerging from these reviews, described in detail later, were tabulated and used to describe consensus-based definitions of probable and possible PD-D .
|
|
Where To Get Help
- Your local community health service
- Your local council
- National Dementia Helpline Dementia Australia Tel. 1800 100 500
- Aged Care Assessment Services Tel. 1300 135 090
- My Aged Care Tel. 1800 200 422
- Cognitive Dementia and Memory Service clinics Tel. 1300 135 090
- Carers Victoria Tel. 1800 242 636
- Commonwealth Respite and Carelink Centres Tel 1800 052 222
- Dementia Behaviour Management Advisory Service Tel. 1800 699 799 for 24-hour telephone advice for carers and care workers
Read Also: Parkinson’s Stages Life Expectancy
How Is Age Related To Pdd
Both PD and PDD are more common with increasing age. Most people with PD start having movement symptoms between ages 50 and 85, although some people have shown signs earlier. Up to 80% of people with PD eventually develop dementia. The average time from onset of movement problems to the development of dementia is about 10 years.
Visual Perceptual Dysfunction And Hallucinations: Multiple Network Involvement
Patients with Parkinsons disease exhibit both subtle visuospatial deficits , and visuoperceptive deficits , in some patients from early in the disease . These deficits become more marked and more common with disease progression and show high sensitivity in detecting the transition to PDD . Indeed impairment on the Pentagon Copying Test from the MMSE at baseline has been shown to be predictive of PDD at 5-year follow-up .
Visual hallucinations are also well-recognized in Parkinsons disease and are typically complex, consisting of well-formed people, animals or objects . Although they can be induced by anti-parkinsonian drugs, correlations between use of these agents and presence of hallucinations are actually relatively weak, and instead cognitive impairment has been shown to be the major risk factor, indicating that they are a core symptom of the dementing process . Visual hallucinations generally occur in the latter stages of the disease course with a progressive nature . Their presence is a strong predictor of PDD and indeed the prevalence of hallucinations in PDD is 70% . Although insight is initially maintained in patients with PDD, 81% will lose insight over 3 years , which severely affects quality of life for both patients and caregivers .
Don’t Miss: Life Expectancy With Parkinson Disease
What’s The Difference Between Memory Loss And Parkinson’s Dementia
Alzheimer’s dementia and Parkinson’s disease can both affect a person’s memory, but not in the same way.
Generally speaking, Parkinson’s dementia is not associated with the sort of memory loss that comes with Alzheimer’s, the most common form of dementia. Put differently: It doesn’t typically impact a person’s ability to absorb and store new memories or information the way Alzheimer’s does.
“You can learn , but it’s difficult to retrieve the information that you have in your brain,”Irene Litvan, MD, director of the Movement Disorder Center at the University of California, San Diego, tells Health. “You may not know where the cassette is, but if somebody asks you, ‘Where were you when you lost it?’ You can say, ‘Oh, I was there.'”
RELATED: Here’s How a Doctor Explains the Difference Between Alzheimer’s and Dementia
But that’s not to say Parkinson’s disease dementia doesn’t affect memory at all. On the contrary, some people with Parkinson’s dementia do indeed experience short- and long-term memory loss. They might also forget how to perform simple tasks, like how to run the dishwasher. And since Parkinson’s can affect people in different ways, there’s no way to tell whether someone with the disease will experience memory loss related to dementia.
Parkinsons Disease As Subcortical Dementia
As we mentioned, the dementia associated with Parkinsons disease consists of subcortical dementia this means that it causes alterations in the subcortical area of the brain. Another large group of dementias are cortical dementias, which generally include another well-known dementia, that caused by Alzheimers disease.
But, continuing with subcortical dementias, they include in addition to Parkinsons dementia , Huntingtons dementia and HIV dementia .
All subcortical dementias have characteristic symptoms of motor alterations , slowing down, bradypsychia and decreased motivation.
Bibliographical references:
- Belloch, A., Sandín, B. and Ramos, F. . Manual of psychopathology. Volumes I and II. Madrid: McGraw-Hill.
- Demey, I. and Allegri, R. . Dementia in Parkinsons disease and Lewy body dementia. Argentine Neurological Journal, 33: 3 21.
- Rodríguez-Constenla, I., Cap-López, I., Belles-Lama, P. and Cebrián, I. . Cognitive and neuropsychiatric disorders in Parkinsons disease. Rev Neurol, 50 : S33 S39
Recommended Reading: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinsons disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinsons disease.
The overlap in symptoms between Lewy body dementia and Parkinsons disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinsons disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinsons disease itself isnt fatal, but complications can be.
Research has shown a median survival rate of about
How Is Parkinson Disease Treated
Parkinson disease can’t be cured. But there are different therapies that can help control symptoms. Many of the medicines used to treat Parkinson disease help to offset the loss of the chemical dopamine in the brain. Most of these medicines help manage symptoms quite successfully.
A procedure called deep brain stimulation may also be used to treat Parkinson disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Read Also: Can Parkinson’s Cause Hip Pain
Degeneration Of Neurotransmitter Systems
More widespread dopaminergic deficits in the brain
By definition, all patients with PD have a moderate-to-severe loss of dopaminergic neurons in the nigrostriatal projection pathway. More widespread degeneration of dopaminergic terminals in the striatum particularly denervation of dopaminergic terminals in the associative dorsal caudate nucleus occurs in those with PD-MCI than in those with PD without cognitive impairment . However, in patients with PD-MCI, there is relative preservation of other dopaminergic systems in the brain, whilst those with PDD have a considerable loss of the lateral dopaminergic system to frontal, parietal and temporal cortical regions . In healthy individuals, cortical dopamine modulation can boost working memory as well as visuospatial and attentional processing, and promotes cognitive effort,, suggesting a key role for dopamine in cognitive function.
Fig. 2: Neurotransmitter deficits associated with cognitive decline in PD and DLB.
Noradrenergic locus coeruleus and sympathetic systems
Basal forebrain cholinergic systems
Serotonergic dysfunction is not directly related to cognitive decline
