How Do I Know If I’m Freezing
If you feel like your feet are glued to the ground and prevent you from walking, you are probably experiencing freezing. The first signs of freezing can also be a hesitation to start walking rather than a full blocking.
Freezing is not the same as off periods, which are a decrease in medication efficacy. During these periods, people are incapable of moving and all movements are blocked, even in the upper body. On the other hand, freezing only affects gait.
Freezing episodes are disturbing and sometimes anxiety-inducing. These episodes should not cause you to reduce your activities or avoid situations that give you pleasure. There are several strategies you can implement to help you continue your daily routine.
During freezing periods:
Perform the chosen strategy by choosing which foot you will continue walking with
Visual strategies
Look at an object on the ground and imagine yourself trying to get over it by exaggerating the motion.
- Use lines on the ground, or imagine lines on the ground, as a target for your next step.
- Stick a piece of tape on the ground in locations where you tend to freeze.
- Start by imagining big steps, then attempt to take these big steps.
- Use the light of a laser as a target to guide your next step.
Auditory strategies
Use rhythms to help you initiate your steps or maintain your pace.
- Clap your hands to the beat of a song you like.
- Sing or whistle to create a rhythm.
- Give yourself commands out loud .
- Take steps to the rhythm of a song or metronome.
About Dr Sarah King Pt Dpt
Sarah is a passionate Parkinsons advocate who founded Invigorate Physical Therapy & Wellness, an online wellness practice 100% specialized in Parkinsons disease, to help her clients get out of overwhelm and into action by connecting them with the tools and support they need to thrive over the course of their Parkinsons journey. She lives in Austin, Texas with her husband , Matt.
Sarah will also be joining us for the Victory Summit® event in Austin, TX on Saturday, April 13, 2019. If youd like to join us and meet Sarah in person, you can register for this free event here.
Strategies To Combat Freezing In Parkinsons Patients
Freezing is when an individual suddenly feels like theyre glued to the ground. Parkinsons disease patients often experience freezing during the late stages of the disease. It can occur while the person is in motion or after theyve been stationary and then attempt to move. Its associated with complicated movements like dodging obstacles or getting up from a chair.
The loss of automatic motor skills affects ones sense of control and even their safety, as about 38 percent of Parkinsons patients fall each year. Tracking when your struggles occur can help you to manage them, allowing you to challenge how frequently freezing occurs.
Read Also: What Are Early Warning Signs Of Parkinson’s Disease
Electrophysiological Signal Recording And Analysis
The subthalamic LFP recordings were combined with measures of the cortical electrophysiological activity using a 64-channel portable EEG . EEG signals were acquired with the sampling frequency at 1000 Hz and resampled at 400 Hz to match the STN LFP sampling frequency and optimize signals alignment for connectivity analyses. Low frequency and high frequency were eliminated using a bandpass Kaiser windowed FIR filter . Power line noise was eliminated using a bandstop fourth order Butterworth filter. EEG channels affected by bad scalp-electrode were visually identified and replaced with spherical spline interpolation. Stereotypical artefacts were removed by independent component analysis . Laplacian montage was applied to reduce muscular artefacts . We ruled out the effect of movement artefacts by comparing the wavelet transformation of epochs of walking with epochs of gait freezing, focusing on the 13 Hz band. In this frequency band, the epochs of walking and gait freezing showed similar spectral profiles, thus further excluding a confounding effect due to movement artefacts.
We first computed the power in the specific and -frequency bands of the two STN and compared it between walking and the abovementioned time frames of gait freezing.
Read Also: How To Tell Difference Between Parkinsons And Essential Tremor
The 5s Method Consists Of The Following 5 Sequential Steps:

If you are a Thrive patient, be sure to ask your therapist for your 5S magnet if you dont already have one.
Also Check: Early Symptoms Of Parkinson’s Disease
Ways To Reduce Parkinsons Freezing Of Gait
Do you sometimes feel like your feet are stuck to the floor or your hips are glued to your chair, despite your best efforts to move them?
This symptom, called freezing, has been seen in 30-67% of people diagnosed with Parkinsons, with a higher rate of incidence in later stages.
While everyone has unique freezing patterns, some common triggers include: turning in tight spaces, walking through doorways, walking in narrow hallways or crowded places or changing walking surfaces .
As soon as you notice freezing symptoms creeping up on you, its important to address them so you can prevent them from worsening over time.
The first line of treatment is often dopaminergic medications that aim to keep you in an ON state for longer. However, evidence suggests there is a cognitive component of freezing that medication and deep brain stimulation do not address effectively.
This is why the best long-term treatment option for Parkinsons freezing is non-pharmaceutical, non-invasive and focuses on retraining your brain for success.
Here are six actions you can take to help minimize your freezing of gait.
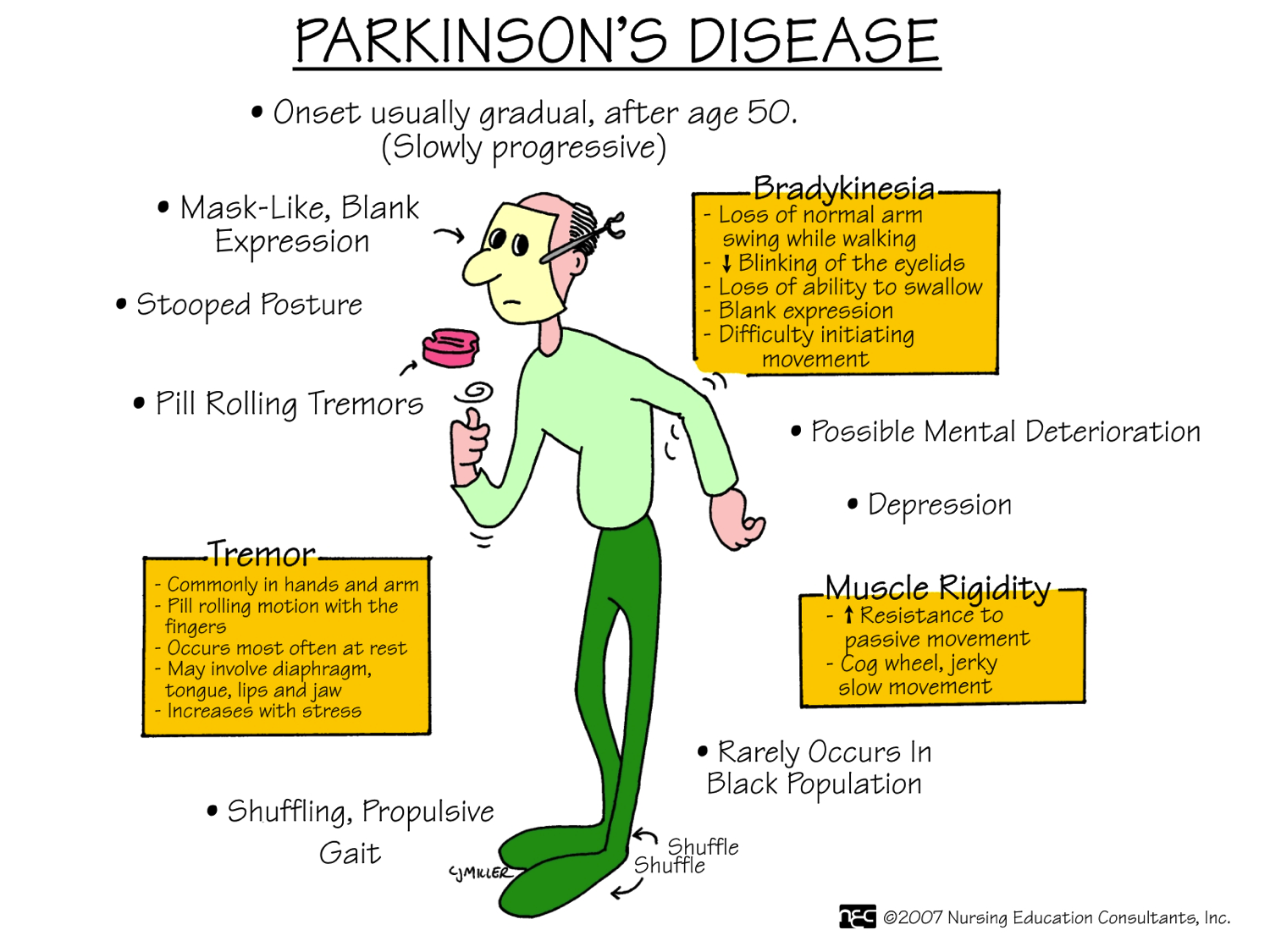
The Symptoms Of Parkinsons Disease
Parkinsons Disease is a neurodegenerative disease, which means the symptoms can get worse over time. PD is also a very complex disease with both motor and non-motor symptoms, and the symptoms present differently in every individual. The most common symptoms of Parkinsons are discussed below. It is important to note that individuals with PD may not experience all of these symptoms, and symptoms will progress at a different rates in different people.
Also Check: Dementia Vs Parkinsons Disease
Read Also: Parkinson’s Color Ribbon
Subthalamic Oscillatory Activity And Connectivity During Gait Freezing
To investigate the role of the STN neural activity in gait freezing we compared the STN oscillations between walking and ongoing freezing episodes. We first studied power changes in low frequency and in the -frequency band of the two STN and did not find any differences during gait freezing in comparison to walking . We also assessed the duration of -burst and did not find a difference between walking and gait freezing . We finally investigated the subthalamic interhemispheric coupling in the -band and showed an increase of -coupling followed by a reduction in the synchronization between the two STN during gait freezing. However, this change did not reach statistical significance .
The Symptoms Of Parkinson’s Disease
Parkinsons Disease is a neurodegenerative disease, which means the symptoms can get worse over time. PD is also a very complex disease with both motor and non-motor symptoms, and the symptoms present differently in every individual. The most common symptoms of Parkinsons are discussed below. It is important to note that individuals with PD may not experience all of these symptoms, and symptoms will progress at a different rates in different people.
Recommended Reading: What Are Early Warning Signs Of Parkinson’s Disease
Why Do People With Parkinsons Freeze
Some people are more prone to freezing than others. It tends to occur with increased frequency as Parkinsons progresses and appears to be linked to long-term use of levodopa. It can be experienced by people who do not take levodopa, so it is not simply a side effect of medication.
Whatever the cause, not everyone with Parkinsons will experience freezing and it is impossible to accurately predict those who will. Freezing seems to be more prevalent in those whose initial symptoms included gait problems, and less prevalent in people who initially present with tremor.
The exact cause of freezing is unclear, but it is thought to occur when there is an interruption to a familiar or automatic sequence of movements. During walking, freezing is mainly observed when:
- you are walking towards doorways, chairs or around obstacles
- you are turning or changing direction, especially in a small space
- you are distracted by another task when you are walking
- you are in places that are crowded, cluttered or have highly patterned flooring
- the flow of your walking is interrupted by an object, by someone talking, or if you begin to concentrate on something else. All of these will stop you from being able to keep a rhythm going
- your medication is wearing off and no longer controlling symptoms as well
- youre in a group situation or in conversation.
Coping With Freezing In Parkinson’s Disease
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Around half of people who have Parkinson’s disease experience freezinga temporary inability to move that occurs suddenly and without warning. Such episodes are short-lived, lasting from a few seconds to up to several minutes.
Parkinson’s freezing can affect nearly any part of the body and disrupt nearly any activitychewing for example, or writing. However, it most often occurs when someone is walking, causing them to feel as if their feet are glued to the ground even though the upper part of their body is still mobile. This sometimes is referred to as freezing of gait and can have repercussions ranging from a brief disruption in stride to an increased risk of falling that can lead to broken bones and other injuries.
The exact physiological cause of freezing in Parkinson’s has yet to be determined. What is known is that it’s often associated with lulls in the effectiveness of medication, particularly among people who have mid-to-late stage disease. There also are a number of common triggers of freezing while walking, such as changing direction, approaching a doorway, or navigating a crowded area. Although Parkinson’s freezing can have a negative impact on a person’s quality of life, there are simple and effective ways to manage it.
Read Also: Can Parkinson’s Run In The Family
Treating Freezing Of Gait For People With Parkinsons
Freezing of gait episodes often occur when a person is under-medicated and can improve with increased amounts of their PD meds, usually carbidopa/levodopa. However, as mentioned earlier, the brain abnormalities that lead to freezing of gait are very complex, so giving more dopaminergic medication is only part of the solution. In fact, some people have what is referred to as ON freezing. This means that freezing of gait episodes occur even when other PD symptoms are well treated with their medication regimen.
Cueing, or the introduction of an external sensory stimulus to facilitate movement, has been identified as a way to break a freezing episode. Terry Ellis, PhD, PT, NCS, Director of the APDA National Rehabilitation Resource Center at Boston University, and Tami DeAngelis, PT, GCS, compiled this list of cues that can be used to get out of a freezing episode:
Probing Significant Interactions In Amplitude Synchronization
In order to distinguish significant from non-significant interactions between signals j1 and j2, we study how their amplitude-phase synchronization index R decays when shifting the signals against each other. Panels and in Fig. show examples of R versus the time shift and suggest that more synchronized signals have a marked decay of R ) that may not be seen for less synchronized signals ). To quantify this observation, we define a significance value W that normalizes the maximum phase synchronization index \ by the background noise characterized by the mean and standard deviation of R. Colloquially, W gives an estimate of how much \ stands out from the noise background. It can be defined by
Dont Miss: Micrographia In Parkinsons Disease
Also Check: What Are Early Warning Signs Of Parkinson’s Disease
So What Can You Do To Manage Freezing
- If you find yourself getting stuck in particular places, try changing the layout of your living space. Freezing can occur because you have to pivot around furniture.
- Exploring rhythm helps you to maintain momentum where you previously got stuck. Some Parkinsons patients explore strategies like dancing, counting, marching, and shifting their weight from side to side.
Thinking outside of the box can assist you in unfreezing yourself. Dad finds that his posture can affect whether or not hes able to unfreeze himself: When I freeze, I stand up straight. If I move away from gravity, I can unfreeze. But if Im hunching over, gravity pulls me toward the floor and it takes longer to get out of the freeze. And once I move my left foot forward, I can unfreeze. Freezings scary. Thats why a lot of Parkinsons patients fall.
Techniques To Overcome Freezing
Physical therapy and occupational therapy can be helpful to reduce or overcome freezing episodes. Physical therapy focuses on the physical rehabilitation of people recovering from injuries or disease with the goal of restoring mobility, as well as educating patients on managing their condition to maintain long-term benefits. Occupational therapy also deals with rehabilitation and motion but is focused more on enabling the person to engage in daily activities as seamlessly as possible. Occupational therapists also suggest adaptations and modifications to the persons environment.3
There are several techniques that can help people with PD overcome freezing, including:
As with any symptom, patients who experience freezing episodes should mention this to their neurologist who is managing their care. The neurologist may make changes to medication or provide a referral to a physical or occupational therapist.
Don’t Miss: What Is The Life Expectancy Of Someone With Parkinson’s Disease
Rhythmical Or Auditory Cues
- A steady beat from a metronome or suitable music can help. The rhythm should be a comfortable pace, the beat prompting you to lift your feet and step.
- Develop a trigger word such as go, step or march to re-start your walking.
- Try closing your eyes to take the first step, making sure it is safe to do so, then open your eyes to continue walking.
- Hum a tune or download music with a good beat onto an MP3 player to keep your walking pattern going. Remember though that you should not use your MP3 in busy places where you should listen for traffic.
- The cue timing can be varied according to where you are, for example you will probably walk faster when outside, and slower in your home. See our video – Coping Strategies: overcoming freezing by counting 1 and our video – Overcoming freezing by counting 2.
- A physiotherapist or occupational therapist may be able to advise on mini metronomes or similar devices that can be clipped onto clothing so can be taken with you anywhere.
Attentional strategies use your imagination
The weight shift method
Start hesitation
Touch
- Touching a particular part of the body can also sometimes be helpful as a cue to unblock freezing see our video: Coping Strategies: using touch as a cue.
Tips To Get Moving Again
When you get stuck, these tricks from the National Parkinson Foundation can help:
- Be aware of freezing triggers and prepare strategies in advance.
- Shift the weight of your body from one leg to another.
- Listen to music and step with the rhythm.
- Hum, sing, or count.
- Imagine a line to step over or focus on a target on the floor to step on.
- Use a mobile laser device to create a line in front of you to step over.
- Turn by walking half a circle instead of by a pivot turn.
You May Like: Parkinson’s Disease Life Span
Walking Freezing And Falling
The dopamine in your brain is heavily involved in controlling the movement of your body. In Parkinsons, there are reduced levels of dopamine. For this reason the most obvious changes related to Parkinsons are normally those that affect your movement, including walking, falling and freezing.
In particular, slowed movement, stiff muscles and changes to posture affect all people living with Parkinsons. These issues and others can lead to challenges with walking, freezing and falling.
How Does Anxiety Cause Freezing Of Gait
Recently, imaging studies have begun to identify neural correlates associated with freezing behaviour. Although these studies did not focus on inducing anxiety to provoke freezing of gait, it is interesting that decreases in activation were found in the medial prefrontal cortex, left anterior insula and left ventral striatum during motor arrests compared to walking . Although these regions are involved in an array of functions such as the cognitive control network , these areas also have a well-established role in emotional processing . A recent review highlighted that nearly 60% of emotional induction studies reported activation of the insula , and furthermore the insula has been suggested to participate in evaluation of distressing thoughts and interoceptive emotional responses . Imaging results have also shown that Freezers have significantly less BOLD signal in the bilateral anterior insula and bilateral ventral striatum compared to Non-Freezers during simulated walking in virtual reality with increased cognitive load . Taken together, these results align with the current findings and theoretical framework suggesting that dysfunctional processing of emotional information in the ventral striatum might be one explanation of the current results showing that anxiety increased freezing of gait.
Read Also: Symptoms Of Early Parkinsons Disease
