Tip : Make Other Healthy Lifestyle Choices
In addition to regular exercise, eating a healthy diet, and interacting with others, there are plenty of other steps you can take to manage Parkinsons symptoms and lower your risk for dementia.
1. Seek mental stimulation. By continuing to learn new things and challenge your brain, you can strengthen your cognitive skills and stay mentally sharp. Another great way to improve brain function is to learn a new skill, whether its a musical instrument, a foreign language, a new computer program, or a new game or sport. Classes at community centers or colleges can help you to tackle new subjects.
2. Improve the quality of your sleep.Good sleep is important for flushing out toxins and protecting your brain. Most adults need 7 to 9 hours of quality sleep. Establish a regular sleep schedule, create relaxing bedtime rituals such as taking a bath or doing some light stretches, and turn off all screens at least one hour before sleep.
3. Manage stress. Unchecked stress takes a heavy toll on the brain, shrinking a key memory area, hampering nerve cell growth, and can make many Parkinsons symptoms worse. Overwhelming stress may even increase your risk for developing dementia. As well as connecting face-to-face with others, exercise and relaxation techniques such as meditation or deep breathing can help you lower your stress levels.
To learn more about putting these strategies into action, see Preventing Alzheimers Disease.
Don’t ignore depression
Is The Dementia Caused By Parkinsons Or Something Else
Indications that dementia may be caused by something other than Parkinsons disease include agitation, delusions , and language difficulties. If the onset of cognitive symptoms is sudden, theyre more likely due to something other than Parkinsons diseaseeven reversible causes such as infection, a vitamin B12 deficiency, or an underactive thyroid gland.
Depression can mimic dementia by causing similar symptoms such as apathy, memory problems, and concentration difficulties. Since depression is very common in Parkinsons patients, its important to recognize the signs and symptoms of depression in older adults.
Parkinson’s disease dementia vs. other dementias
Other types of dementia that can be commonly mistaken for Parkinsons disease dementia include:
Lewy Body Dementia is characterized by fluctuations in alertness and attention, recurrent visual hallucinations, and Parkinsonian motor symptoms like rigidity and the loss of spontaneous movement. In this disorder, cognitive problems such as hallucinations tend to occur much earlier in the course of the disease and often precede difficulties with walking and motor control.
Alzheimers disease and Parkinsons disease are both common in the elderly, especially in those over 85. Patients with Parkinsons who develop dementia may even develop Alzheimers dementia as well. Therefore, its important to be aware of the signs of Alzheimers Disease and how its treated.
Hidden Away In Some Of The Oldest Creatures On Earth Lives A Naturally Occurring Compound That May Be Key To Tackling Dementia In Parkinsons We Discover More And Find Out About The Latest Parkinsons Virtual Biotech Project A Clinical Trial That Plans To Start Next Year
Why are fish so good at fighting off infection? Its the question that just might have started the ball rolling on a new drug treatment for Parkinsons-related dementia.
In 1993, Dr Michael Zasloff, discovered the answer to this fishy conundrum in the liver of dogfish sharks a naturally occurring steroid which the team of researchers named squalamine.
Squalamine has anti-microbial properties against both bacteria and viruses. It has shown promise in clinical trials for cancer but perhaps its most interesting ability relates to its interaction with problematic proteins alpha-synuclein, beta-amyloid, tau and TDP-43.
Read Also: Dbs For Parkinson’s Disease
Tips For Communicating With A Person With Pdd
PD-related mood and motor changes can impact communication cognitive changes and Parkinsons disease dementia can further these difficulties.
- Stay calm and be patient. It is not usually helpful to try to reason or argue with someone experiencing a hallucination or delusion. If the person is frightened by the hallucination or delusion, try to redirect their attention to something else.
- Acknowledging what the person is seeing, even if you do not see it, can reduce stress.
- Speak slowly and at eye level. Communicate in simple sentences.
- Ask one question at a time and wait for an answer.
- Limit distractions. Turn off the TV or radio before asking a person with PDD to do something.
- Consider causes behind disruptive behavior. Can your loved one be hungry, thirsty, tired, in pain, frustrated, lonely or bored?
- If the person is stuck on an idea, try agreeing with them, then changing the subject.
- Its okay to use humor to diffuse stressful situations but avoid negative humor or sarcasm these can be misunderstood.
Page reviewed by Dr. Chauncey Spears, Clinical Assistant Professor and Dr. Sydney M. Spagna, Clinical Fellow at the University of Michigan.
Epidemiology Of Dementia And Parkinson’s Disease
Dementia and PD are both diagnosed frequently and increase mortality . Perhaps dementia is perceived more so as a memory problem and a disease of old age, but the incidence of dementia and PD in younger age is similar. In the Netherlands, for dementia, the incidence per 1,000 person-years is 0.4 among those aged 6064 , and for PD, it is 0.3 . Dementia incidence patterns, however, show a much steeper increase with age mounting to 27 per 1,000 person-years for those 85 and over, compared to 4 for PD over 85. In view of similar mortality , therefore, the prevalence of dementia in the general population is much higher than prevalence of PD . However, adjusted for age and other factors, 6-year mortality in PD is higher than in Alzheimer’s dementia . Age adjustment is relevant also as it shows that comorbid disease may be equally prevalent for Alzheimer’sa main type of dementiaand PD across the same age groups .
Don’t Miss: How Does Sinemet Help With Parkinson’s
Parkinsons Dementia Vs Alzheimers Dementia
According to experts, Parkinsons dementia can cause impaired physical activity and impacts motor skills. Two neurotransmitters called dopamine and serotonin tend to be damaged by Parkinsons.
In addition to causing issues with movement and coordination, this form of dementia can also cause a slower thought process and memory problems. This is usually less pronounced however, until the later stages of the disease.
With Alzheimers, two types of proteins in the brain, tangles and plaques , accumulate and kill brain cells. This Alzheimers-induced dementia affects memory, clear thinking, language skills, and orientation. It reduces comprehension, learning capacity, and judgement. Storing new information and memory retrieval are impacted more than motor skills.
Distinguishing between these neurodegenerative conditions is important to determine the best treatment approach. Medications for one of condition might create problems when given to a patient with the other condition.
Wondering how to support a loved ones goal of being able to age at home? Were here to help. Whether its for one month or ten years, our caregivers can help your loved one live the life they want at home. Call a Care Advisor today at or and learn more about how we can support your needs.
Also Check: Yopd Life Expectancy
Dementia In Parkinsons Disease
Dementia is an umbrella term that is defined by a decline in memory and cognitive, or thinking, skills to a level that interferes with normal function. It is normal for older people to have more problems remembering names and faces than they had before, but this does not interfere with normal activities in most cases. People with dementia will misplace things much more than they used to. They will forget appointments, get lost driving, even in relatively familiar places. They may wake up during the night and think they need to go to work even though they retired years ago. They may ask to go home even though they are at home, mistake their wife for their mother, and sometimes get agitated when they are certain there is something wrong and no one else takes this seriously. Patients with dementia often cause problems because they wake up at night and try to go outside, or they may try to cook something and then forget theyve left the burner or oven on. More commonly they ask the same question repeatedly, driving their family crazy.
Recommended Reading: Large 10 Parkinson’s Exercises
How Is Age Related To Pdd
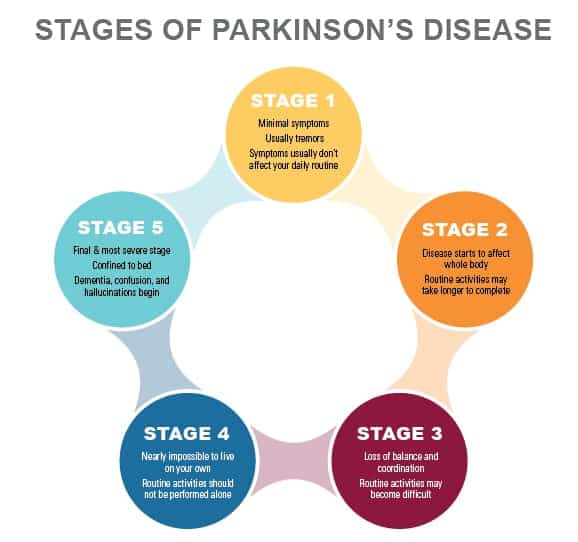
Both PD and PDD are more common with increasing age. Most people with PD start having movement symptoms between ages 50 and 85, although some people have shown signs earlier. Up to 80% of people with PD eventually develop dementia. The average time from onset of movement problems to the development of dementia is about 10 years.
Dementia Risk In Parkinsons Disease Is Associated With Interhemispheric Connectivity Loss And Determined By Regional Gene Expression
Dementia risk in PD is associated with interhemispheric structural connectivity loss.
-
Connection type rather than length alone determines selective vulnerability of connections.
-
Specific regional gene expression patterns and cell types are associated with interhemispheric connection loss.
Also Check: How To Support Someone With Parkinson’s Disease
Symptoms And Mortality Of Parkinsons Disease With Dementia
Parkinsons disease turns into Parkinsons disease with dementia at least one year after the initial diagnosis, well after those PD symptoms above become apparent. As PD becomes PDD, the following symptoms start to appear: Anxiety, depression, and irritability Delusions Paranoia Inability to process visual information Hallucinations Memory loss
While people with Parkinsons have only slightly higher mortality rates than people without the disease, mortality rates significantly increase for people with PDD. In other words, someone with PDD is more likely to die sooner than someone who has Parkinsons without dementia. The disease is not fatalyou cannot die from Parkinsonsbut mortality rates increase because falls and accidents become more likely. Add dementia and it becomes dangerous, making caregiving, or finding the right assisted living or memory care home , more important.
The following are some of the most common indications and symptoms of Parkinsons disease dementia:
- Memory and attention problems
- Visual hallucinations are a common occurrence.
It is critical to have yourself or a loved one checked out if you detect any of the following signs and symptoms. But do not make hasty judgments. Anxiety, a lack of desire, and slower thinking are common cognitive impairments in people with Parkinsons disease. These signs do not always indicate dementia.
Tip : Make It A Priority To Be Socially Engaged
The more socially active you are, the more you connect face-to-face with others, the stronger your memory and cognition is likely to be. You dont need to be a social butterfly or the life of the party, but you do need to regularly connect with people who care about you.
Connecting with others is the most effective means of relieving stress which left unchecked can exacerbate symptoms of Parkinsons disease. Staying socially engaged also stimulates immune function that may slow the progress of disease. While many of us become more isolated as we get older, its never too late to meet others and develop new friendships.
Tips for meeting new people
- Join a club or social group
- Visit your local community center or senior center
- Take group classes
- Reach out over the phone or email
- Connect to others via social media
- Get to know your neighbors
- Make a weekly date with friends
Don’t Miss: Stage Three Parkinson’s Disease
What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
What Is Lewy Body Dementia
Lewy body dementia is not a single disorder but rather a spectrum of closely-related disorders involving disturbances of cognition, behavior, sleep, movement and autonomic function.
In these progressive disorders, Lewy bodies build up in the brain. Lewy bodies in the brain stem cause a disruption in the production of chemical messengers called dopamine. Too little dopamine can cause parkinsonism, a clinical syndrome thats characterized by tremor, bradykinesia , rigidity and postural instability. Parkinsonism can be caused by Parkinsons disease itself as well as by other underlying neurological conditions such as LBD. These Lewy bodies are also found throughout other areas of the brain, including the cerebral cortex. The neurotransmitter acetylcholine is also depleted, causing disruption of perception, thinking and behavior.
A German neurologist, Friederich H. Lewy, first discovered the abnormal protein deposits in the early 1900s as he was conducting research on Parkinsons disease.
Recommended Reading: Does Parkinson’s Disease Cause Pain
Signs And Symptoms Of Pdd
Common signs and symptoms of Parkinsons disease dementia include:
- Poor memory and concentration
- Visual hallucinations
If youve noticed some of the above signs and symptoms in yourself or a loved one, its important to get them checked out. But dont jump to conclusions. People with Parkinsons often experience cognitive changes such as anxiety, lack of motivation, and slowed thinking. These symptoms do not automatically mean dementia.
Lewy Bodies And Parkinsons Disease
A person with Parkinsons disease may develop dementia and have problems with reasoning and thinking. Lewy bodies are a feature of several brain disorders, including Parkinsons disease and Alzheimers disease, and they may cause rigid muscles and problems with movement and posture.
Research suggests that the similarity of the symptoms of Parkinsons disease and Lewy body dementia may be indicative of a shared link to how the brain processes alpha-synuclein.
It is not possible to test for the presence of Lewy bodies, so researchers must try to determine their effects by carrying out postmortem studies.
There is currently no cure for dementia. However, medication can alleviate the symptoms, while a team of medical professionals and therapists may help a person develop strategies to manage their daily activities.
Don’t Miss: How Fast Parkinson’s Progression
Conceptualization Of The Diseases Needs And Interventions
Both dementia and PD are incurable and progressive diseases with often complex problems and needs, for which tailored interventions are available . For dementia, experts agree that recognizing its eventual terminal nature is the basis for anticipating future problems and an impetus to the provision of adequate palliative care . Some advocate advanced dementia to be a terminal disease to support eligibility for palliative care. However, as about half of dementia patients never reach an advanced stage , it may be a late trigger to initiate palliative care. There is no consensus, however, at which stage palliative care in dementia should start .
Table 2. Conceptualization of the disease, needs of patients and family caregivers, and interventions.
For PD there are no curative treatments either, but the success of dopaminergic replacement therapy and deep brain stimulation has enabled the majority of patients to live independently with a relatively low symptom burden for the first 10 years after diagnosis-when they live up to a decade . This may contribute to PD generally not being recognized as an illness for which a palliative approach may be helpful . A US patient and caregivers council recommends palliative care to be available from diagnosis of PD . This is also the ideal of the European Parkinson’s Disease Association although they emphasize that when to start palliative care is an individual decision.
Dysfunction In Cholinergic And Noradrenergic Networks Impairs Bottom
One view of automatic orienting of attention considers it to be mediated by bottom-up or stimulus-driven signals from the NBM in the basal forebrain . This nucleus consists of 90% cholinergic neurons and its widespread projection axons provide the main cholinergic innervation to the entire cortical mantle . Selective activation of the nucleus basalis of Meynert network causes an increase in acetylcholine levels in the cortical target field, which boosts the signal-to-noise ratio for salient stimuli, thereby enhancing the strength of their neural representations . In facilitating this process the NBM effectively amplifies detection of salient stimuli by posterior regions of the fronto-parietal network and ensures their attentional significance . Animal experiments have shown that this NBM-driven cortical signal enhancement is responsible for generating event-related potentials on the EEG . These can be measured on the human EEG as negative deflections occurring 80100 ms after an unpredictable stimulus , and have long been regarded as the electrophysiological correlate of orienting of attention .
Also Check: Advice For Parkinson’s Patients
What Is Aggressive Parkinsons Disease
As written above, Parkinsons dementia aggression is that form of Parkinsons which makes the patient exhibit aggressive behavior. They vent out their aggression either verbally or physically, in the various forms that have been written above. Besides verbal and physical outbursts, PD Dementia patients are also prone to hallucinating caused by the medication administered. Hallucinations in PD Dementia patients primarily occur because of the effects of dopaminergic agents for motor symptoms.
Loss of dopamine neurons in the ventral tegmental area is one of the likeliest of all neuropathological causes as changes in serotonin and norepinephrine systems are not. For the uninitiated, the ventral tegmental area is the origin of the mesolimbic dopaminergic projection. Plenty of studies have gone into analyzing the cause behind the aggression in PD Dementia patients. Depression in PD Dementia patients has been identified due to changes in the medial frontal cortex and the anterior cingulate. Akinetic-rigid variants have been found in patients showing signs of major depression.
The Problem With Tangled Up Proteins
When it comes to neurodegenerative conditions, there seems to be a common issue proteins that become tangled up inside nerve cells and become toxic.
- In Parkinsons, the culprit is alpha-synuclein
- In Alzheimers, both tau and beta-amyloid get tangled up
- Tau also plays a role in progressive supranuclear palsy
- The protein TDP-43 has been seen to accumulate in motor neurone disease and certain types of dementia
- And in Huntingtons, the protein huntingtin builds up in clumps.
While there is still much we dont know about how and why they form, there is a general consensus that these clumps, tangles, plaques and aggregates can be damaging and are likely at the route of all these conditions. There is also much we dont know about the proteins involved in forming these clumps but researchers are uncovering more about the role they play. For instance, it is now believed that alpha-synuclein can be produced by nerve cells in the gut in response to infection, and protects us by calling in the immune system to help defend us.
Perhaps the complexity of the problem with protein tangles underscores why we lack treatments that slow the progression of all these conditions. But there is also hope that identifying drugs that slow or stop the proteins becoming tangled and toxic could be key to halting progression.
You May Like: Is There A Test To Determine Parkinson’s Disease
