Tips For Care Partners
- Offer help only when asked.
- Prompt the person for example, instead of asking, Did anyone call? ask, Did Linda call?
- Say the name of the person and make eye contact when speaking to gain and hold attention.
- Put reminder notes and lists in a prominent place.
- Keep things in routine places.
- To ensure medications are taken on time, provide a dispenser, perhaps with a built-in alarm.
- Use photos on cell phone contact entries to prompt face-name association.
- If the person is searching for a word, provide a cue, such as, the word you are looking for probably begins with d.
- Do not finish the sentences of a person who needs more time to put them together.
- When presenting the person with a list of actions, first verbalize them, then write them down.
- Ask questions to moderate the conversation pace and allow catch up and reinforcement.
Page reviewed by Dr. Kathryn P Moore, Movement Disorders neurologist at Duke Health, a Parkinsons Foundation Center of Excellence.
You May Like: Weed Killer That Causes Parkinsons Disease
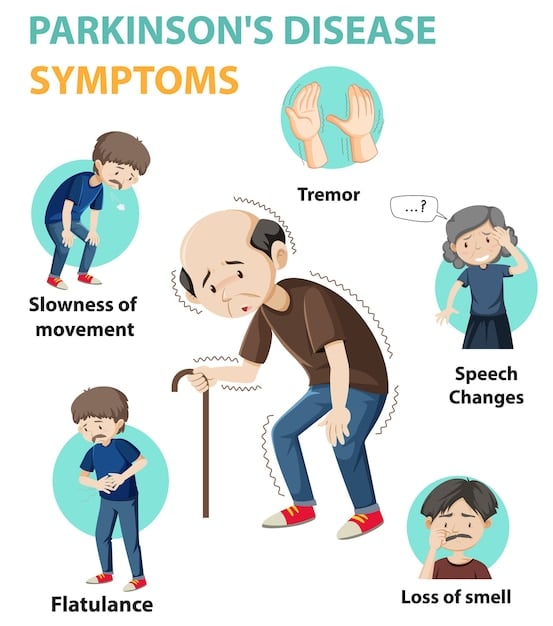
Signs And Symptoms Of Parkinsons Disease
The primary symptoms of Parkinsons disease are:
Tremors or shaking often occur in the hands, fingers, forearms, feet, mouth, or chin. Typically, the tremor appears when your limbs are at rest as opposed to when youre moving. Some people notice that their tremor is exacerbated by stress and excitement.
Slowed movement . You may find that your ability to move freely and spontaneously is reduced or slowed down. Repetitive movements can be especially difficult, causing problems with everyday tasks like buttoning a shirt, brushing your teeth, or cutting food. You may start to walk with short, shuffling steps, or your feet may start to drag.
Rigidity, or muscle stiffness, may occur in any part of your body . This can limit your range of motion and cause muscle pain that gets worse when you move.
Poor balance, or the tendency to be unstable when standing upright, is one of the most important signs of Parkinsons. It happens because of the loss of reflexes needed for maintaining posture. Some people develop a tendency to sway backwards when standing or turning, which can result in backwards falls.
Dementia Outcomes According To Baseline Motor Features
Among motor variables , the proportion of gait involvement at baseline , falls , and freezing predicted dementia. Poor performance on the Purdue Pegboard Test and alternate tap test , but not the UPDRS predicted dementia. Patients developing dementia were more likely to report bilateral onset of motor symptoms . There was no association between dementia status and PD subtype, although the dementia-converted group had slightly more patients with akinetic-rigid Schiess scores than the group without dementia . Baseline UPDRS part III scores, total UPDRS scores, Timed Up and Go, Hoehn and Yahr stage, and axial-limb ratio were not predictive of dementia status.
Don’t Miss: How To Help Someone With Parkinson’s Dementia
What Happens In Pdd
People with PDD may have trouble focusing, remembering things or making sound judgments. They may develop depression, anxiety or irritability. They may also hallucinate and see people, objects or animals that are not there. Sleep disturbances are common in PDD and can include difficulties with sleep/wake cycle or REM behavior disorder, which involves acting out dreams.
PDD is a disease that changes with time. A person with PDD can live many years with the disease. Research suggests that a person with PDD may live an average of 57 years with the disease, although this can vary from person to person.
What To Do If Rbd Is Suspected
While REM sleep behavior disorder may occur in conjunction with, or as a predecessor to, certain neurological disorders such as Parkinsons disease, it can also result from medication usage.
If you or a loved one is concerned about RBD, contact a movement disorder neurologist or sleep disorders specialist, such as the experts available at Michigan Medicine, for an evaluation.
ByJoe Brownstein30 May 2013
A rare sleep disorder that causes people to punch and kick others during sleep may have some of the same risk factors as Parkinsons disease, and could give researchers clues to predicting Parkinsons many years before it surfaces, a new study suggests.
The results revealed a number of factors linked with an increased risk of REM sleep behavior disorder , including smoking, working on a farm, past head injuries and pesticide exposure.
A better understanding of how these factors might be at work in both REM sleep Behavior Disorder and Parkinsons could lead to a way of diagnosing Parkinsons and detecting it very early, said study author Dr. Ronald Postuma, a neurologist at McGill University in Montreal.
Patients with RBD typically make sounds or move during REM sleep. The condition has been linked with some forms of dementia and Parkinsons disease, with one study of 93 RBD patients showing that more than half developed a neurodegenerative disease over a 12-year period.
Violent sleep
The link between neurological diseases and sleep
MyHealth_MHND.Were also on & .
You May Like: Does Michael J Fox Have Parkinson’s
How Can We Manage Hallucinations
It may not be necessary to treat all hallucinations of a person with PDD. Hallucinations are often harmless, and it is okay to allow them to happen, as long as they are not disruptive or upsetting to the person or surroundings. Sometimes, recognizing the hallucination and then switching the topic might be an efficient way of handling frustrations that occur because of a hallucination. If hallucinations need medical treatment, your provider may be able to discuss and suggest some options. However, many of the medications used to treat hallucinations may make movement symptoms worse.
Managing Psychotic Symptoms In Parkinsons Disease
Any psychotic symptoms, such as hallucinations, delusions, or paranoia, that are experienced by a person with PD should be reported to a doctor, even if the symptoms are not bothersome. Managing these symptoms may include reducing or withdrawing the use of PD medications that may be causing the symptoms or adding an antipsychotic medication.1,2
You May Like: Can A Blood Test Detect Parkinsons
Don’t Miss: What Metal Is Linked To Parkinson’s
Vascular Dementia And Vascular Cognitive Impairment
The term vascular dementia has been problematic for the same reasons as the term dementia, and the term vascular cognitive impairment is preferable. Impairment of episodic memory is less prominent in vascular dementia than in Alzheimers disease, particularly in patients with small vessel disease in whom impairment of executive function and cognitive slowing are more common. White matter changes indicative of small vessel disease and lacunar infarcts are commonly seen on MRI scans in elderly individuals and are particularly common in association with Alzheimers disease, often indicating mixed dementia. In younger patients there is usually, but not invariably, an association with vascular risk factors but intensive investigation might identify rarer causes, including mitochondrial disease or cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy . Amyloid angiopathy is important to recognise as some patients might have an inflammatory component that could be responsive to steroids lobar microhaemorrhages seen on T2*-weighted MRI might help detection. APP duplications are commonly associated with a prominent amyloid angiopathy with cerebral haemorrhages and seizures. Treatable causes such as cerebral vasculitis are also more commonly found in younger patients than in the elderly.
Pd Dementia And Safety Concerns
Safety issues should be considered and monitored from the time of diagnosis. As PDD progresses, ensure that your loved one is not left alone and try to:
- Evaluate driving privileges before safety is a concern. Your doctor can make a driving evaluation referral.
- Work out legal and financial issues and safeguard finances. People with dementia are at greater risk of falling victim to scams and fraud.
- Minimize prescription risks. Confirm with the doctor the medication names and doses of the person with PD. If the person is in dementias early stages and capable, fill up their weekly pill box together and monitor use.
- Look into medical alert systems. These systems can be critical in the event of a fall or if your loved one wanders outside of the home. Many types of systems are available, from bracelets and pendants to smartwatches with fall detection and one-button connections to 911.
- Evaluate gun safety. If your loved one owns a firearm or has one in the home, consider bringing it up with their doctor and taking additional safety precautions.
Don’t Miss: Is There A Definitive Test For Parkinson’s Disease
What Can I Expect If A Loved One Or I Have Lewy Body Dementia
Each persons experience with Lewy body dementia is unique to them. How slowly or quickly the disease progresses is impossible to know, but may be influenced by your general health and any existing conditions you may have.
Because LBD is a progressive disease, difficulties with mind and body functions get worse over time. Currently, theres no known way to stop the progression of the disease.
However, theres always hope. Research on dementia with Lewy bodies, Alzheimers disease and Parkinsons disease with dementia are ongoing. New medications are being developed and new treatment approaches are being investigated.
You May Like: Delusions In Parkinsons Disease
Wait So What Is Parkinsonism
Parkinsonism refers to the motor symptoms that are typically associated with PD, such as tremors, stiffness, and walking/balance problems. Both PD and LBD are forms of Parkinsonism, meaning that PD patients and LBD patients may experience these motor symptoms.2 Because the Parkinsonism motor symptoms of PD and LBD can be very similar, it can be difficult to differentiate between the two conditions.
Dont Miss: Similar To Parkinsons
Don’t Miss: Is Red Wine Good For Parkinson’s Disease
Tip : Make It A Priority To Be Socially Engaged
The more socially active you are, the more you connect face-to-face with others, the stronger your memory and cognition is likely to be. You dont need to be a social butterfly or the life of the party, but you do need to regularly connect with people who care about you.
Connecting with others is the most effective means of relieving stress which left unchecked can exacerbate symptoms of Parkinson’s disease. Staying socially engaged also stimulates immune function that may slow the progress of disease. While many of us become more isolated as we get older, its never too late to meet others and develop new friendships.
Tips for meeting new people
Parkinsons Sleep Problems: Diagnosis And Treatment
Parkinsons disease is chronic and progressive, meaning it tends to get worse over time. However, there are treatment options that can help manage symptoms and allow patients to get more restful sleep.
The simplest way to start sleeping better with Parkinsons disease is by adopting healthy sleep habits. Sleep hygiene tips for Parkinsons disease sufferers include:
- Sticking to regular bedtimes
- Following a consistent bedtime routine with soothing activities such as listening to music or reading a calming book
- Getting regular exercise, preferably early in the day
- Getting adequate exposure to light, whether outdoors or through light therapy
- Avoiding long naps and naps late in the day
- Creating a cool, dark, and comfortable sleeping environment
- Restricting bedtime activities to sex and sleep only
- Turning off screens an hour before bedtime
- Reducing liquid intake before bedtime
- Avoiding caffeine, alcohol, and tobacco
- Eating a healthy diet and avoiding large meals at night
Light therapy, exercise, and deep brain stimulation have been successfully used to improve overall sleep quality and to treat specific conditions, such as REM sleep behavior disorder, in patients with Parkinsons disease. Cognitive behavioral therapy for insomnia has proven effective at reducing insomnia in healthy adults, although further research is needed on the effects of CBT in patients with Parkinsons disease.
- Was this article helpful?
Recommended Reading: Does Bill Clinton Have Parkinsons
Secondary Symptoms Of Parkinsons Disease
In addition to the major symptoms of Parkinsons, there are many secondary motor symptoms associated with the disease. Again, not everyone with Parkinsons will necessarily develop all or even any of these symptoms.
- Freezing when walking, usually occurring when taking the first step.
- Small, cramped handwriting that gets worse the more you write.
- A less expressive face. People may comment that you look serious or mad. You may have a blank stare or blink less often.
- Speech may become slow, whispery, or slurred.
Not Everyone With Parkinsons Will Develop Dementia
Despite the fact that the pathology of Parkinsons disease can trigger the development of different types of dementia, not everyone with Parkinsons will develop dementia. About 30 percent of people with Parkinsons will actually not develop dementia at all, as stated by the National Parkinson Foundation.
However, the vast majority of people with Parkinsons may experience some form of cognitive impairment over time, the foundation says.
Also Check: Patch For Parkinsons Disease
Don’t Miss: What Is Stage 5 Parkinson’s
Theres No Cure For The Diseases But Some Therapies May Help
Certain drugs, like cholinesterase inhibitors and antipsychotic medications, are prescribed as treatment for people with Parkinsons and dementia. And lifestyle changesfrom improved diet, sleep, exercise and socializinghave been shown to have beneficial effects on patients with these diseases.
Oguh noted she hopes that improved treatments that will help some of the emotional and behavioral problems in these patients will be on the horizon soon.
Im hoping that with the new advances in medication, well be able to control better, Oguh said. I believe there will be better medication to improve cognition in patients, and that that will be seen in the next five to 10 years.
Parkinsons And Lewy Body Disease
Lewy body disease occurs when there is an abnormal build-up of a protein called alphasynuclein in the brain. Depending on where the proteins accumulate, Lewy body disease can lead to impairments in movement, thinking and behaviour.
Lewy body disease includes three overlapping disorders:
- Dementia with Lewy bodies
- Parkinsons disease dementia
This overlap results in the disease being called a spectrum disease.
In people with Parkinsons a large number of Lewy bodies appear in an area of the brain known as the substantia nigra. This area of the brain is responsible for movement, so the Lewy bodies are likely to cause impairments in movement.
Some people may go on to develop dementia with Lewy bodies. In this form of the disease, the clumps of protein occur in the cortex . This part of the brain is responsible for many cognitive processes, so the Lewy bodies are likely to result in cognitive impairments like those described under the heading above. It can result in symptoms similar to those seen in Alzheimers.
You May Like: What Are Lewy Bodies In Parkinson’s Disease
Parkinsons Disease: Symptoms Stages And Treatment
Parkinsons disease usually begins after age 60, gradually progressing over the years. Some people can have early-onset Parkinsons disease, starting in their 30s or 40s. It is primarily a movement disorder characterized by resting tremors and slowness and stiffness of movement.
In the late stages of the disease, Parkinsons dementia can develop. But most people who have Parkinsons disease do not develop dementia as a part of the condition.
Inborn Errors Of Metabolism
A handful of inborn errors of metabolism may cause visual hallucinations. While these are quite rare, they are nonetheless important to consider because patients with inborn errors of metabolism may present with hallucinations at a time when their disease is treatable and when serious neurologic damage has not yet occurred. Specific inborn errors of metabolism that may present with visual hallucinations include homocysteine remethylation defects, urea cycle defects, GM2 gangliosidosis, Neimann-Pick disease type C, and -mannosidosis.
You May Like: Parkinson’s Disease Typically Causes
Diagnosis: Parkinson’s Dementia Or Dementia With Lewy Bodies
During assessment, a specialist may look at when the dementia symptoms first appeared before reaching a diagnosis of Parkinson’s dementia or dementia with Lewy bodies.
If there have been motor symptoms for at least one year before dementia symptoms occur, specialists will often give a diagnosis of Parkinson’s dementia.
If dementia symptoms occur before or at the same time as motor symptoms, specialists will usually give a diagnosis of dementia with Lewy bodies.
However, it should be noted that in some cases of dementia with Lewy bodies, no motor symptoms develop at all.
Theres no single test – diagnosis is made through several different assessments, usually starting with an appointment with your GP or Parkinson’s nurse.
Some people find it helps to go to the appointment with someone who knows them well, who can give the GP or Parkinson’s nurse information about changes they’ve noticed.
Your GP can discuss your symptoms with you and carry out a physical examination, including blood and urine tests, to rule out other potential causes of the symptoms .
Your GP may also review your medication, in case your symptoms are side effects.
If your GP thinks you have dementia, they can refer you to a specialist, such as a neurologist, psychiatrist or geriatrician.
You might be referred to a memory clinic or memory service. In some areas of the country, you can refer yourself to these services.
But if you feel you need to see the specialist again, you can ask to be referred back.
Panel : Dementia Plus Syndromes And Associated Diseasessystemic Features
Cataracts
Myotonic dystrophy, cerebrotendinous xanthomatosis, mitochondrial disorders, familial Danish dementia
Splenomegaly
Niemann-Pick disease type C, Gauchers disease
Tendon xanthomas
Fabrys disease, Lesch-Nyhan syndrome, mitochondrial disorders
Hepatic dysfunction
Wilsons disease, Gauchers disease, mitochondrial disorders
Respiratory failure
Frontotemporal lobar degeneration and motor neuron disease, Perry syndrome, mitochondrial disease , anti-NMDA receptor-mediated limbic encephalitis
Gastrointestinal dysfunction
Coeliac disease, Whipples disease, porphyria
Anaemia
Vitamin B12 deficiency, neuroacanthocytosis , Wilsons disease, Gauchers disease
Skin lesions
Behcets disease, systemic vasculitides and connective tissue disease, Fabrys disease
Metabolic or infectious crises
Vanishing white matter disease, Alexanders disease, ornithine transcarbamylase deficiency, alpha mannosidosis, porphyria
Hyponatraemia
VGKC limbic encephalitis
The dementia plus syndromes describe patterns of cognitive impairment plus additional neurological or systemic features that aid investigation and diagnosis of the underlying disease process. This list cannot be comprehensive. Note that vascular disease, structural disorders, and neoplastic disease can be associated with a wide range of presentations. POLG=polymerase , gamma. VGKC=voltage-gated potassium channel.
Neuropsychological signatures of young-onset dementia
Recommended Reading: Shaking Disease Similar To Parkinson’s
