Balance Dysfunction In Parkinsons Disease
Antonio Currà
1Neurology and Neurophysiopathology, Sandro Pertini Hospital, Via Monti Tiburtini 385, 00157 Rome, Italy
2Institute of Neurology, Department of Neurosciences, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health , Largo Daneo 3, University of Genova, 16132 Genova, Italy
3Academic Neurology Unit, A. Fiorini Hospital and Department of Medical-Surgical Sciences and Biotechnologies, Sapienza University of Rome, Polo Pontino, Via Firenze, 04019 Terracina, Italy
4Neurosurgery Unit, Policlinico Umberto I, Department of Neurology and Psychiatry, Sapienza University of Rome, Via del Policlinico, 00161 Roma, Italy
5Neurology Unit, Policlinico Umberto I, Department of Neurology and Otolaryngology, Sapienza University of Rome, Via dellUniversità 30, 00185 Roma, Italy
6Academic Neurorehabilitation Unit, ICOT and Department of Medical-Surgical Sciences and Biotechnologies, Sapienza University of Rome, Polo Pontino, Via F. Faggiana 34, 04100 Latina, Italy
7INM Neuromed IRCCS, Via Atinense 18, 86077 Pozzilli, Italy
Abstract
1. Introduction
In the late stages of the disease, when the postural reactions begin to be impaired or inadequate , patients manifest abnormal dynamic postural control . This is a highly disabling symptom because it is poorly controlled by dopaminergic therapy; if present early in the disease, a form of atypical Parkinsonism should be suspected .
2. Sensory Organization: Visual, Vestibular, and Somatosensory Inputs
6. Conclusions
Directing Focus To Stay One Step Ahead
The subthemes focused attention; internal dialogue and anticipating and planning group together to form this theme. Participants described having to place an increasing amount of conscious effort into dealing with the present moment and, more specifically, performing activities without falling. They were more careful and aware of challenging situations and had begun to implement a sort of strategic carefulness, which could entail staying seated on the bus until it had come to a full stop or walking on the middle of the train platform instead of near the edge.
Yes exactly, and at the same time, if I walk on a path and meet someone I let them pass in a way that I do not have to step aside, because then I would be afraid that I might fall.
While in the moment of performing a certain balance-demanding task, such as walking, participants described having to concentrate on this 1 task with undivided attention.
Yes I do that, when I walk from the kitchen counter to the sofa I do that. But the thing is that I concentrate on just that one thing that I am doing right then, and then when I sit down, then I relax a little. But I cant relax while Im walking.
The subtheme internal dialogue concerns how participants pep-talked themselves when faced with environmental demands such as icy streets, stairs, or an oncoming crowd of people. It also entails how they communicated with their body to prepare for and thereafter perform the action in a goal-directed manner.
Equipment And Walking Aids
You might find that equipment can help you to walk, such as a walking stick or a rollator .
Before you start using a walking aid, it’s very important to get advice from a physiotherapist. Some walking aids aren’t recommended for people with Parkinsons as they can affect your walking pattern and make you more likely to fall. But, the correct walking aid can increase your confidence and help you to lift your feet better.
Don’t Miss: What Is One Of The Main Symptoms Of Parkinson’s Disease
Impaired Kinesthesia Affects Sensory Integration
Central sensory integration involves active interpretation of visual, vestibular and somatosensory inputs for orientation of the body in space. When sensory information is unavailable or conflicting, a process of sensory reweighting occurs so the nervous system ignores ambiguous, unhelpful information and relies more on useful sensory information. For example, somatosensory input normally contributes 70% to postural stability when standing on a firm surface with eyes open but, but vestibular input contributes 100% to postural stability when standing on an unstable surface with eyes closed . Patients with advanced PD are often unable to stand on an unstable surface with eye closed, although their vestibular system is usually normal . This finding suggests that patients with PD may take more time for the sensory reweighting process than healthy people. Another problem in sensory orientation is that the patients with PD have impaired use of proprioception for a kinesthetic body map. For example, patients with PD have difficulty perceiving small changes in surface inclination, i.e., impaired kinesthesia . Consequently, a poor sense of kinesthesia in PD is compensated by an over-reliance on vision for postural orientation.
Medicines For Parkinson’s Disease

Medicines prescribed for Parkinson’s include:
- Drugs that increase the level of dopamine in the brain
- Drugs that affect other brain chemicals in the body
- Drugs that help control nonmotor symptoms
The main therapy for Parkinson’s is levodopa, also called L-dopa. Nerve cells use levodopa to make dopamine to replenish the brain’s dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapysuch as nausea, vomiting, low blood pressure, and restlessnessand reduces the amount of levodopa needed to improve symptoms.
People with Parkinson’s should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, such as being unable to move or having difficulty breathing.
Other medicines used to treat Parkinsons symptoms include:
- Dopamine agonists to mimic the role of dopamine in the brain
- MAO-B inhibitors to slow down an enzyme that breaks down dopamine in the brain
- COMT inhibitors to help break down dopamine
- Amantadine, an old antiviral drug, to reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
Read Also: Can A Neurologist Diagnose Parkinson’s
Exercises To Improve Gait
Physical therapy, along with other exercises to help you practice walking strategies, can help reduce Parkinsonian gait. Some of these exercises can be done at home. Consult a physical therapist to help you figure out which exercises will be the most beneficial for you. Potential exercises include:
Walking Freezing And Falling
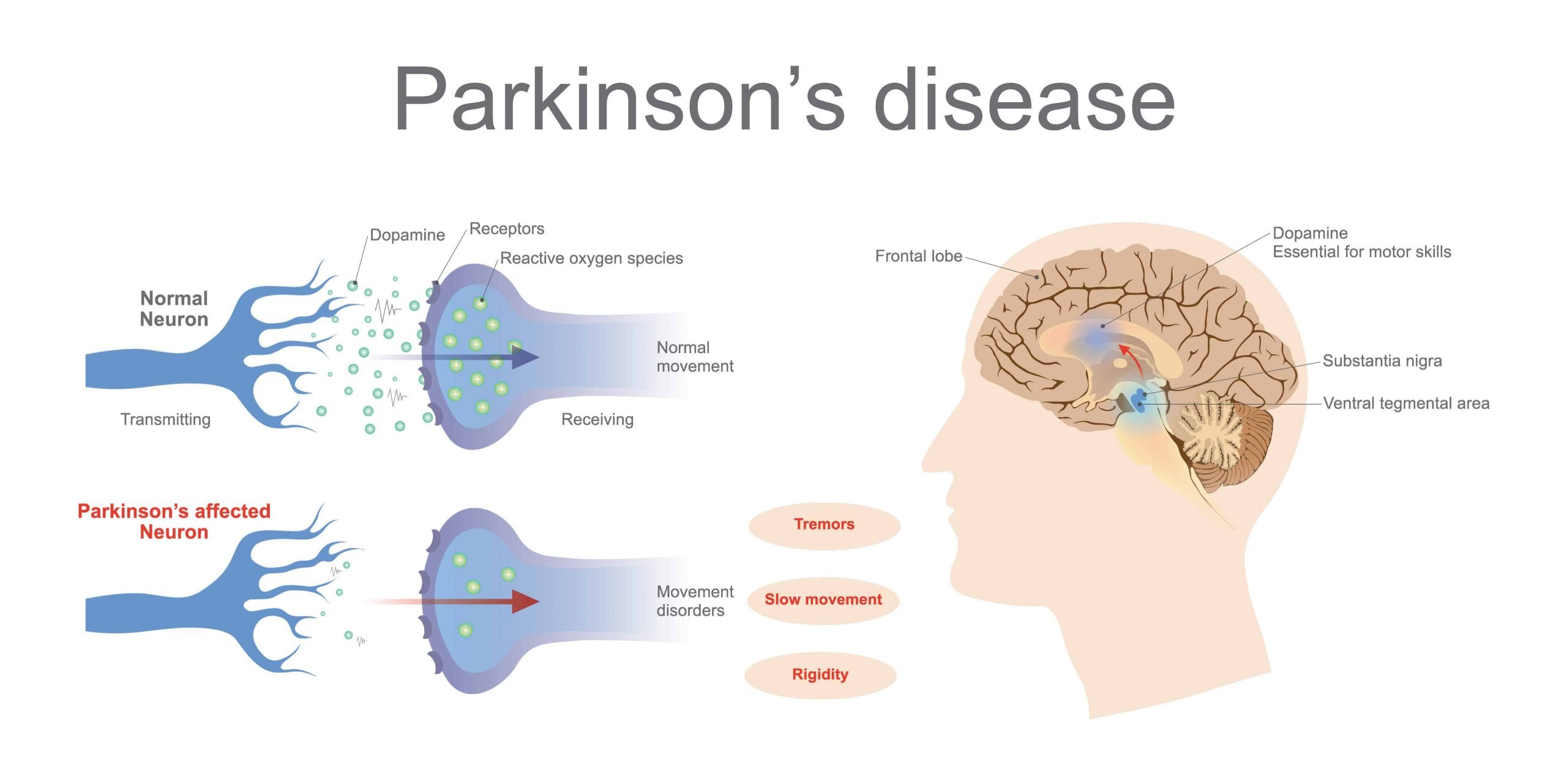
The dopamine in your brain is heavily involved in controlling the movement of your body. In Parkinsons, there are reduced levels of dopamine. For this reason the most obvious changes related to Parkinsons are normally those that affect your movement, including walking, falling and freezing.
In particular, slowed movement, stiff muscles and changes to posture affect all people living with Parkinsons. These issues and others can lead to challenges with walking, freezing and falling.
Read Also: How Does A Person With Parkinson’s Feel
How Are Speech Problems Treated
There are many options to help improve your speech. A speech-language pathologist can help you pick the right approaches for you. Speech-language pathologists are trained health care professionals who specialize in evaluating and treating people with speech, swallowing, voice, and language problems.
Ask your doctor for a referral to a speech-language pathologist. It is also important to contact your health insurance company to find out what therapy and procedures are eligible for reimbursement and to find a list of SLPs covered by your plan. Finally, visit a SLP who has experience treating people with PD.
The Route To Better Walking
The good news for people with PD is that with exercise and physical therapy it is possible to cope better with freezing, turn and walk more normally and improve balance. Through practice and sessions, a physical therapist can help people with PD avoid tripping by helping them learn to take larger steps. Additionally, joining an exercise class tailored to people with PD can help. If you take levodopa, be sure to exercise while it is working the drug helps your body learn and remember motor skills.
Tricks that can help overcome freezing:
- Walk to a regular beat to help prevent freezing. Try a metronome.
- Take large, voluntary marching steps.
- Step over an imaginary line or laser pointer.
- Work with a therapist to find the solution that works best for you.
People respond differently to audio, visual or sensory cues. Dr. Horak and her team are testing a device that provides sensory feedback vibration on the foot to stimulate automatic stepping.
Another consideration for people who have freezing is anxiety, a common PD symptom. People who have anxiety experience freezing more often. It is a vicious circle being anxious about freezing can trigger it. Treating anxiety may help freezing.
Also Check: When To Start Levodopa Therapy For Parkinson’s Disease
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinsons disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable reducing symptoms during on periods and no longer controlling symptoms during off periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they cant. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Makes Pd Hard To Predict
Parkinsonâs comes with two main buckets of possible symptoms. One affects your ability to move and leads to motor issues like tremors and rigid muscles. The other bucket has non-motor symptoms, like pain, loss of smell, and dementia.
You may not get all the symptoms. And you canât predict how bad theyâll be, or how fast theyâll get worse. One person may have slight tremors but severe dementia. Another might have major tremors but no issues with thinking or memory. And someone else may have severe symptoms all around.
On top of that, the drugs that treat Parkinsonâs work better for some people than others. All that adds up to a disease thatâs very hard to predict.
You May Like: Is Parkinson’s Disease An Autoimmune Disease
Production Of Dopamine Neurons From Stem Cells: Could We Be One Step Closer To The Cure
As the disease progresses, people may experience reduced quality of life, if normal functions such as swallowing, start to be affected. Currently, there is no known cure for Parkinsons disease. Once Parkinsons is diagnosed, the symptoms can often be treated with medications and therapies, especially in the early stages. However, the scientific community is making every effort to find a way to cure or at the very least find more effective ways to lessen the symptoms of this physically impairing disease.
As we mentioned before, the disease primarily affects dopamine-producing brain cells or neurons. The good news is, scientists in Sweden have identified some insights and a set of markers that should help control the quality of stem cells engineered for clinical use to treat Parkinsons disease. As the disease progresses and dopamine-producing brain cells malfunction and die, it leads to lower levels of dopamine, which is a chemical messenger essential for controlling movement. These findings should help fine-tune stem cell engineering to produce pure populations of high-quality dopamine neurons. Then, a pool of progenitor cells can be transplanted into the brains of patients, so they can make new supplies of dopamine cells.
But while this exciting new research is still in the lab, what else can we hope for to delay the symptoms of Parkinsons and improve the quality of life of those suffering from the disease?
Reducing The Risk Of Falls
It is important that you take all your Parkinsons medications as prescribed so that symptoms such as poor gait and freezing are well controlled.
Some Parkinsons medications may, unintentionally, lower blood pressure and this can cause dizziness and increase the risk of falling. If this happens you should ask your doctor or nurse to check your blood pressure both when standing and sitting. Your doctor may be able to advise on medication to help with low blood pressure and dizziness, although this can be complicated because of possible interference with Parkinsons medications.
Some dizziness can be avoided. For example, when getting out of bed let your feet dangle over the side of the bed for a few minutes before standing and then rise slowly. When getting up from a chair, pause for a few moments and only start walking when you feel steady.
Some Parkinsons medications can actually aggravate falls by causing dyskinesias;Again, it is important to tell your doctor if you fall so that medication can be adjusted if necessary.
Caution!;
You are more likely to fracture a bone if you fall frequently, particularly if you have osteoporosis. If you fall frequently, ask your doctor for an osteoporosis assessment. If osteoporosis is diagnosed, he or she will be able to give you s advice on minimising its effects or refer you to another professional who can help.
Recommended Reading: What Medications Should Parkinson’s Patients Avoid
Rigidity Results In Biomechanical Impairments
Excessive, inflexible axial postural tone, called rigidity, results in many biomechanical impairments affecting postural control such as abnormally stooped postural alignment, forward head, Pisa syndrome, reduced joint range of motion, and low back pain. Stooped posture, due to excessive, static flexor muscle activity, is associated with increased velocity and jerkiness of postural sway in stance . Automatic postural responses to external displacements are also impaired by a stooped postural alignment. The postural stability margin, which is defined by the difference in displacement of the center of pressure under the feet and displacement of the body CoM in response to external perturbations, is reduced in healthy subjects who assume a stooped posture like PD . This observation suggests that a stooped posture, per se, has a destabilizing effect on postural control and is not an attempt to compensate for postural instability. Responses to backward body perturbations are especially compromised by a stooped posture, perhaps due to a shortening of the tibialis anterior muscle, which is critical for bringing the backward falling body back to equilibrium.
What Is Parkinsonian Gait
Parkinsonian gait is a defining feature of Parkinsons disease, especially in later stages. Its often considered to have a more negative impact on quality of life than other Parkinsons symptoms. People with Parkinsonian gait usually take small, shuffling steps. They might have difficulty picking up their feet.
Parkinsonian gait changes can be episodic or continuous. Episodic changes, such as freezing of gait, can come on suddenly and randomly. Continuous changes are changes in your gait that happen all the time while walking, such as walking more slowly than expected.
Read Also: How Many Forms Of Parkinson’s Are There
Physical Issues Of Your Sex Drive
Parkinsons affects ones autonomic nervous system, which controls sexual response and functioning. Parkinsons acts upon neurons in the brains substantia nigra, causing dopamine-producing nerve cells to die. Since dopamine is a chemical that transmits signals between parts of the brain that usually coordinate smooth muscle movement, this is critical to sexual function on two fronts.
Introducing an easier way to track your symptoms and manage your care.
Dont want to download the app? Use the non-mobile version here.
First, this dopamine drop may result in a decreased sex drive and sexual interest. Second, the lower levels of dopamine that result are believed to cause ones loss of balance, changes in walking pattern and posture, muscle rigidity, Bradykinesia , and tremors when resting. The symptoms of Parkinsons can also be seen in:
Falls And Common Household Hazards
If you or a loved one has Parkinson’s disease, here are tips for preventing falls around the home:
- Floors. Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its accustomed place.
- Bathroom. Install grab bars and nonskid tape in the tub or shower. Use nonskid bath mats on the floor or install wall-to-wall carpeting.
- Lighting. Make sure halls, stairways, and entrances are well lit. Install a night light in your bathroom or hallway. Make sure there is a light switch at the top and bottom of the staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen. Install nonskid rubber mats near the sink and stove. Clean up spills immediately.
- Stairs. Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it may be helpful to arrange most of your activities on the lower level to reduce the number of times stairs must be climbed.
- Entrances and doorways. Install metal handles on the walls adjacent to doorknobs of all doors to make it more secure as you travel through the doorway.
Recommended Reading: How Do Lewy Bodies Cause Parkinson’s
What Is Parkinsons Disease
Parkinsons disease was named after the British doctor James Parkinson, who, in 1817, first described the disorder as shaking palsy. You may be surprised to learn that it is the second most common neurodegenerative disorder in the world. It is most known for the degree of impairment that it causes, most often leading to fall-related issues due to the progressive loss of muscle control that causes trembling of the limbs and head, stiffness, slowness, and impaired balance, making it gradually more difficult to walk, climb stairs, complete simple tasks or even talk.
Most individuals who develop Parkinsons disease are 60 years of age or older, but early-onset Parkinsons disease can occur.
Bradykinesia And Freezing Impair Gait
Dynamic balance control involves controlling the body CoM with respect to, but not necessarily over a moving base of support. Walking becomes less automatic in PD so it requires more attention, particularly for challenging tasks such as turning, walking between obstacles, and dual-tasking. Newly diagnosed patients with PD show signs of bradykinetic gait features, such as reduced trunk rotation, decreased arm swing, and slow turns, even when walking speed is normal . Extent of arm swing on the most involved side may, in fact, be the most sensitive early sign of gait affected by the disease. Bradykinesia results in slow gait velocity and shuffling of the feet that progresses with the disease. Freezing of gait is not usually only lack of stepping but often includes high frequency trembling of the legs as the patients attempt to get their feet moving. These quick motions may represent repeated, multiple APAs that get larger and larger until a step is finally triggered .
Also Check: What Is The Difference Between Parkinson’s Disease And Alzheimer’s Disease

