How Will The Person With Advanced Pd Experience Death
The journey for every person with PD will be different. Their symptoms, disease progression, access to medical care, and their concurrent medical issues may vary widely and play a role in their life and their death with PD. As described above, the person with advanced PD typically dies from an event that occurs on top of the increasing levels of frailty and disability that build up over time. That event may be a fall, an infection, a choking event, or another medical issue that leads to a hospitalization and causes a more precipitous decline.
Regardless of the cause, when a neurologist assesses that the possibility of death within a particular time frame is likely, hospice care can be initiated. This is different from palliative care, which is a clinical approach that focuses on improving quality of life for people with complex diseases. Palliative care can begin at any point during the disease progression and work in conjunction with the treatment plan. Hospice care, on the other hand, is provided to improve the quality of life when end of life is near.
In summary, while it is true that PD in and of itself is not fatal in the same way that a rupture of a brain aneurysm or a massive heart attack may be , the disability caused by PD can contribute to death in a variety of ways as outlined above. Educating yourself on the various possibilities and areas of concern may help you better prepare for the future, minimize some risks, and possibly enhance or prolong quality of life.
Starting Palliative Care In Patients With Pd
Patients with PD benefit early from palliative care in view of the impact of the disease impairing autonomy and quality of life. The provision of palliative care in patients with PD focuses on unmet needs and should be aligned with patient priorities. It is recommended that a palliative care approach should be applied from the early phase, throughout the course of the disease, complementing but not replacing other treatments . However, like other patients with chronic neurological condition, the individual needs may vary over time, therefore it is suggested that a model of dynamic involvement of palliative care services should be adopted . The services can be triggered at times of particular symptoms or psychosocial issuessuch as the start of new interventions or at the very end of life.
For patients with complex physical, social, psychological and/or spiritual needs that do not respond to simple or established protocols of palliative care, there should be access to the support from specialist palliative care service .
However, rate of use of hospice in PD patients has been low . Caregivers often considered palliative care services to be synonymous with hospice care, and hence they did not consider this service option . Health care workers also have uncertainty about timing of palliative care, such that it was often not introduced until a crisis point .
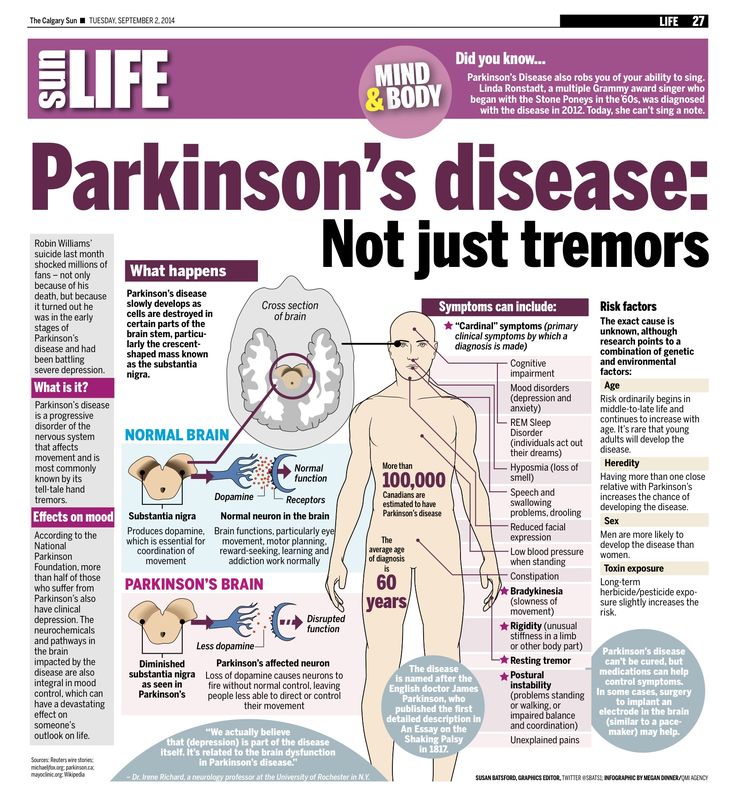
What Are The Five Stages Of Parkinson’s Disease
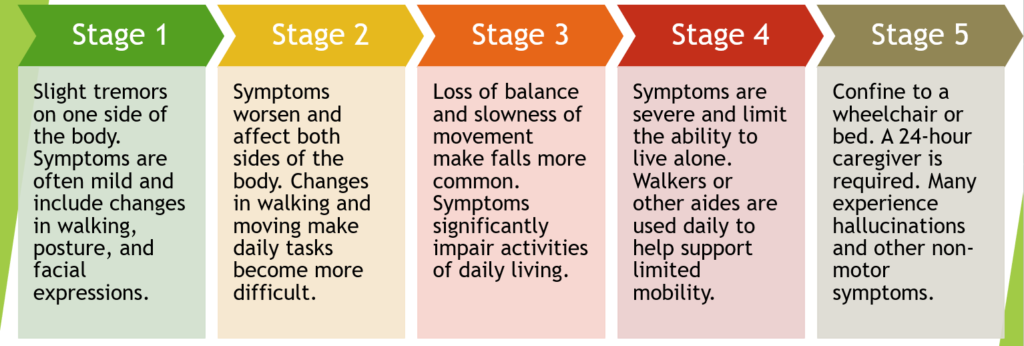
Parkinsons disease is a progressive nervous system condition that impacts movement. Due to the diversity of the disease, the nature and severity of symptoms are often a bit different from person to person, and not all people who have Parkinsons will experience every symptom. Parkinsons patients experience progression at different speeds.
Doctors have established stages that describe how the disease progresses, even though Parkinsons patients wont necessarily experience them in the same order or at the same intensity. There are, however, typical patterns of progression in Parkinsons disease. These five stages of Parkinson’s are used by medical staff throughout the world to classify patients and can help people affected by Parkinsons cope with changes as they occur.
Recommended Reading: Animal Models Of Parkinson’s Disease
Stage 3 Of Parkinsons Disease
Stage 3 is considered the mid-point of Parkinsons disease and includes a loss of balance and coordination. Your reflexes become slower, and falls are more common in this stage. Many of the symptoms from stage 2 are present here, and daily activities such as getting dressed, eating, and getting out of bed become more and more difficult. It is important to note that patients in stage 3 can still live independently.
Stratification For Therapeutic Outcomes
Based on the increasingly recognized heterogeneity of PDnot only in terms of underlying genetic and/or environmental causes, but also in terms of clinical presentationsthere is an emerging need for better definitions of subtypes of PD that allow to assign treatments and shape therapeutic approaches according to the best response. As there is still no established neuroprotective treatment option that is able to intervene with the chronic neurodegenerative process, most benefit for the patients in terms of quality of life can be currently achieved by providing access to best symptomatic treatment. This is also reflected by the fact that clinical trials focus on more meaningful parameters in terms of primary and secondary outcomes . Complications of symptomatic pharmacological treatment of PD like dyskinesia remain a significant problem and several recent trials failed to efficiently target dyskinesia at phase III level . Therefore, the translation of novel drugs into successful trials requires the definition of clinically important change that goes beyond the application of clinical rating scales and aligns with the patients observation, e.g., of remission and perception of dyskinesia.
Recommended Reading: Does Vitamin B12 Help Parkinson’s
New Treatment Targets In Advanced Parkinsons Disease
A good example is the concept supported by mPower: a relative simple smartphone-app assesses with short questions or easy motor tasks a complex pattern of features for each patient. Since it is easy to download and install, already over 9.500 patients have registered and include their data . The implementation of novel technologies ultimately has the potential to provide patterns of symptoms extracted from real-life patient scenarios and allows for a more direct and active participation of patients to research programmes, which might improve their quality of life . Today a great number of different technologies for domestic monitoring of motor symptoms do exist, ranging from wearable sensors to non-wearable devices or gait labs . Non-motor symptoms like sleep quality, skin humidity or cardiovascular function can also be monitored, but still need development to improve practicability and consequently adherence of the patient to the device-based assessment .
Relationship Between Parkinsons Disease And Mortality
Multiple studies have investigated the connection between PD and mortality. Results are not consistent across studies, and some conclude that PD does not increase mortality over the general population. Other studies conclude that people with PD have a mortality ratio of about 1.5 as compared with the general population. This means that the rate of observed deaths among all people with PD is about 1.5 times higher than would be expected in the general population.
However, even studies that conclude that PD overall does not confer an increase in mortality over the general population, find that people with PD who have certain characteristics are at an increased risk of dying. These characteristics are associated with advanced PD and include:
- Longer duration of disease
- Presence of comorbid medical conditions
Recommended Reading: Does Bill Clinton Have Parkinsons
Stage Three Of Parkinsons Disease
Stage three is considered mid-stage and is characterized by loss of balance and slowness of movement.
Balance is compromised by the inability to make the rapid, automatic and involuntary adjustments necessary to prevent falling, and falls are common at this stage. All other symptoms of PD are also present at this stage, and generally diagnosis is not in doubt at stage three.
Often a physician will diagnose impairments in reflexes at this stage by standing behind the patient and gently pulling the shoulders to determine if the patient has trouble maintaining balance and falls backward . An important clarifying factor of stage three is that the patient is still fully independent in their daily living activities, such as dressing, hygiene, and eating.
Stage 1 Of Parkinsons Disease
This beginning stage of Parkinsons disease has minimal symptoms, if any at all. If symptoms are present, they may include tremors and affect one side of the body. For example, one side of the face may be affected, or one hand or leg may feel slower than the other. Your family and friends may notice changes in your posture or facial expressions. Any symptoms that are present arent severe enough to interfere with daily activities. Diagnosis is difficult at this stage, and the affected person may not even seek medical attention at this point.
Don’t Miss: How Is Parkinson Disease Diagnosed And Treated
Another Tool For Tracking Parkinsons Progression
Some neurologists also use the Unified Parkinsons Disease Rating Scale to track the symptoms of Parkinsons. The UPDRS is a more extensive tool that also checks nonmotor symptoms, such as:
- Mental function
- Lightheadedness upon standing
- Fatigue
Members of MyParkinsonsTeam have discussed a wide range of experiences when it comes to how their condition progresses. I was diagnosed with PD in 2003, and my symptoms did not advance significantly until 2019, one member wrote. Another said, My PD has advanced slowly and I feel pretty good most of the time.
What Are The Stages Of Parkinson’s Disease
Parkinsons disease is a neurodegenerative disorder that causes difficulty with walking and coordination. It occurs when the brain can no longer produce enough dopamine, one type of chemical in the brain. A progressive disease, Parkinson’s starts gradually and gets worse with time.
The most common symptoms of Parkinson’s disease are stiffness in different parts of the body, shaking , difficulty with balance and coordination, difficulty walking and slow movements. As the disease advances, muscle pain and cramps, problems with sleep, memory impairment, depression, and behavioral changes may set in, too.
The Hoehn and Yahr scale is used to stage Parkinsons disease according to the order in which symptoms appear and gradually worsen. There were previously five stages in the Hoehn and Yahr scale, but over time it was modifiedstages 1.5 and 2.5 were added to it.
Read Also: What Is The Difference Between Lewy Body Dementia And Parkinson’s
Getting Care At Any Stage
Although the different scales are meant to measure the progression of Parkinsons disease and the response to medication and treatment, some patients may never progress to stage 5, and not everyone with Parkinsons will spend the same amount of time in each stage. Some people are diagnosed with Parkinsons when they are young and remain in the early stages for several years. Others may skip stages, or their progression to end-stage Parkinsons may be more rapid. It is also possible to experience symptoms like tremors but not have any balance issues.
No matter where you are in your Parkinsons journeywhether youre at stage 1 or stage 5know that youre alone. At PLM, there is a community of over 30,000 Parkinsons patients who know what youre going through. Join the conversation to connect with others who are like you and can support you through your illness.
Signs Of Parkinsons Disease
In 1817, Dr. James Parkinson published An Essay on the Shaking Palsy describing non-motor, as well as, motor symptoms of the illness that bears his name. Parkinsons is not just a movement disorder, explained Dr. Shprecher. Constipation, impaired sense of smell, and dream enactment can occur years before motor symptoms of Parkinsons. The latter, caused by a condition called REM sleep behavior disorder, is a very strong risk factor for both Parkinsons and dementia . This has prompted us to join a consortium of centers studying REM sleep behavior disorder.
Also Check: Can You Get Rid Of Parkinson Disease
Causes Of Parkinsons Disease
Parkinsons disease is caused by a loss of nerve cells in part of the brain called the substantia nigra. This leads to a reduction in a chemical called dopamine in the brain.
Dopamine plays a vital role in regulating the movement of the body. A reduction in dopamine is responsible for many of the symptoms of Parkinsons disease.
Exactly what causes the loss of nerve cells is unclear. Most experts think that a combination of genetic and environmental factors is responsible.
-
Offer modified foods that are easy to digest.
-
Allow more time for eating and never rush your loved one.
-
Offer high protein supplements such as protein shakes.
-
Try offering popsicles if liquids are being refused.
-
Keep your loved ones mouth and lips moist to aid in comfort.
-
As hard as it is, be patient and understanding that this is part of the natural death and dying process.
Myth : Parkinsons Disease Is Fatal
Fact: Although a diagnosis of Parkinsons is devastating, it is not as some people may still believe a death sentence. Parkinsons disease is not a direct killer, like stroke or heart attack. That said, much depends on the quality of your care, both from your medical team and yourself.
As the disease progresses, you may become more vulnerable to falls, which can be dangerous. Thats why exercise and physical therapy are so important.
Infection is another problem. In later stages of Parkinsons, people often miss those signals and may not notice somethings up until its too late. That can be, literally, a killer so be sure to stay up to date with checkups.
Read Also: Sam Waterston Parkinsons
Also Check: What Age Does Parkinson’s Usually Start
Parkinsons Disease Life Expectancy
Most people with Parkinsons can have a normalor close to normallife expectancy today, thanks to new medications, therapies, and other treatments. Survival rates for those with typical Parkinsons disease are either the same as for the general population or shortened by about a year, studies show.
Risk factors for earlier mortality with Parkinsons include:
-
Being diagnosed before age 70
-
Having cognitive impairment early in the disease
-
Developing Parkinsons dementia
People with Parkinsons dont die from the disease itself, but from associated complications, such as infections or injuries . Cardiovascular disease is another common cause of death.
Treatments and lifestyle improvements, can help forestall cognitive decline, lower your risk of falls and strengthen your cardiovascular system. These can help improve your quality of life and, by slowing progression of the illness, potentially keep you living longer.
Researchers are continuing to explore new treatments that they hope will one day lead to better therapies for Parkinsons, which will result in an improved prognosis.
First Signs Of Impaired Righting Reflexes This Is Evident As The Patient Turns Or Is Demonstrated When He Or She Is Pushed From Standing Equilibrium With The Feet Together And Eyes Closed
Loss of balance, with the inability to make the rapid, automatic and involuntary movements necessary to protect against falling, is one of the most troubling and dangerous aspects of Parkinsonism and one of the least easily treated. Even when manifested by only slight unsteadiness, it is the criterion separating Stage II and Stage III. All other aspects of Parkinsonism are evident and usually diagnosis is not in doubt.
However, the most important factor identifying Stage III is that the patient is still fully independent in all activities of daily living Although somewhat restricted, has work potential depending upon the type of employment. A normal life can be.
Recommended Reading: How To Diagnose Parkinson’s Disease Symptoms
How Is It Diagnosed
Diagnosing Parkinson’s disease is mostly a clinical process, meaning it relies heavily on a healthcare provider examining your symptoms, asking you questions and reviewing your medical history. Some diagnostic and lab tests are possible, but these are usually needed to rule out other conditions or certain causes. However, most lab tests aren’t necessary unless you don’t respond to treatment for Parkinson’s disease, which can indicate you have another condition.
When Is It Time For Hospice Care
Even though the course of Parkinsons is predictable, the end stage of Parkinsons is not. Despite its severity, people dont pass on from Parkinsons rather, the disease leaves patients vulnerable to injury or infection which, in their weakened conditions, often proves to be fatal.
Consequently, knowing when to call hospice is not a simple matter of tracking symptoms. Physicians should always be consulted if patients are experiencing:
- Persistent pain
- Systolic blood pressure below 90
- Frequent falls or poor balance
- Recurrent infections
- Constant nausea
Once a doctor has given the patient a six-month prognosis, a hospice team can be called in. Patients can receive hospice wherever they call homeresidential care facilities, retirement communities or wherever theyve been residing.
Hospice serves both patients and families alike. It also gives patients a chance to spend their final weeks or months free from pain, while lifting a huge burden from families.
Hospice teams provide comfort care to patients. Comfort care provides relief from pain, nausea, and shortness of breath. Working closely with the patients doctor, the hospice team creates a personal care plan to manage symptoms. Nurses check in regularly to adjust pain medication. Home Health aides tend to the patients hygiene. Case managers secure high-grade equipment, such as hospital beds or oxygen machines.
You May Like: How I Cured My Parkinson’s
Interacting With Parkinsons Disease
Here are a few simple, but effective strategies to employ when faced with understandably uncomfortable scenarios:
- Change the subject. When symptoms manifest, sometimes talking about something else can help calm patients down. Whether its a recollection from their past or just a different topic, changing the conversation can turn chaos into calm.
- Take it outside. Fresh air and sunlight can help improve oxygen flow and trigger mood stabilizers in the brain.
- Get busy. Having an activity, especially something patients find meaningful, can help set them on a more even keel. Old hobbies or household tasks generally work best in these instances.
- Have a snack. Most of us get cranky when were hungry or thirsty patients with Parkinsons are no different. A light snack, some water or juice can help stabilize behaviors.
- Adjust the ambience. Sometimes, something as simple as a rooms brightness or temperature can contribute to a patients acting out. Too much noise can overstimulate too little light can cause anxiety excessive heat or cold can trigger anger. Adjusting lighting and temperatures, turning the volume down on the TV or the radio, or simply offering a cozy blanket may help restore the peace.
- Ask for help. Looping in a patients doctor may reveal underlying medical conditions, like urinary tract infections, behind the sudden shifts in behavior.
